1 ...8 9 10 12 13 14 ...24 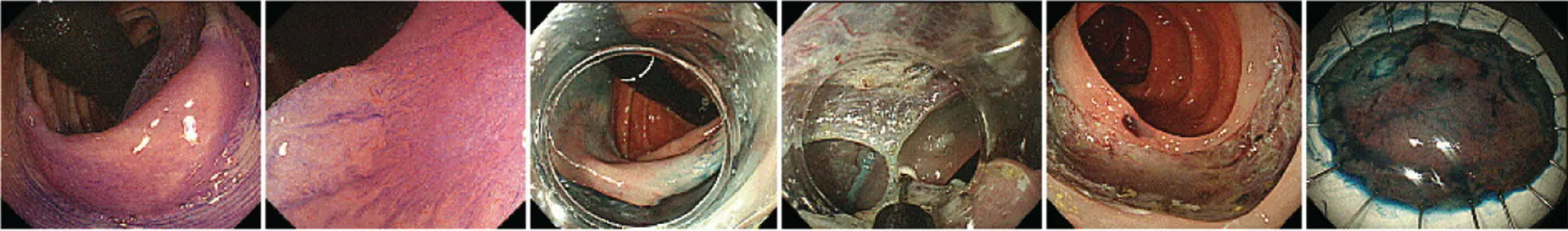
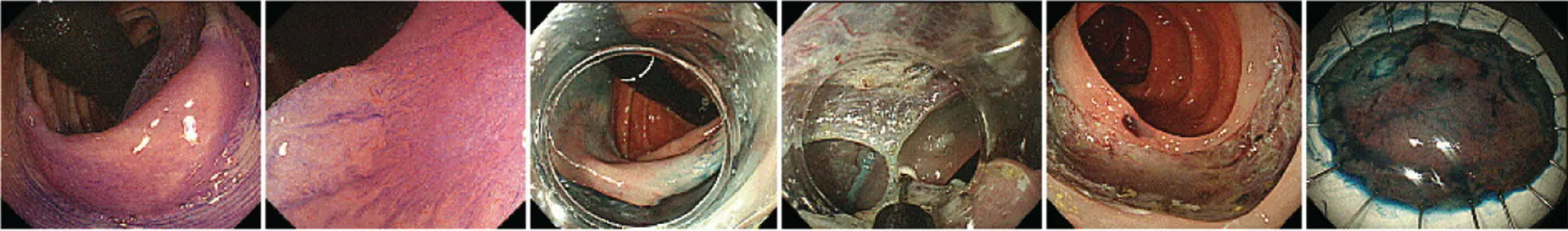
Figure 1.14 Endoscopic submucosal dissection (ESD) procedure. A flat neoplastic lesion is seen in panel 1–2 after staining with cresyl violet. The margins are incised (panel 3) with the endoscope retroflexed (black tube). The submucosal plane is dissected with a needle knife (panel 4). The final resection site (panel 