Additional practical Global FAST examples would include cases with right‐sided congestive heart (CHF) and making decisions on whether the patient requires therapeutic abdominocentesis as well as tracking ascites using the AFS for response to CHF therapy; and the use of the AFS postoperatively in vomiting septic abdomen cases to screen for abdominal‐related complications, including effusions and ileus or dehiscence, or thoracic‐related complications such as aspiration pneumonia or myocardial dysfunction, and so forth. The Global FAST approach screens these systems as part of its standardized protocol.
The use of AFAST and AFS in Dehydrated and Hypovolemic Patients
These subsets of veterinary patients often have no ultrasonographically visible free fluid until after they are resuscitated and rehydrated. In the dehydrated patient with a bowel perforation, the omentum is often adhered to the defect, with the resorption (recruitment) of any available free water from the abdominal cavity. Thus, the serious lesion (same for a “small‐volume bleed” from a mass) is not producing substantial free fluid until after rehydration and resuscitation. We use the mantra “Rehydrate, resuscitate, reevaluate with a minimum of at least one additional serial AFAST and AFS” within the next 2–4 hours. In humans with possible bowel injury, serial ultrasound examinations are recommended out to 12‐24 hours post‐admission (Mohammadi and Ghasemi‐Rad 2012) ( Figure 7.9).
Pearl:Serial AFAST exams increase sensitivity in detecting peritonitis and “small‐volume bleed” suspects and should be performed four hours post admission, and again after resuscitation and rehydration. If the patient has not declared itself overtly surgical but remains a candidate, AFAST and AFS should be used serially for at least 12–24 hours and longer if patient status is questionable.
Use of AFAST for Canine Anaphylaxis
Gallbladder Wall Edema – Sonographic Striation
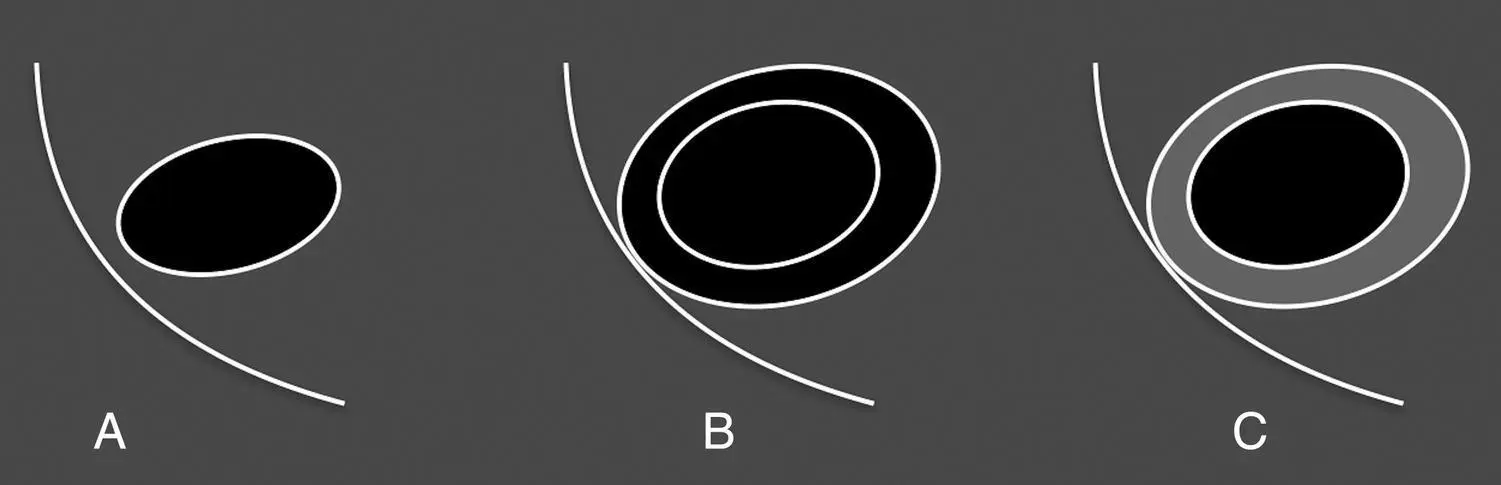
In 2009, the clinical utility of using point‐of‐care ultrasound for the rapid diagnosis of canine anaphylaxis (AX) was shown to be clinically helpful. Since the shock organ in dogs is the liver and gastrointestinal tract, hepatic venous congestion occurs rapidly (experimentally within minutes) due to massive histamine release within the portal circulation (Quantz et al. 2009; Caldwell et al. 2018; Hnatusko et al. 2019). As a result of massive histamine release, the intrahepatic venous sphincters tighten, thus causing the marked acute hepatic venous congestion along with degrees of gallbladder wall edema (intramural edema). The gallbladder change is generally easy to recognize during AFAST because the gallbladder is a fluid‐filled structure and the intramural edema appears as sonographic striation, alternating hyperechoic and anechoic layering, called the “halo effect” or “double rim effect” and more commonly the “gallbladder halo sign” (Quantz et al. 2009) ( Figures 7.10and 7.11). The sonographic striation is observed as an outer hyperechoic line (outer gallbladder wall) and inner hyperechoic line (inner gallbladder wall) with sonolucency (hypoechoic to anechoic) in between. In other words, a layering of white‐black‐white or white‐gray‐white (see Figures 7.10, 7.11, and 18.22).
