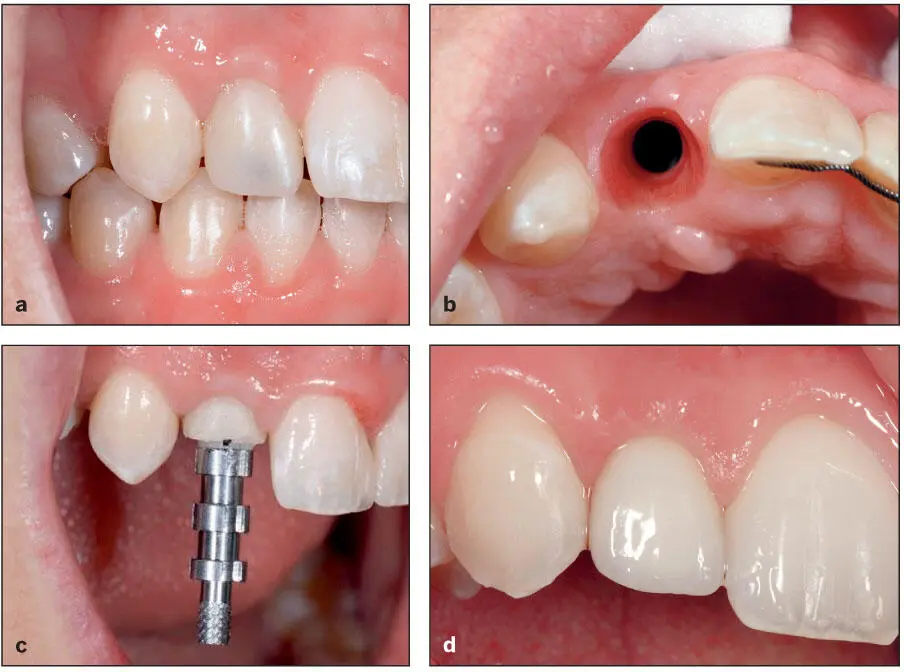
In the esthetic zone, techniques have evolved that idealize the soft tissue contours around the implant prostheses. Provisional restorations are designed to support the soft tissues and develop ideal contours, and these contours can be recorded using customized impression techniques ( Fig 1-10). In addition, surgical procedures have been developed that can be used to enhance bone and soft tissue contours.
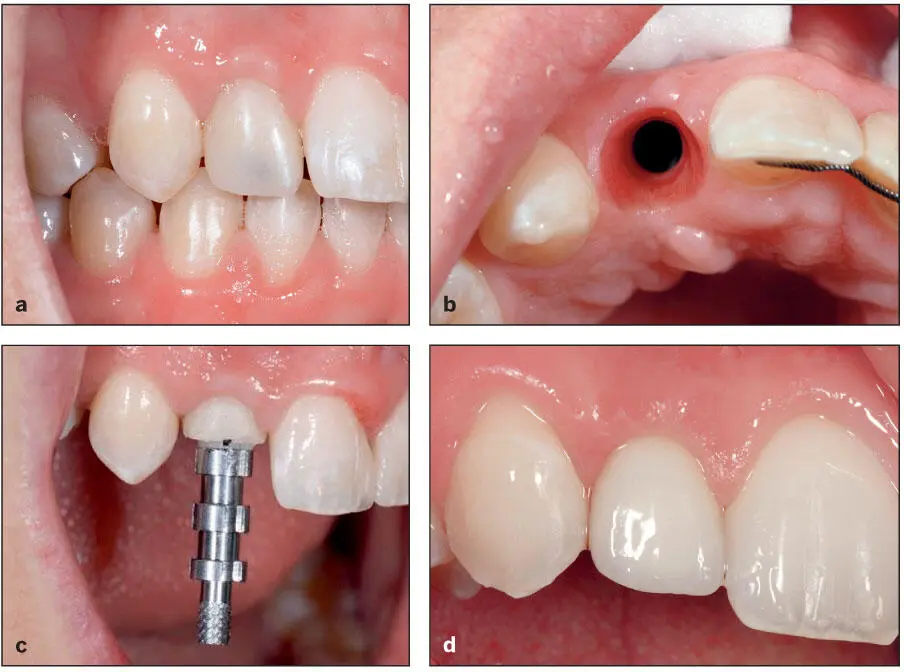
Fig 1-10 (a and b) A provisional implant crown was fabricated and altered as necessary to refine the peri-implant soft tissue contours. (c) A customized impression coping was used to make the definitive impression. (d) The definitive restoration.
