4 No
5 No
Comments: Skin telangiectasias are also seen in patients with ataxia telangiectasia, Crest and Sjogren syndromes. In rosacea, main vascular lesions are the broken vessels that are located exclusively on the skin predominantly on the middle of the face, as in ataxia telangiectasia. In ataxia telangectasia, the vascular lesions are associated with poor coordination, and in Crest syndrome with calcinosis and sclerodactyly and Raynaud phenomenon. Sjogren's syndrome affects the mouth, eyes, nose and other organs causing dryness, swelling of the salivary glands and facial telangiectases.
Q2Which are the main complications of this condition?
1 Anemia
2 Pulmonary hemorrhage
3 Ischemic stroke
4 Skin photosensitivity
5 Mental retardation
Answers:
1 Iron deficiency anemia is a very common complication induced by a series of episodes of blood loss through the nose (epistaxis) and gastrointestinal tract (melena stools) from telangiectic lesions.
2 Pulmonary hemorrhage is mainly found in patients older than 40 years old and with multiple visceral involvements, causing breathing problems, portal hypertension and liver cirrhosis.
3 Ischemic stroke is a rare yet serious complication in patients with HHT, and requires special care.
4 No
5 No
Comments: The vascular lesions on facial skin sometimes cause cosmetic problems, but never skin photosensitivity, while the brain lesions of HHT may cause neuro‐psychiatric complications with various pathways which have not been related to mental illness before.
Which genes are linked with this condition?
1 Endoglin gene (ENG)
2 Fibroblast growth factor receptor 3 (FGFR3)
3 Activin receptor like kinase (ALK‐1)
4 Collagen type I alpha 1 chain(COL1A1)
5 Dentin sialophosphoprotein (DSPP)
Answers:
1 Engoglin gene mutations have been isolated in HHT families (type 1)
2 No
3 Activin receptor like kinase (ALK‐1)mutations have been found in HHT (type 2)
Comments: Mutations in the COL1A1 and COL1A2 genes are related to the development of the majority of osteogenesis imperfecta (>90%), while FGFR3 is associated with fibrous dysplasia and DSPP with dentinogenesis imperfecta.
The following abbreviations are used throughout the book – CO: Complains of; HPC: History of present complaint; PMH: Past medical history; OE: oral examination.

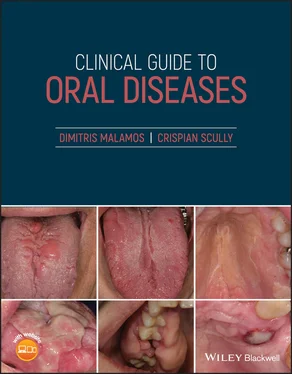
Figure 1.2
CO: A six‐year‐old boy was admitted with bleeding of his mouth.
HPC: The patient sustained a facial injury during a football match half an hour before the bleeding.
PMH: He was a healthy child with no serious medical problems. He was very sociable, and used to take part in all activities at his kindergarten.
OE: He is a very young child, feeling stress and fear because of the bleeding in his mouth, especially from the area of deciduous central right incisor. This tooth had been pushed into its hemorrhagic and swollen gingivae ( Figure 1.2). No other problems with the rest of his teeth, jaws, and oral mucosa were noticed.
Q1What is the possible cause of the hemorrhage of this child?
1 Trauma
2 Self‐induced
3 Infections
4 Children abuse
5 Bleeding disorders
Answers:
1 Facial trauma is commonly noticed among children and characterized by soft tissue injuries (lips, oral mucosae, face) or deep ones into the maxilla or mandibular bone and their associated teeth. Facial trauma is responsible for the “impressive” bleeding due to the high vascularity of this area.
2 No
3 No
4 No
5 No
Comments: The absence of multiple bruises and hematomas alone, or with the different ages of lesions combined with the history of the accident and type of injuries in a child's body is an easy way to exclude bleeding disorders or child abuse from the diagnosis. The absence of fever, swelling and erythema in the lesion rules out infections (bacterial, viral, or fungal). In addition to this, the lack of similar lesions in the past together with the child's good healthy social life reinforces the idea that the lesion was not self‐induced.
Q2Which is/are the difference(s) of facial trauma between children and adolescents?
1 Etiology
2 Bone involvement
3 Symptomatology
4 Complications
5 Recovery rate
Answers:
1 Facial trauma is caused by falling in children and by assault or altercation in adolescents.
2 Fractures of nose bones or jaws are more common in adolescents rather than in children.
3 The symptomatology in children does not fit with the severity of the lesions and is more remarkable than in adolescents.
4 The facial trauma in children is more superficial than in adolescents and their complications seem to be minimal.
5 The younger the children, the easier their recovery.
Q3Which is the clinician's first priority when faced with a patient with facial injury?
1 Calm patient and his parents
2 Retain the airway open
3 Check for broken or dislocated teeth
4 Stop bleeding
5 Treat facial wound (cleaning and suturing)
Answers:
1 No
2 Retaining child's airway open is the first priority as the mucosal edema is disproportional with the patient's airway tract. The clinician should remove obstacles like debris, clots and foreign bodies from the oropharynx, control the location of patient's tongue while in severe cases an orotracheal intubation could be mandatory.
3 No
4 No
5 No
Comments: The second priority for the clinicians is to control bleeding by putting direct pressure on the facial injury. Having bleeding under control, clinicians are then able to properly examine the soft tissue injury, investigate for possible teeth and jaws fractures and then go further to cleanse and suture the wound, as well as reassuring the patient and his parents.

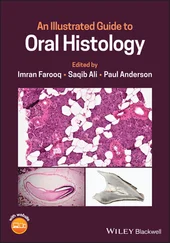
Figure 1.3
CO: A 32‐year‐old woman presented with a soft hemorrhagic lump on her lower left gingivae.
HPC: The lump appeared three months ago and became gradually bigger, covering the whole crown of the second premolar, thus causing eating difficulties and phobias to the patient of being a malignant neoplasm.
PMH: A healthy woman at the third month after baby delivery, with no serious medical problems and drug use apart from iron and calcium tablets prescribed by her gynecologist during her pregnancy. Smoking or drinking habits were plentiful.
OE: A very soft penduculated mass on the gingivae from the distal part of the 1st lower right premolar to the 1st molar. It was very soft, vascular and sensitive, and was bleeding easily with slight probing and caused eating problems ( Figure 1.3). The lesion developed gradually and reaching its biggest site at the last month of pregnancy and began to decrease slowly within the next three months after her delivery. No other similar lesions were found within her mouth, other mucosae or skin. Regional or systemic lymphadenopathy was not recorded.
Q1What is this lesion?
1 Kaposi's sarcoma
2 Pregnancy epulis
Читать дальше