In the case of myofascial pain, there is no readily demonstrable histopathology.
There is a multitude of classifications based upon the aetiology, clinical signs and symptoms, or anatomy; all have their weaknesses. Those classification systems that define the different kinds of TMD and utilize the history and examination provide the most help to the general dental practitioner as well as to the researcher.
The gold standard classification system for research is currently the TMD research diagnostic criteria (RDC/TMD).
This is a dual axis classification of TMD pain in a research tool which aims to provide a more rational, scientific basis for TMD diagnosis.
Axis 1: a set of opertionalised RDC for use in evaluating and investigating masticatory muscle pain, DD and degenerative diseases of the TMJ.
Axis 2: a set of operational RDC to assess chronic pain, dysfunction, depression, non‐specific physical symptoms, and orofacial disability.
The RDC categorise TMD criteria into three groups according to the common factors among conditions.
GROUP I: Muscle disorders
1 I.a Myofascial painCriteria: Reported pain in masticatory musclesPain on palpation in at least three sites, one of them at least in the same side of the reported pain.
2 I.b Myofascial pain with limited openingCriteria: Myofascial painPain‐free unassisted opening <40 mm and passive stretch ≥5 mm.
1 II.a DD with reductionCriteria: No pain in the jointReproducible click on excursion with either opening or closing clickWith click on opening and closing (unless excursive click confirmed):Click on opening occurs at ≥5 mm interincisal distance than on closingClicks eliminated by protrusive opening
2 II.b DD without reduction with limited openingCriteria: History of locking or catching that interfered with eatingAbsence of TMJ clickingUnassisted opening (even painful) ≤35 mm and passive stretch ≤4 mmContralateral excursion <7 mm or uncorrected ipsilateral deviation on opening
3 II.c DD without reduction without limited openingCriteria: History of locking or catching that interfered with eatingThe presence of TMJ sounds excluding DDR clickingUnassisted opening (even painful) >35 mm and passive stretch >4 mmContralateral excursion ≥7 mm 5. Optional imaging (Arthrography or MRI) to confirm DD
GROUP III: Other common joint disorders
1 III.a ArthralgiaPain and tenderness/no crepitationCriteria: Pain on TMJ palpation either laterally or intra auricularSelf‐reported joint pain with or without jaw movementAbsence of crepitus, and possibility of clicking
2 III.b OsteoarthritisInflammatory conditionPainCrepitation and/or changes on radiographCriteria: Pain as for arthralgiaCrepitus on any movement or radiographic evidence of joint changes
3 III.c OsteoarthrosisDegenerative disorderNo painCrepitation and/or changes on radiographCriteria: Crepitus on any movement or radiographic evidence of joint changesNo reported joint pain nor pain on any movement
1 Avery, J. (2006). Essential of Oral Histology and Embryology: A Clinical Approach, 3nde. St Louis, MO: Mosby.
2 Gage, J.P. (1989). Mechanisms of disc displacement in the temporomandibular joint. Aust Dent J 34: 427–436.
3 Gray, R.J., Davies, S.J., and Quayle, A.A. (1994). A clinical approach to temporomandibular disorders. 1. Classification and functional anatomy. Br Dent J 176: 429–435.
4 Rees, L.A. (1954). The structure and function of the mandibular joint. J Br Dent AssocXCVI: 126–133.
5 Schiffman, E., Ohrbach, R., Truelove, E. et al. (2014). Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache 28: 6–27.
3 Articulatory System Examination
 Examination of the articulatory system should be a routine that you perform for all new patients and at regular intervals for existing patients, even those whom you know well. Symptoms of a temporomandibular disorder can come and go, and the patient may present complaining of the recent onset of a symptom such as a click which, by chance, was not present at the time of your previous examination. The three components to examine are the temporomandibular joints (TMJs), the mandibular muscles, and the occlusion.
Examination of the articulatory system should be a routine that you perform for all new patients and at regular intervals for existing patients, even those whom you know well. Symptoms of a temporomandibular disorder can come and go, and the patient may present complaining of the recent onset of a symptom such as a click which, by chance, was not present at the time of your previous examination. The three components to examine are the temporomandibular joints (TMJs), the mandibular muscles, and the occlusion.
