Today, the management of SDB represents an enormous worldwide medical economy. We know that snoring, upper airway resistance syndrome (UARS), and its end-expression of OSA is a major contributor to the development of obesity, diabetes, and cardiovascular disease in the forms of hypertension, stroke, and heart attack risk. We also know that OSA, UARS, and SDB have primary effects related to childhood cognitive performance and physical growth (see Fig 2-1) and adult-related risk of traffic accidents or workplace injury.
The Australian government, along with the Royal Australasian College of General Practitioners, has dedicated enormous economic and medical resources to the endeavor of surveillance, diagnosis, and management of SDB. Australia has led the way with developing treatments for snoring. Both the CPAP machine and at least one major dental (MAD) device company, SomnoMed, began their lives in backyard Australian garages. For almost 100 years, the dentist has been front and center of the war against snoring, and Australian dentists have helped lead the way for the past 20 years.
Most of us really don’t know what causes UARS. And people may not know the small mandible is a major primary cause of snoring. Physicians find this difficult to see, because a fat neck and obesity and aging often mask the small chin. In older kids, dentists recognize the Class II malocclusion associated with the small mandible relatively easily. But in adults, this dental sign of the small mandible can be obscured by the camouflage orthodontics the patient had during adolescence.
By identifying the small mandible and recognizing glossoptosis, the dental practitioner is the primary means of identifying the risk of snoring. Whether it is in the child presenting with a big dental overbite or in the adult presenting in the late stages of full-blown OSA, the dentist is front and center in the ability to offer definitive help.