Recent Innovations, Clinical Trends, and Impact
Several innovations have been introduced into clinical practice in recent years. The number of patients now considered suitable candidates for implant treatment has expanded dramatically because of the bioreactivity of modern implant surfaces and of our ability to enhance the bone and soft tissues of the potential implant sites. In addition, improved site evaluation with CBCT scans and the accompanying software, tilted implants, guided implant surgery, improved prosthodontic designs, the introduction of new materials, and a better understanding of the limitations of the prosthodontic materials previously used in conventional dentistry when used for implant prostheses have improved implant success rates and prosthesis predictability.
Impact of 3D imaging and CAD/CAM on diagnosis, treatment planning, surgical planning, surgical placement, and prosthesis fabrication
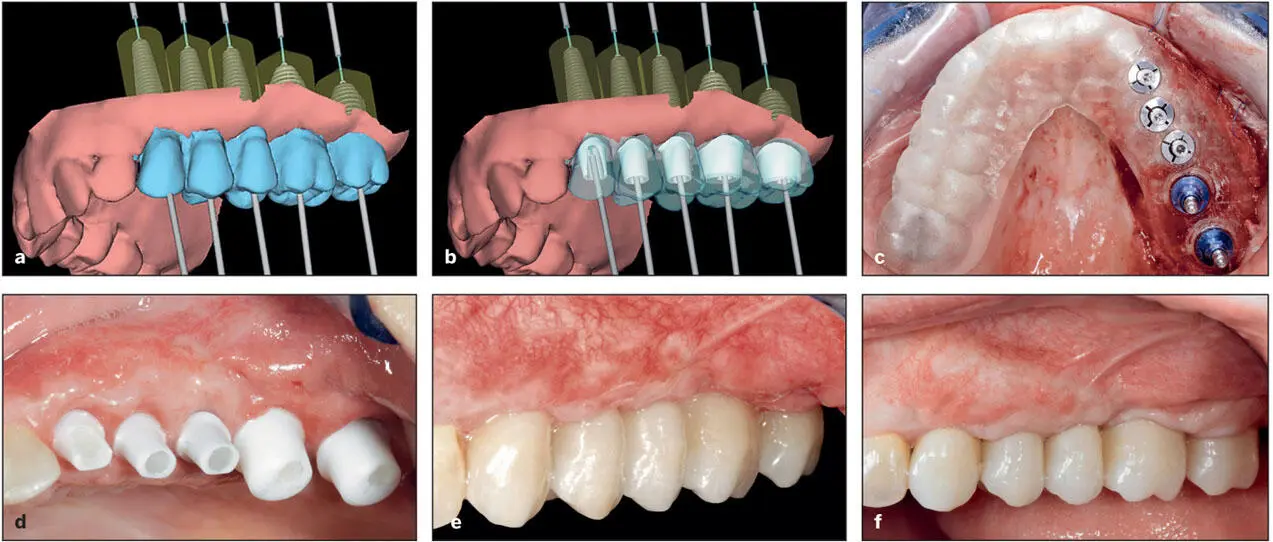
Initially, the workup of potential implant patients was surgically driven; that is, the suitability of a patient was determined primarily by the 3D volume and quality of the bone sites. Today, the development and the improving sophistication of CBCT scans and CAD/CAM programs permits the workup to be driven by the needs of the prosthetic design. With these tools, clinicians are able to identify vital structures such as the inferior alveolar nerve, determine the 3D nature of the potential implant bone sites, predetermine implant position and angulation with great precision, and fabricate surgical stents and surgical drill guides that allow placement of implants into their intended positions via semiguided or fully guided surgery ( Fig 1-11). In addition, CAD/CAM systems allow for the design and manufacture of customized implant connecting bars, custom abutments, provisional restorations, and now, definitive restorations with great precision (see Fig 1-11). All those who practice implant dentistry should become intimately familiar with these technologies.