 1 Examination of the temporomandibular joints
1 Examination of the temporomandibular joints
Range of movement 
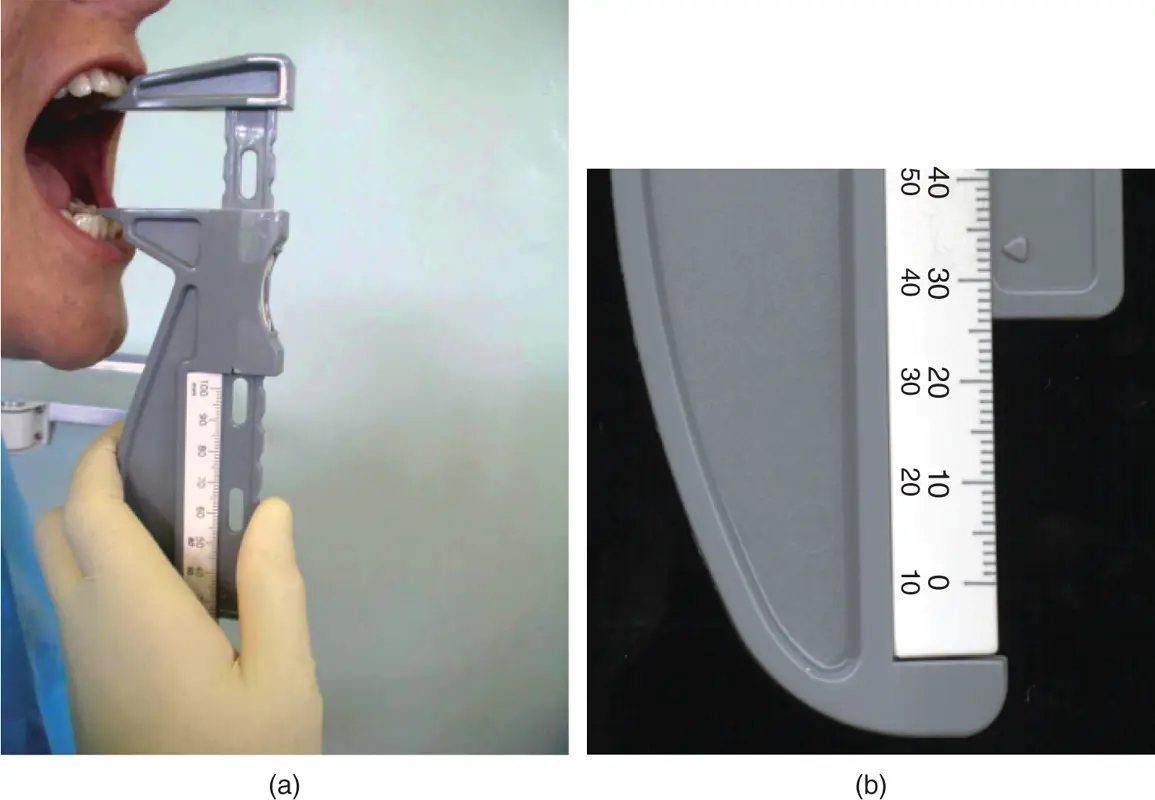
Examination of the range of movement involves examining the interincisal opening, both pain‐free and maximum ( Figure 3.1) and lateral excursions of the mandible.
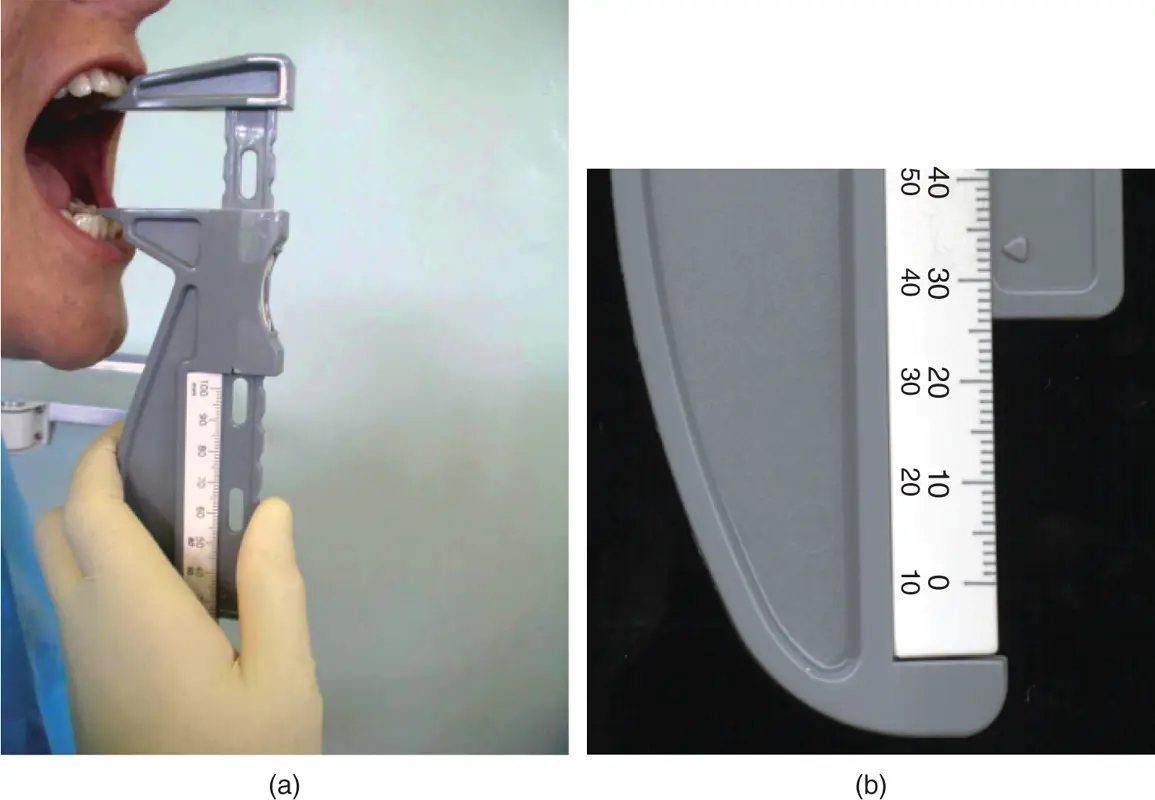
Figure 3.1Measurement of incisal opening.