5) and corresponding resection specimen prepared for pathology processing (panel 6).
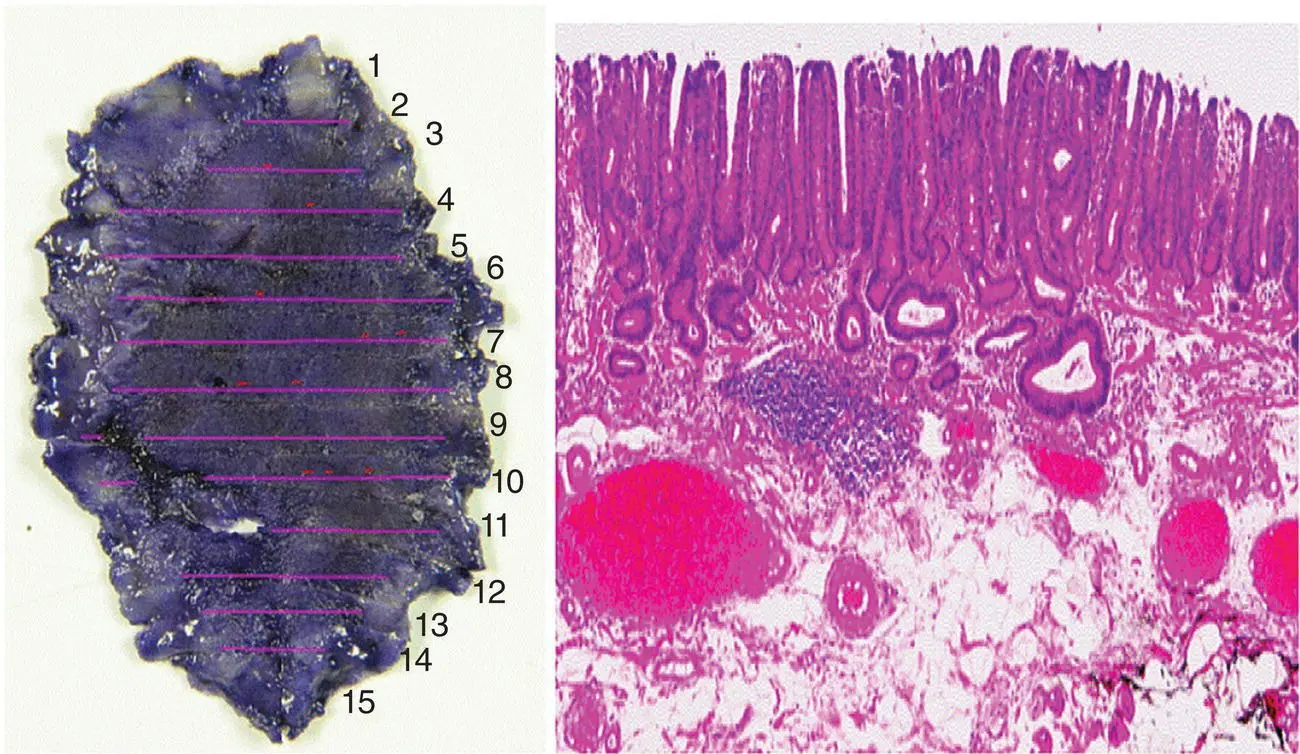
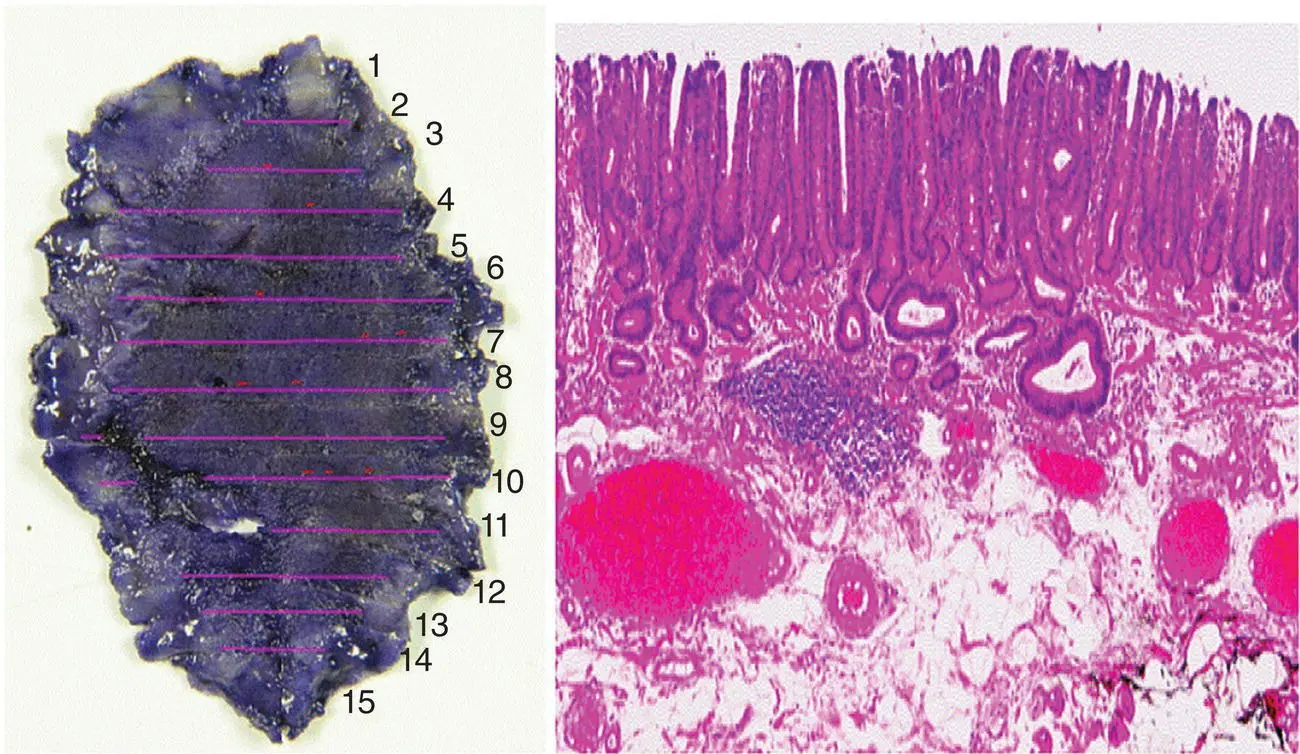
Figure 1.15 Endoscopically resected en bloc well‐differentiated adenocarcinoma 28 × 17 mm with superficial submucosal invasion and no lymphovascular invasion and negative horizontal and vertical margins. This sample meets criteria for endoscopic curative resection.
