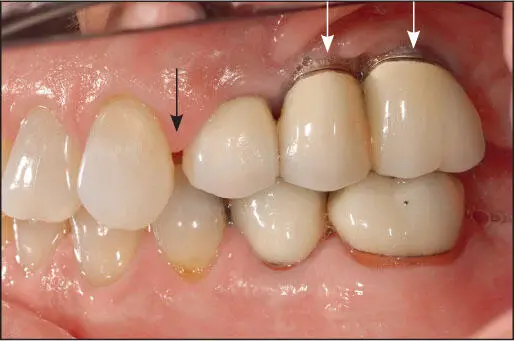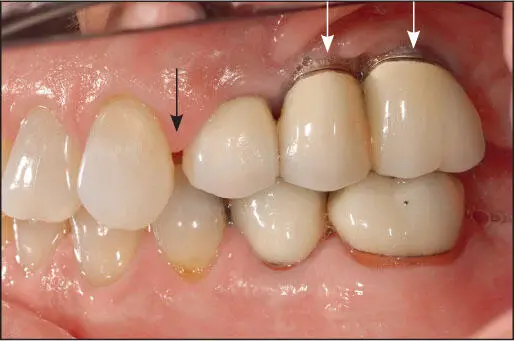
Fig 1-20 Three implants were used to restore the posterior teeth. A 20-year follow-up photograph. Note the significant mesial migration of the anterior teeth, resulting in a large space between the canine and the implant-supported fixed dental prosthesis (black arrow) . Note also the apical migration of bone and soft tissue around the two posterior implants (white arrows) .

Fig 1-21 (a) Delivery; (b) 6-year follow-up; (c) 20-year follow-up. Note the continuous apical migration of bone and soft tissues around these implant-retained fixed dental prostheses. Also, note the progressive eruption and mesial migration of the adjacent natural dentition, and the numerous instances of chipping and fracture of the laminated porcelain. (Courtesy of Dr A. Davodi.)
Summary
Osseointegrated implants are highly predictable when used appropriately, and in many situations, implant treatment is as predictable or even more predictable than any of the conventional restorative procedures used to restore missing dentition. The key to predictable outcomes when implants are employed is accurate diagnosis and appropriate treatment planning, taking into account significant patient history findings such as parafunctional activities as well as implant biomechanics and the occlusal schemes to minimize undesirable occlusal forces. Successful outcomes are best accomplished in a multidisciplinary setting. The purpose of these volumes is to share with clinicians the approach to patient evaluation and treatment that has enabled the authors to provide these services with a very high degree of success. Indeed, when implant therapy is planned and executed properly, taking into account the basic principles of prosthodontics, it is the authors’ expectation that once the implants are osseointegrated, while the prostheses that are retained by the implants may need to be replaced due to wear or breakage, the implants should last the lifetime of the patient. Recent innovations, including tilted implants, new and improved CAD/CAM systems, advances in implant body design, surgical enhancement of bone and soft tissues associated with the implant sites, and refinement of loading protocols, have improved implant and prosthesis success.
References
1.Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg 1977;16:1–132.
2.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;10:387–416.
3.Moy P, Pozzi A, Beuemer J 3rd (eds). Fundamentals of Implant Dentistry. Vol 2: Surgical Principles. Chicago: Quintessence, 2016.
4.Steinberg AD, Willey R, Drummond JL. In-vivo comparisons of clot formation on titanium and hydroxyapatite-coated titanium. J Periodontol 1992;63:990–994.
5.Park JY, Gemmell CH, Davies JE. Platelet interactions with titanium: Modulation of platelet activity by surface topography. Biomaterials 2001;22:2671–2682.
6.Thor A, Rasmusson L, Wennerberg A, et al. The role of whole blood in thrombin generation in contact with various titanium surfaces. Biomaterials 2007;28:966–974.
7.Kammerer PW, Gabriel M, Al-Nawas B, Scholz T, Kirchmaier CM, Klein MO. Early implant healing: Promotion of platelet activation and cytokine release by topographical, chemical and biomimetical titanium surface modifications in vitro. Clin Oral Implants Res 2012;23:504–510.