By working with the orthodontic practitioner, sleep physician, or maxillofacial surgeon, the dentist becomes much more than someone giving fillings, extracting teeth, or applying splints. They become a frontline oral physician, applying their expertise of head and neck anatomy and clinical diagnosis for the cure of a first-world medical disease.
OBSTRUCTIVE SLEEP APNEA
The stories that many older people offer when discussing why they are on a CPAP machine often start with the terrifying discovery of their unconscious apneic states ( Fig 2-3). What started as innocent weight gain, or complaints of daytime tiredness or general mental fogginess, or a sleeping partner’s complaint of relentless snoring, eventually becomes a cry of an unbearable, life-dependent, and desperate need for medical help.
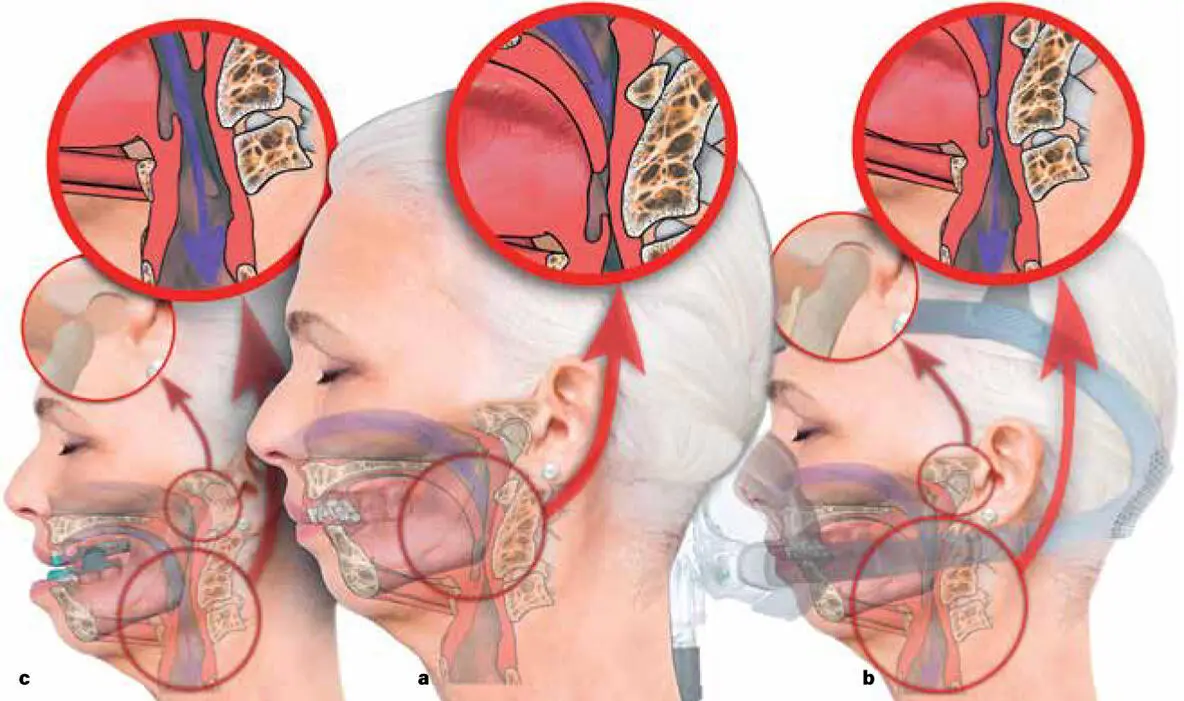
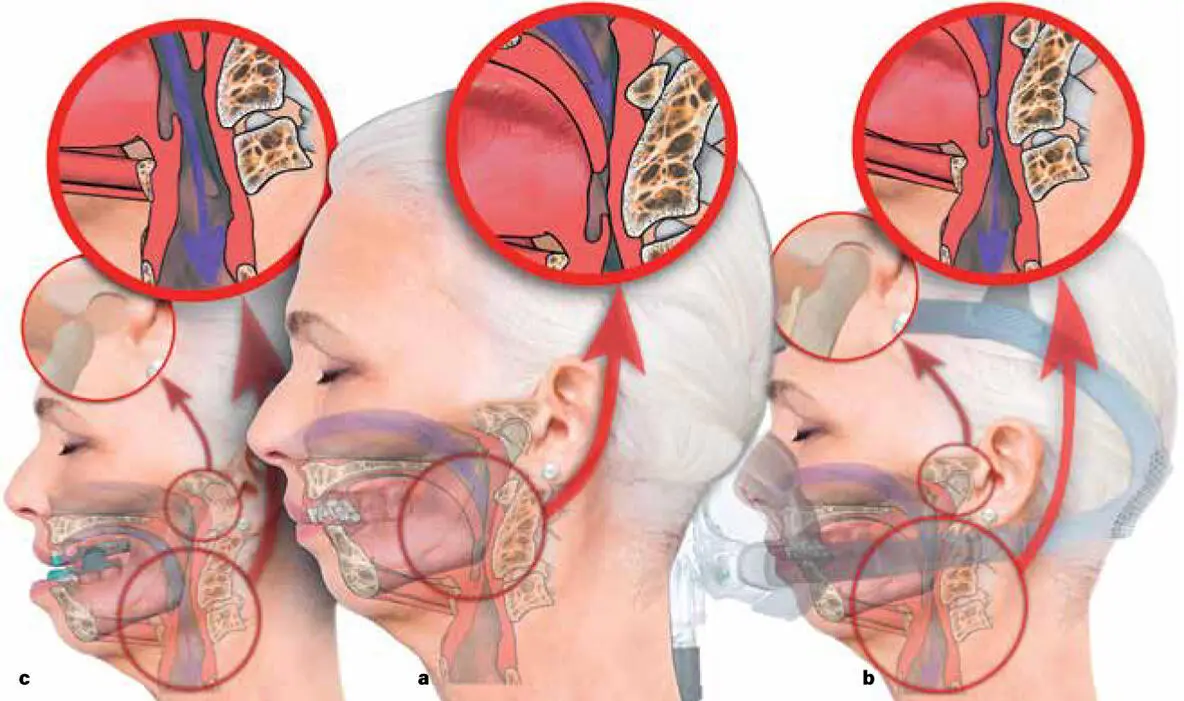
FIG 2-3 (a) The person with increased UARS will obstruct their upper airway between their soft palate and upper epiglottis at approximately the level of the 2nd and 3rd cervical vertebrae (inset). This is called a closed torus or horn torus . The author anatomically calls this C3ERPO, or 3rd cervical, upper epiglottic, retropharyngeal obstruction. (b) Using increased air pressure will drive air via the nose and push open the collapsed airway (torus) through the collapsed C3ERPO column (large inset). Increasing nasal air pressure through the CPAP can be titrated against the upper airway resistance, pneumatically opening the collapsed torus, until airway passage occurs through the C3ERPO region. The temporomandibular joint (TMJ) remains in its normal position (small inset). (c) Pulling the mandible forward through use of a MAD will directly pull the lower part of the C3ERPO column forward and hold the mouth partially open, allowing mouth breathing to occur (large inset). The forward position of the mandible moves the TMJ out of its fossa (small inset), which can lead to the development of TMJ pathology. The splint itself can orthodontically retrude the maxillary teeth and procline the mandibular teeth, eventually leading to development of a chronic malocclusion.