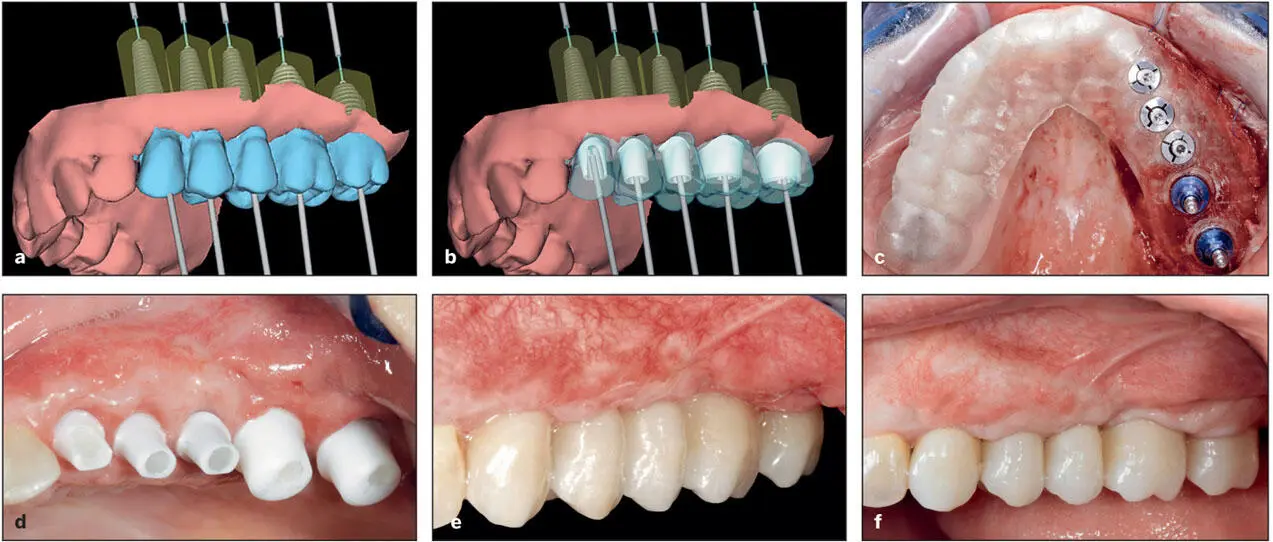
Fig 1-11 A computer-guided approach enables the implant team to (a) design a provisional prosthesis and determine the positions of the implants, (b) design and manufacture abutments and fabricate a provisional prosthesis, and (c) fabricate the surgical template prior to implant surgery. (d) The customized abutments. (e) The provisional prosthesis. (f) The definitive prosthesis. (Courtesy of Dr A. Pozzi.)
Impact of changes in the design of the implant body and the implant platform (ie, interface between abutment and implant fixture)
Several new implant designs have been introduced, and the impact of these designs will be addressed in this new edition. For example, recently there has been increased use of self- tapping implant designs ( Fig 1-12). These are used primarily in poor-quality bone sites (poor density), such as the posterior maxilla. Another innovation is the development of tapered implants designed specifically for immediate loading. With these two design changes, during insertion of the implant, the trabecular bone of the implant site is compressed around the implant, leading to improving primary stability of the implant. As a result, in select patients the improved initial anchorage allows for immediate loading or immediate provisionalization.

Fig 1-12 A variety of implant shapes, thread patterns, and implant platforms are available.