8.Davies JE. Understanding peri-implant endosseous healing. J Dent Educ 2003;67:932–949.
9.Aita H, Hori N, Takeuchi M, et al. The effect of ultraviolet functionalization of titanium on integration with bone. Biomaterials 2009; 30:1015–1025.
10.Att W, Ogawa T. Biological aging of implant surfaces and their restoration with ultraviolet light treatment: A novel understanding of osseointegration. Int J Oral Maxillofac Implants 2012;27:753–761.
11.Cha JY, Pereira MD, Smith AA, et al. Multiscale analysis of the bone-implant interface. J Dent Res 2015;94:482–490.
12.Wang L, Wu Y, Perez KC, et al. Effects of condensation on peri-implant bone density and remodeling. J Dent Res 2017;96:413–420.
13.Khayat PG, Arnal HM, Tourbah BI, et al. Clinical outcome of dental implants placed with high insertion torques (up to 176 Ncm). Clin Implant Dent Relat Res 2013;15:227–233.
14.Grandi T, Guazzi P, Samarani R, et al. Clinical outcome and bone healing of implants placed with high insertion torque: 12-month results from a multicenter controlled cohort study. Int J Oral Maxillofac Surg 2013;42:516–520.
15.Glauser R, Sennerby L, Meredith N, et al. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading. Successful vs failing implants. Clin Oral Implants Res 2004;15:428–434.
16.Norton MR. The influence of low insertion torque on primary implant stability, implant survival and maintenance of marginal bone levels—A cohort prospective study. Int J Oral Maxillofac Implants 2017;32:849–857.
17.Duyck J, Vandamme K, Geris L, et al. The influence of micro-motion on the tissue differentiation around immediately loaded cylindrical turned implants. Arch Oral Biol 2006;51:1–9.
18.Frost HM. Bone “mass” and the “mechanostat”: A proposal. Anat Rec 1987;219:1–9.
19.Frost HM. Wolff’s law and bone structural adaptation to mechanical usage: An overview for clinicians. Angle Orhod 1994;64:175–188.
20.Botticelli D, Berglundh T, Persson LG, Lindhe J. Bone regeneration at implants with turned or rough surfaces in self-contained defects. An experimental study in the dog. J Clin Periodontol 2005;32:448–455.
21.Ogawa T, Nishimura I. Different bone integration profiles of turned and acid-etched implants associated with modulated expression of extracellular matrix genes. Int J Oral Maxillofac Implants 2003;18:200–210.
22.Davies JE. Mechanisms of endosseous integration. Int J Prosthodont 1998;11:391–401.
23.Ogawa T, Nishimura I. Genes differentially expressed in titanium healing. J Dent Res 2006;85:566–570.
24.Butz F, Aita H, Wang CC, Saruwatari L, Ogawa T. Harder and stiffer osseointegrated bone to roughened titanium. J Dent Res 2006;85:560–565.
25.Takeuchi K, Saruwatari L, Nakamura H, Yang JM, Ogawa T. Enhancement of biomechanical properties of mineralized tissue by osteoblasts cultured on titanium with different surface topographies. J Biomed Mater Res 2005;72A:296–305.
26.Garetto LP, Chen J, Parr JA, Roberts WE. Remodeling dynamics of bone supporting rigidly fixed titanium implants: A histomorphologic comparison in four species including humans. Implant Dent 1995;4:235–243.
27.Roberts WE. Orthodontic anchorage with osseointegrated implants: Bone physiology, metabolism, and biomechanics. In: Higuchi KW (ed). Orthodontic Applications of Osseointegrated Implants. Chicago: Quintessence, 2000:161–190.
28.Berglundh T, Lindhe J. Dimension of the peri-implant mucosa. Biological width revisited. J Clin Periodontol 1996;23:971–973.
29.Eggert FM, Levin L. Biology of teeth and implants: The external environment, biology of structures, and clinical aspects. Quintessence Int 2018;49:301–312.
30.Linkevicius T, Vindasiute E, Puisys A, Linkeviciene L, Maslova N, Puriene A. The influence of the cementation margin position on the amount of undetected cement. A prospective clinical study. Clin Oral Implants Res 2013;24:71–76.
Читать дальше