Diagnosing OSA
The general medical practitioner’s referral to a sleep specialist can be a frustrating one for their patient. Linked up to machines and monitors through wires and stickers—and in a hospital bed with technicians and soft lights, strange sheets, and different pillows—is not a true replication of your own bedroom and your own natural state. In this anxious environment, many people find it hard to fall asleep. Or they wake up early and often.
And the test, unless it is repeated regularly and averaged, is not truly a reflection of how well or poorly a patient naturally sleeps at home and over many months. For many people who snore and who take part in a sleep study, they may still come away without a positive test outcome to confirm that they have OSA. Without a critical AHI score barrier (> 5 apnea or hypopnea episodes an hour), the offer of relief through CPAP may be frustratingly denied; or, at best, a repeat sleep study, with all the attendant inconveniences of that, is all that may be offered.
AHI SCORE
Usually, an admission to the hospital provides a sleep technician who will monitor a range of physiologic activities during sleep. Restlessness, blood-oxygen saturation, brain wave activity, nasal air movement, blood pressure, heart rate, and breathing effort are all measured. In the morning, the sleep physician will then analyze the data in a way that will give a number. This number is called the apnea-hypopnea index or AHI. It is a reflection of the number of sleep-wake cycles and low oxygen periods—or choking attacks—a person may or may not have per hour and averaged over the sleeping period. It is scored as mild (5–14), moderate (15–29), or severe OSA (30+).
While snoring, poor sleep, or daytime tiredness is often part and parcel of why people attend a sleep study, for the sleep physician the important medical question is to confirm whether a person is suffocating in their sleep or not. Having apnea literally means you are not breathing. And without breathing your blood-oxygen levels can fall low enough that you may simply not wake up. Ever.
Having a high AHI number (> 5 in adults), along with other measurement parameters, will help confirm a diagnosis of OSA. Being diagnosed with OSA is important to know, because the condition is linked to developing high blood pressure as well as myriad irreversible problems such as arterial wall thickening, stroke risk, heart disease, kidney disease, and diabetes. Most importantly, OSA is associated with a real association of reduced life span, which is a product of developing diseases that directly arise from having chronically low blood-oxygen levels.
Even though it may be the reason why a person first went for a sleep study, a complaint of snoring fundamentally does not primarily support a diagnosis for OSA, and there are no physical signs, other than the AHI score, that a doctor can search for that will positively support a diagnosis of OSA. Some patients who snore are not actually measurably choking in the night. Hospital-based studies exist to assess whether the patient has a critical number of apnea or hypopnea episodes; they are not designed to determine whether that patient has the risk factors that may or may not meet the criteria for OSA in the future. Nevertheless, the diagnosis of OSA is one that belongs to the sleep physician. For an AHI score above 5, CPAP is the remedial treatment of choice by the sleep physician to reduce the AHI score.
Treating OSA
Unfortunately, the medical profession is less interested in “why” or “how” a patient is obstructing their airway than whether or not they are actually suffocating in their sleep. We know that medically treating airway collapse during sleep, regardless of the reason, is relatively accessible. And as long as you haven’t reached a physical end-point, for most people there is at least a limited promise of potential relief.
Читать дальше