The gallbladder wall edema is a more rapid (<2–4 minutes) sign of canine AX over traditional markers of liver enzyme elevation such as the alanine transaminase (ALT) level that may peak in as long as 2–4 hours (Quantz et al. 2009). It is important to note that there are additional causes of gallbladder wall edema ( Table 7.5). In the acute setting, conditions that cause obstruction to venous and lymphatic return to the heart that also result in hepatic venous congestion are important rule‐outs and include pericardial effusion/cardiac tamponade and right‐sided congestive heart failure, such as dilated cardiomyopathy, pulmonary hypertension, and tricuspid valvular disease (Lisciandro 2014a,b, 2016a) (see Figure 18.22). In less acute conditions, primary gallbladder diseases (cholecystitis) and diseases that affect the gallbladder such as pancreatitis and cholangiohepatitis can also cause gallbladder wall edema. Other miscellaneous causes include severe hypoalbuminemia and third spacing (d'Anjou and Penninck 2015), immune‐mediated hemolytic anemia, post transfusion, and right‐sided volume overload from overresuscitation from fluid therapy (Nelson et al. 2010).
Rule‐outs are summarized in Table 7.5with speculative pathogenesis and concurrent expected characterization of the caudal vena cava (see next section). The list is important to know to avoid “satisfaction of search error,” the failure to search for additional abnormalities, which is automatically avoided using the Global FAST approach. By failing to rule out these conditions, the patient may be incorrectly resuscitated to its detriment. For example, a canine AX case requires the use of epinephrine and large‐volume fluid resuscitation, which would not be the strategy to resuscitate a case of dilated cardiomyopathy, and emergent pericardiocentesis would be the treatment for pericardial effusion/tamponade, with inotropes for dilated cardiomyopathy.

Figure 7.9. Composite showing comparison of abdominal radiographic serosal detail to AFS and value of serial examinations. (A) Abdominal radiographs of a dog with automobile trauma with markedly reduced serosal detail. The dog has a minimally displaced left acetabular fracture with an unimaged urinary bladder. (B) The initial AFAST determines that the dog has an AFS of 1 positive only at the DH View ( gray circle ). On the four‐hour postadmission AFAST the AFS remains the same. (C) The AFAST on admission is again a 1 which in fact was found with the abdominal radiographs in (A). On serial exam the dog worsened with an AFS of 3. The fluid pocket was large enough to be accessed via abdominocentesis and its fluid analysis documented the large‐volume bleeder hemoabdomen. The dog seemed stable based on physical exam, vital signs, and blood pressure with a normal PCV when in fact the dog was exsanguinating. Over time, the AFS was tracked and the dog received a blood transfusion due to developing anemia. Serial exams may be continued every four hours to every 12–24 hours on patient rounds, depending on clinical course. The serial exam thereafter documenting improvement to an AFS of 1 is invaluable patient information. (D) Images of the initial and four‐hour postadmission serial AFAST showing absence of a urinary bladder and then its expected rounded contour post fluid resuscitation. The urinary bladder was missed initially likely because it was small and caudally located but in critical patients, the serial AFAST may be better used to decide on urinary bladder integrity post resuscitation.