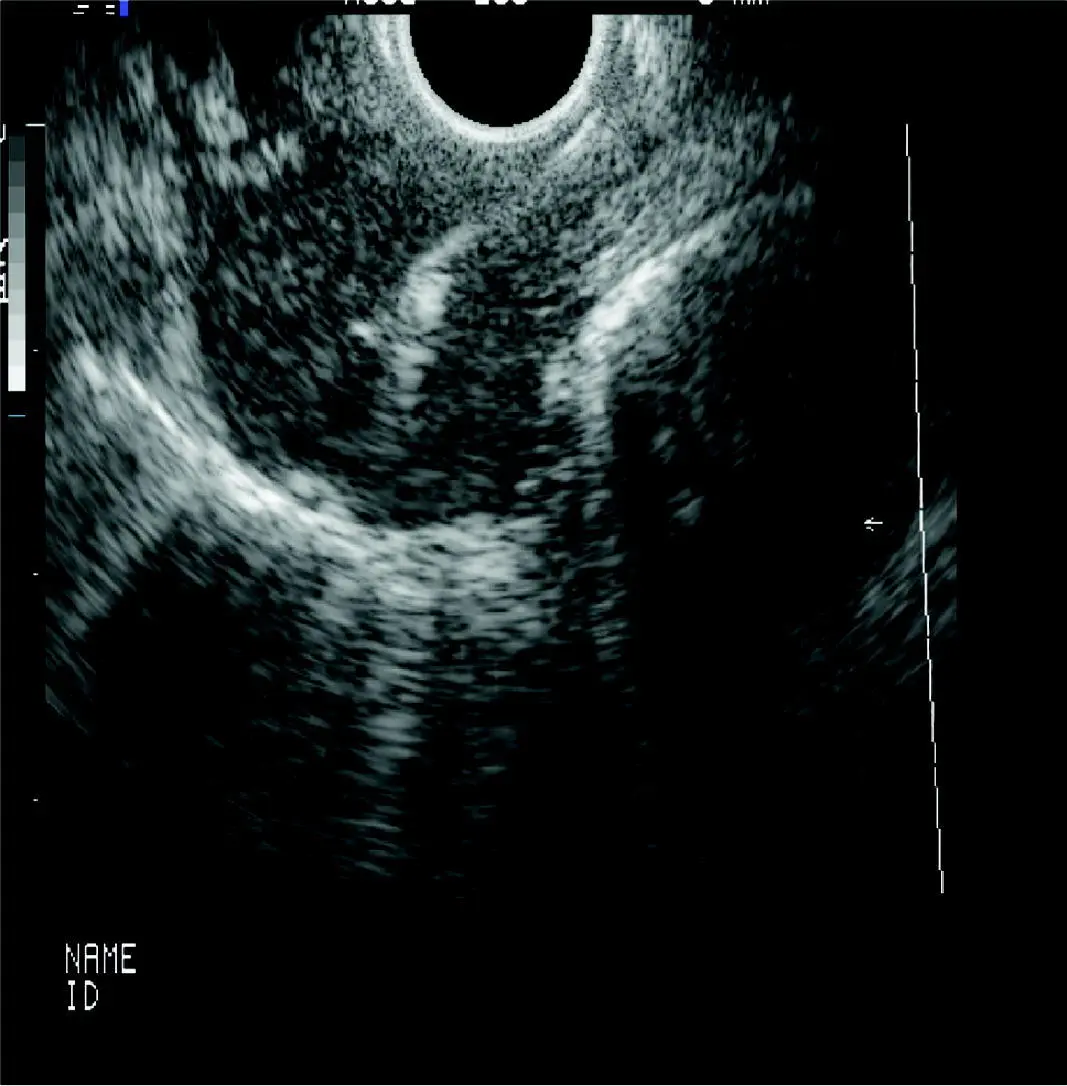
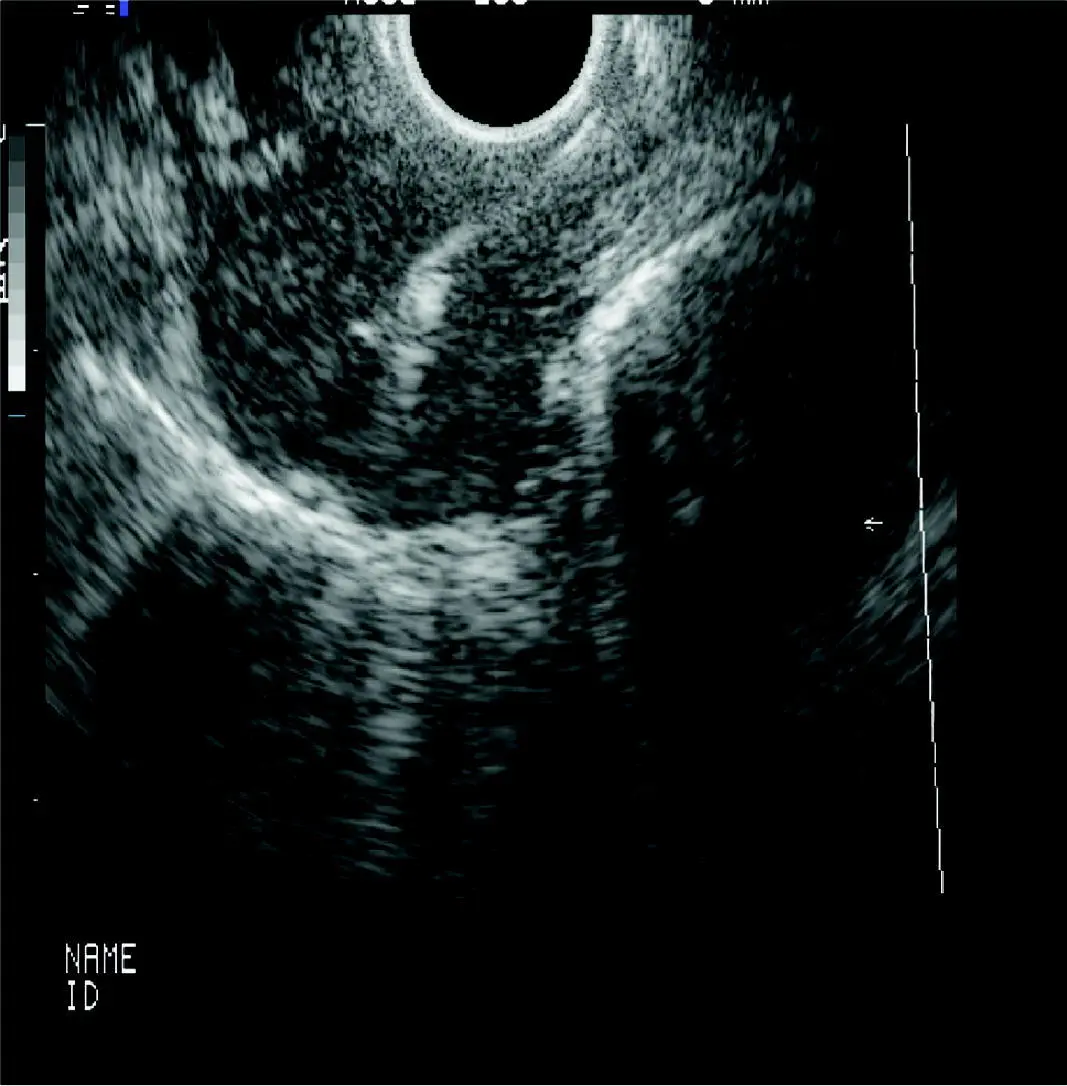
Figure 1.16Large mediastinal lymph node sampled with EUS‐FNA. The needle is seen entering from the upper right of the screen into the tumor in the center of the image.
