Primary cause of dental plaque‐induced gingivitis
The primary cause of dental plaque‐induced gingivitis is simply poor oral hygiene; the bacterial by‐products (i.e. enzymes and toxins) produced by mature plaque have the potential to directly damage the gingival tissue and also initiate inflammatory and immunological reactions in the tissues.
Secondary causes of dental plaque‐induced gingivitis
Secondary factors increase the risk of the dental plaque, causing disease to the gingival tissues. They can be local (i.e. increasing plaque retention in a specific area), or systemic (whole body) conditions that alter the body’s response to inflammation.
Local factors include:
Malpositioned teeth.
Overhanging fillings.
Ill‐fitting crowns, bridges, or dentures.
Implants.
Orthodontic appliances.
Calculus.
Lip apart posture (mouth breathing). The dryness of the attached gingivae in people whose lips are naturally parted when relaxed increases the likelihood of plaque retention.
Systemic factors include:
Hormone changes during:Pregnancy (pregnancy gingivitis) – swollen papilla, may progress to a pregnancy epulis (see Chapter 20).Puberty (puberty gingivitis) – caused by testosterone, for example.Menopause.
Drug‐induced:Anticonvulsants (for epilepsy) – e.g. phenytoin and phenobarbital. Figure 3.4 Drug‐induced gingival growth (immunosuppressants for rheumatoid arthritis).Source: Alison Chapman.Immunosuppressants (anti‐rejection medication for transplant patients) – e.g. cyclosporine ( Figure 3.4).Certain calcium channel blockers (for high blood pressure) – e.g. nifedipine, verapamil, and diltiazem.Deep overbite causing direct gingival trauma.
The OHE needs a basic knowledge of the body’s inflammatory process in order to explain gingivitis to patients who need to deal with the condition. When a word ends in ‘ itis ’, it usually describes an inflammatory condition of a body tissue. For example, tonsill itis is inflammation of the tonsils.
Inflammation is the response of a tissue to injury, and is the first process by which the body defends itself against attack from:
Physical sources (e.g. a blow to the mouth or a scratch from a toothbrush bristle).
Chemical sources (e.g. an aspirin burn or a reaction to chemicals used in dentistry).
Microorganisms (e.g. invasion by bacteria, viruses, or fungi).
Stages of inflammation (also signs of gingivitis)
The four stages of inflammation are also signs of gingivitis that the dental professional may notice:
1 Redness (rubor) – due to increased blood flow.
2 Swelling (tumor) – tissue fluid accumulates.
3 Heat (calor) – tissue temperature increases.
4 Pain (dolor) – rare in gingivitis, but some patients may complain of sore gums.
The words in brackets are Latin and they may help in remembering these stages by association (ruby from rubor ; tumour from tumor ; calories from calor, and doleful from dolor ).
Other signs and symptoms of gingivitis
Signs are what the dental professional notices on examination, symptoms are what the patient may complain of. Both signs and symptoms of gingivitis are reversible and will disappear if inflammation is resolved by improved oral hygiene.
The dental professional may notice:
Loss of stippling – the orange peel appearance seen in healthy attached gingivae, caused by bundles of collagen fibres beneath the epithelium. The inflammatory process damages these bundles and stippling disappears.
Rounding of the gingival margin.
False pocketing – caused by swelling of the marginal gingivae. There is no breach of the junctional epithelium, so the periodontal ligament remains intact.
Loss of contour – gingivae lose their pointed shape due to swelling.
Loss of consistency – gingivae lose their firmness and become soft and spongy.
The patient may complain of:
Red, swollen gums.
Bleeding on brushing – this is often the first thing that patients notice. They may also mention that their gums bleed when eating crisp foods, such as apples, or they may find blood on their pillow in the morning.
Halitosis (fetor oris) – ‘My breath smells’. May be caused by bleeding, but more likely to be noticed in periodontitis when debris becomes trapped in pockets (see Chapter 4).
Itching or pain (rarely) – usually from trauma of vigorous brushing with a stiff brush, or when another factor is present, such as hormonal changes during pregnancy.
Remember! Signs are what the professional notices, symptoms are what the patient complains of.
Treatment should include:
Oral hygiene instruction, encouragement, and motivation.
Removal/good care of potential plaque‐retentive sites.
Fluoride – antibacterial effect, and can be applied via toothpaste or mouthwash.
Chemical (chlorhexidine mouthwash).
Regular monitoring, including scaling, polishing, and reinforcement of oral health instruction.
1 1. The Health and Social Care Information Centre (2011) Disease and Related Disorders – A Report from the Adult Dental Health Survey 2009. The Health and Social Care Information Centre, Leeds.
Chapter 4 Periodontal disease
Learning outcomes
By the end of this chapter you should be able to:
1 Define periodontitis and list the primary and secondary factors in its development.
2 List the signs, symptoms, and features of the condition, and explain its management.
3 Define necrotising ulcerative gingivitis (NUG), its causes and treatment.
4 Define peri‐implant mucositis and peri‐implantitis, and their causes and treatment.
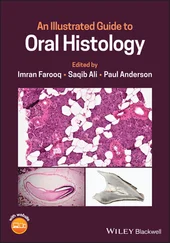
Periodontitis ( Figure 4.1) describes the inflammation and gradual destruction of the periodontium (the supporting structure of the tooth).
Slowly progressing periodontitis was previously called chronic periodontitis , and rapidly progressing disease was called aggressive periodontitis . However, it is now thought that they are variations of the same disease process.
Periodontitis may look like gingivitis, but can be distinguished by:
Periodontal probing (depth of pocket is greater than 3 mm).
X‐rays, which show loss of bone support.
Loose teeth (potentially).
Damage is not reversible.
Remember!It is important that the oral health educator (OHE) can distinguish between gingivitis (the continual but superficial inflammation of the gingivae), and periodontitis (the destruction of the periodontium).

Figure 4.1 Adult periodontal disease.
Source: Alison Chapman.
In the UK Adult Dental Health Survey (2009), only 17% of dentate adults showed no evidence of periodontal disease at the most stringent threshold [1].
Good periodontal health was more common among adults under 45 years old than in older age groups. For example, 20% of dentate adults aged between 25–34 years had very healthy periodontal tissues compared with 14% between 45– 54 years, and 10% above 55 years [1]. Twenty‐one percent of dentate adults from managerial and professional occupation households had very healthy periodontal tissues compared with 16% of adults of intermediate occupations, and 12% of manual occupation households [1].
Читать дальше