(M. Ziad Al‐Ani, Robin J.M. Gray.)
The lower limit of normal range of incisal opening is regarded as being approximately 35 mm for female patients and 42 mm for male patients. The opening is usually measured from incisal tip to incisal tip. It does not matter whether or not the overbite is included in your measurement regimen as long as you are always consistent in either including the overbite or excluding it so that your measurements are comparable and reproducible.
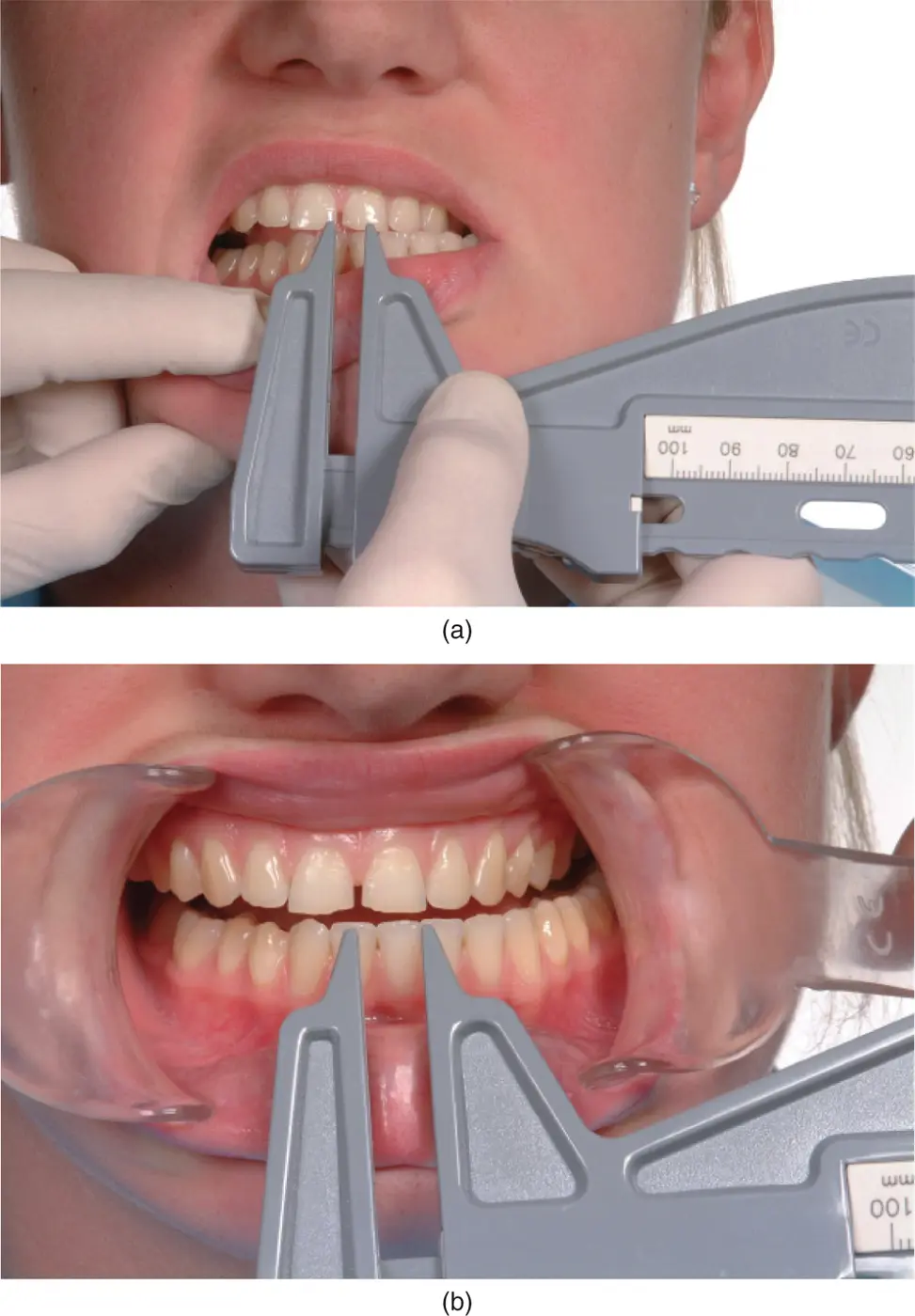
The range of lateral mandibular excursions (lower limit 8 mm on either side) should be measured from upper incisal midline to lower midline, with the patient moving the mandible first to one side then to the other ( Figure 3.2).
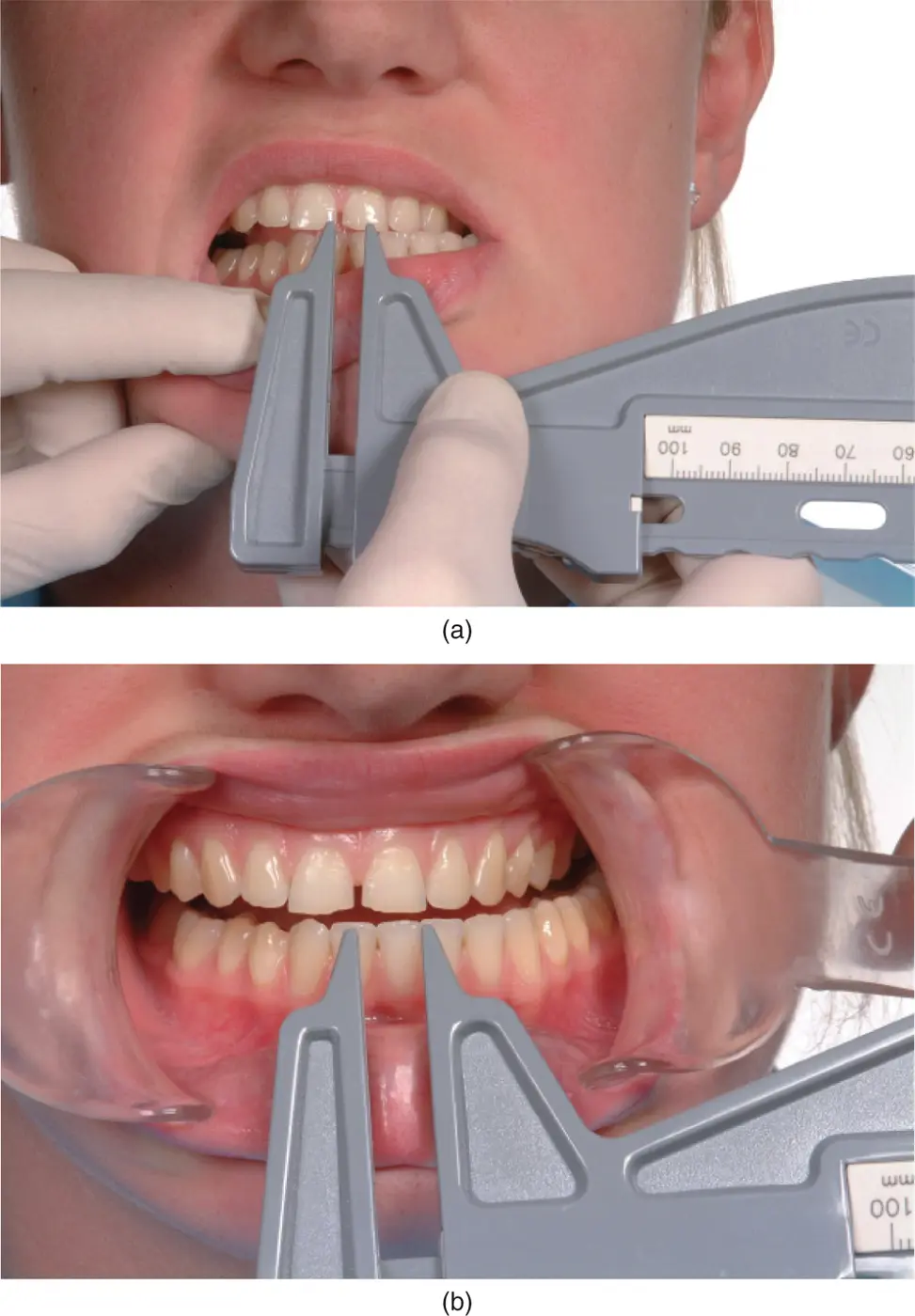
Figure 3.2Measurement of lateral jaw movement.