1 Al‐Haddad, M. and Eloubeidi, M.A. (2008). Diagnostic and therapeutic applications of endoscopic ultrasound‐guided punctures. Dig. Dis. 26 (4): 390–397.
2 Basford, P., George, R., Nixon, E. et al. (2014). Endoscopic resection of sporadic duodenal adenomas: comparison of endoscopic mucosal resection (EMR) with hybrid endoscopic submucosal dissection (ESD) techniques and the risks of late delayed bleeding. Surg. Endosc. 28 (5): 1594–1600.
3 da Cunha Santos, G., Boerner, S.L., and Geddie, W.R. (2011). Maximizing the yield of lymph node cytology: lessons learned from rapid onsite evaluation of image‐ and endoscopic‐guided biopsies of hilar and mediastinal lymph nodes. Cancer Cytopathol. 119 (6): 361–366.
4 Eloubeidi, M.A., Tamhane, A., Jhala, N. et al. (2006). Agreement between rapid onsite and final cytologic interpretations of EUS‐guided FNA specimens: implications for the endosonographer and patient management. Am. J. Gastroenterol. 101 (12): 2841–2847.
5 Falk, G.W., Rice, T.W., Goldblum, J.R., and Richter, J.E. (1999). Jumbo biopsy forceps protocol still misses unsuspected cancer in Barrett's esophagus with high‐grade dysplasia. Gastrointest. Endosc. 49 (2): 170–176.
6 Gupta, N., Mathur, S.C., Dumot, J.A. et al. (2012). Adequacy of esophageal squamous mucosa specimens obtained during endoscopy: are standard biopsies sufficient for postablation surveillance in Barrett's esophagus? Gastrointest. Endosc. 75 (1): 11–18.
7 Hikichi, T., Irisawa, A., Bhutani, M.S. et al. (2009). Endoscopic ultrasound‐guided fine‐needle aspiration of solid pancreatic masses with rapid on‐site cytological evaluation by endosonographers without attendance of cytopathologists. J. Gastroenterol. 44 (4): 322–328.
8 Humphris, J.T.J., Kwok, A., and Katelaris, P.H. (2007). Cold snare polypectomy for diminutive polyps: an assessment of the risk of incomplete removal of small adenomas. Gastrointest. Endosc. 69: AB207.
9 Ichise, Y., Horiuchi, A., Nakayama, Y., and Tanaka, N. (2011). Prospective randomized comparison of cold snare polypectomy and conventional polypectomy for small colorectal polyps. Digestion 84 (1): 78–81.
10 Ikematsu, H., Yoda, Y., Matsuda, T. et al. (2013). Long‐term outcomes after resection for submucosal invasive colorectal cancers. Gastroenterology 144 (3): 551–559. quiz e514.
11 Johanson, J.F., Frakes, J., and Eisen, D. (2011). Computer‐assisted analysis of abrasive transepithelial brush biopsies increases the effectiveness of esophageal screening: a multicenter prospective clinical trial by the EndoCDx Collaborative Group. Dig. Dis. Sci. 56 (3): 767–772.
12 Kadri, S.R., Lao‐Sirieix, P., O'Donovan, M. et al. (2010). Acceptability and accuracy of a non‐endoscopic screening test for Barrett's oesophagus in primary care: cohort study. BMJ 341: c4372. https://doi.org/10.1136/bmj.c4372.
13 LeBlanc, J.K., Emerson, R.E., Dewitt, J. et al. (2010). A prospective study comparing rapid assessment of smears and ThinPrep for endoscopic ultrasound‐guided fine‐needle aspirates. Endoscopy 42 (5): 389–394.
14 Levy, M.J., Reddy, R.P., Wiersema, M.J. et al. (2005). EUS‐guided trucut biopsy in establishing autoimmune pancreatitis as the cause of obstructive jaundice. Gastrointest. Endosc. 61 (3): 467–472.