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX. Illustration by Hannah M. Cole, Adkins, TX.
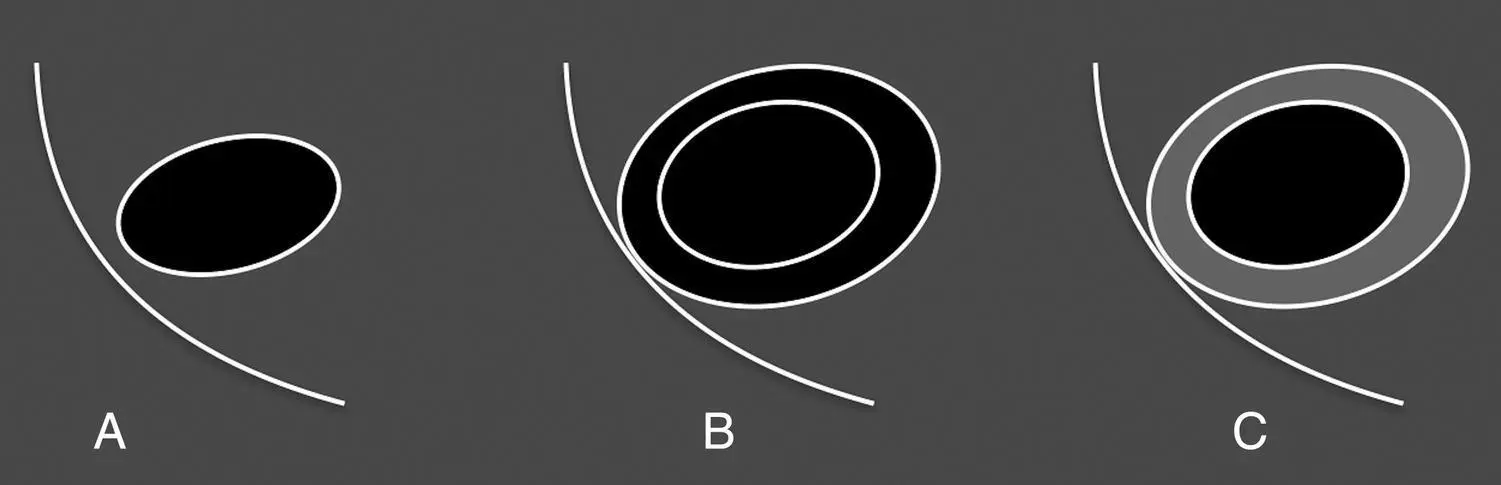
Figure 7.10. Normal and edematous gallbladder wall and sonographic striation. The gallbladder is represented by the black oval and the diaphragm is the white curved line mimicking the DH view. In (A) the gallbladder wall is normal and represented as a hyperechoic (white) thin line. In (B) and (C) the gallbladder has sonographic striation that alternates hyperechoic‐anechoic‐hyperechoic (white‐black‐white) and hyperechoic‐hypoechoic‐hyperechoic (white‐gray‐white). The inner and outer walls are shown as white lines with the intramural edema (black or gray) in between. The gallbladder wall does not have to be of abnormal thickness as dogs with an anaphylactic gallbladder can have sonographic striation with a wall thickness of <3 mm (Lisciandro 2016b) as shown in Figure 7.11B.
Читать дальше