(M. Ziad Al‐Ani, Robin J.M. Gray.)
Any starting discrepancy in the incisal midlines when the patient is in centric occlusion should be taken into account.
Stand in front of your patient and ask him or her to repeatedly open and close the mouth as far as comfortably possible. Carefully watch the pathway and range of jaw movement. You can learn a lot from looking!
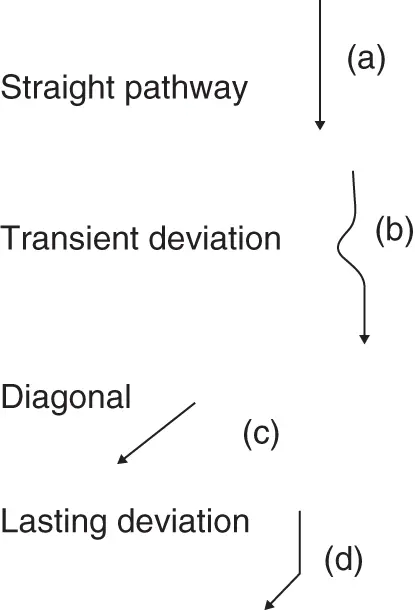
The mandible can open in a straight pathway or with a transient or lasting deviation. The mandibular pathway can be observed by standing in front of the patient and asking the patient to repeatedly open and close the mouth. Limitation or deviation of mandibular movement can be caused by two principal factors: either pain in the mandibular muscles or TMJ, or a physical obstruction to movement. Much can be gained from examining the patient slowly opening and closing the mouth ( Figure 3.3).
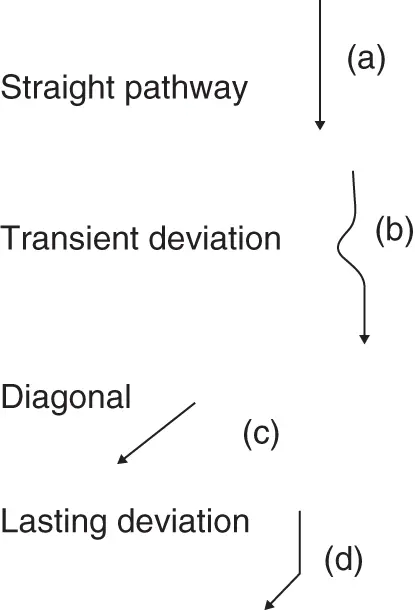
Figure 3.3Diagrammatic representation of mandibular movements.
If the pathway is straight throughout the whole range of mandibular movement, this indicates that both joints are acting synchronously ( Figure 3.3a).
Читать дальше
 Examination of the articulatory system should be a routine that you perform for all new patients and at regular intervals for existing patients, even those whom you know well. Symptoms of a temporomandibular disorder can come and go, and the patient may present complaining of the recent onset of a symptom such as a click which, by chance, was not present at the time of your previous examination. The three components to examine are the temporomandibular joints (TMJs), the mandibular muscles, and the occlusion.
Examination of the articulatory system should be a routine that you perform for all new patients and at regular intervals for existing patients, even those whom you know well. Symptoms of a temporomandibular disorder can come and go, and the patient may present complaining of the recent onset of a symptom such as a click which, by chance, was not present at the time of your previous examination. The three components to examine are the temporomandibular joints (TMJs), the mandibular muscles, and the occlusion. 1 Examination of the temporomandibular joints
1 Examination of the temporomandibular joints





![John Bruce - The Lettsomian Lectures on Diseases and Disorders of the Heart and Arteries in Middle and Advanced Life [1900-1901]](/books/749387/john-bruce-the-lettsomian-lectures-on-diseases-and-disorders-of-the-heart-and-arteries-in-middle-and-advanced-life-1900-1901-thumb.webp)