15 Mann, N.S., Mann, S.K., and Alam, I. (1999). The safety of hot biopsy forceps in the removal of small colonic polyps. Digestion 60 (1): 74–76.
16 Monkemuller, K.E., Fry, L.C., Jones, B.H. et al. (2004). Histological quality of polyps resected using the cold versus hot biopsy technique. Endoscopy 36 (5): 432–436.
17 Phoa, K.N., van Vilsteren, F.G., Weusten, B.L. et al. (2014). Radiofrequency ablation vs endoscopic surveillance for patients with Barrett esophagus and low‐grade dysplasia: a randomized clinical trial. JAMA 311 (12): 1209–1217.
18 Qumseya, B.J., Wang, H., Badie, N. et al. (2013). Advanced imaging technologies increase detection of dysplasia and neoplasia in patients with Barrett's esophagus: a meta‐analysis and systematic review. Clin. Gastroenterol. Hepatol. 11 (12): 1562–1570. e1561–e1562.
19 Sakamoto, T., Matsuda, T., Nakajima, T., and Saito, Y. (2012). Efficacy of endoscopic mucosal resection with circumferential incision for patients with large colorectal tumors. Clin. Gastroenterol. Hepatol. 10 (1): 22–26.
20 Sharaf, R.N., Shergill, A.K., Odze, R.D. et al. (2013). Endoscopic mucosal tissue sampling. Gastrointest. Endosc. 78 (2): 216–224.
21 Trier, J.S. (1971). Diagnostic value of peroral biopsy of the proximal small intestine. N. Engl. J. Med. 285 (26): 1470–1473.
22 Vogelstein, B., Fearon, E.R., Hamilton, S.R. et al. (1988). Genetic alterations during colorectal‐tumor development. N. Engl. J. Med. 319 (9): 525–532.
23 Wang, K.K. and Sampliner, R.E. (2008). Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus. Am. J. Gastroenterol. 103 (3): 788–797.
24 Watanabe, T., Itabashi, M., Shimada, Y. et al. (2012). Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int. J. Clin. Oncol. 17 (1): 1–29.
25 Wu, L., Li, P., Wu, J. et al. (2012). The diagnostic accuracy of chromoendoscopy for dysplasia in ulcerative colitis: meta‐analysis of six randomized controlled trials. Color. Dis. 14 (4): 416–420.
2 Esophagus Inflammatory Conditions
Anthony R. Mattia1, Gregory Y. Lauwers2, Michael B. Wallace3 and Till S. Clauditz4
1 Newton‐Wellesley Hospital, Newton, MA, USA
2 Moffitt Cancer Center, Tampa, Florida, USA
3 Mayo Clinic, Jacksonville, Florida, USA
4 Department of Pathology, University‐Medical Center, Hamburg, Germany
Normal Histology, Variations
The esophagus has a pearly white and smooth surface under which a network of small vessels is seen ( Figure 2.1) except for the distal esophageal sphincter where prominent longitudinal and palisading vessels (exceeding 100 mm in diameter) are observed and used to define the esophagogastric junction.
The esophageal mucosa is composed of a non‐keratinizing flat stratified squamous epithelium, lamina propria, and muscularis mucosae ( Figure 2.2; Table 2.1). The squamous epithelium is 10–20 cell layers thick measuring 300–500 μm in thickness. The prickle cells contain a large quantity of cytoplasmic glycogen, which stains positively with periodic acid–Schiff (PAS). The basal proliferative zone, the cuboidal or polyhedral basal and parabasal cells account for 15% or less of the epithelial thickness. A small number of specialized cell types, including T lymphocytes, Langerhans cells, endocrine cells, and melanocytes are also present in the deep/parabasal epithelium. The lamina propria consists of loose connective tissue with scattered inflammatory cells, vessels, nerves, and small mucous glands. The lamina propria papillae normally extend into the epithelium for 1/3–1/2 of its thickness. The muscularis mucosae is a thick layer of smooth muscle bundles oriented longitudinally. In the distal 1–2 cm of the esophagus, the basal zone, papillae, and intraepithelial cells may be more prominent, and include rare eosinophils. Esophageal mucosal biopsies typically include the squamous epithelium and scant lamina propria. The muscularis mucosae is seldom present, and better identified in esophageal mucosal resection specimens.
Читать дальше