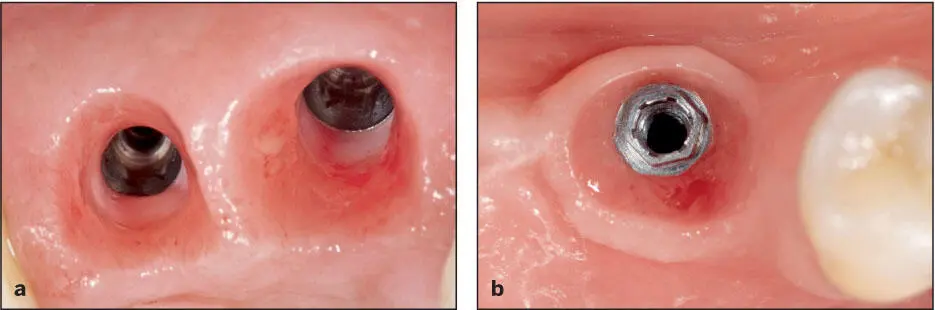
Manufacturers continue to introduce new implant platform designs. However, the clinical impact of these design changes is rarely addressed. As a result, restorative dentists must increase their inventories of prosthetic components. A good example is the continuing debate regarding the use of external hex versus internal locking systems ( Fig 1-13). The nature of the implant-abutment connection may be clinically significant when restoring single-tooth defects but probably not when restoring multiple-tooth defects. Single implants, especially in the posterior regions, are subjected to significant occlusal forces. The lateral component of these forces may be sufficient to widen the microgaps between the abutment and the implant during function in the external hex designs. Some have speculated that this may be detrimental to the long-term survivability of the implant and the restoration. However, clinical reports do not support this hypothesis. 36, 37These issues are probably not clinically significant when multiple implants are splinted together when restoring posterior quadrants or fabricating full-arch restorations where multiple implants are splinted together across the arch. 36
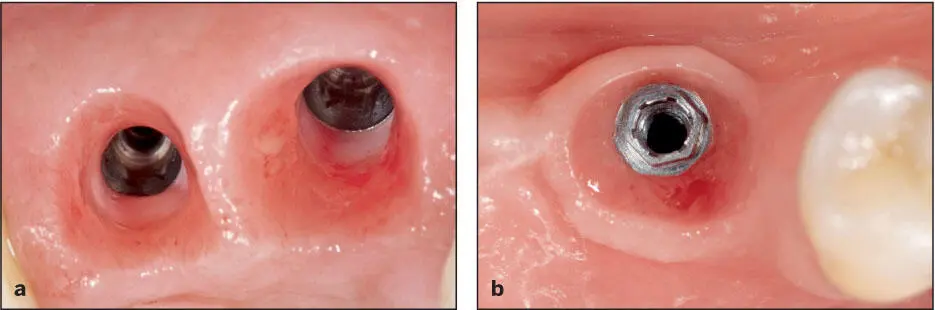
Fig 1-13 Implant platform designs. (a) Internal interlocking system. (b) External hex system.
Likewise, the impact of platform reduction is still far from settled. Some authors have hypothesized 38that using designs where the diameter of the abutment is less than that of the head of the implant fixture horizontalizes the epithelial attachment 39and may also redirect the stresses away from the crestal bone–implant interface, 40and as a result of these phenomena, such designs will reduce the rate of crestal bone loss ( Fig 1-14). The clinical evidence for this claim is not convincing, 41and randomized clinical trials have failed to demonstrate a benefit of platform reduction with respect to maintenance of crestal bone levels. 42

Fig 1-14 Platform reduction. The diameter of the abutment as it emerges from the implant is less than the diameter of the neck of the implant.
Impact of surgical innovations
Widening the alveolar ridge with bone grafts has become very predictable, and several new techniques have been introduced ( Fig 1-15). The need to maximize the zone of keratinized tissue and retain or restore the interdental papilla has led to the development of many new grafting techniques and flap designs (see Figs 1-15band 1-15c), particularly in the esthetic zone. 43Furthermore, a one-stage technique can be used in select patients, as opposed to burying the implants beneath the mucosa during the healing period. Recent reports have also suggested that fully guided, flapless implant placement in select patients reduces the incidence of surgery-related bacteremia and may be beneficial for patients with medical risk factors that require prophylactic antibiotic coverage 44( Fig 1-16). Many of these techniques are highlighted throughout the book, including in a newly added chapter 19 that discusses basic surgical techniques.
Читать дальше