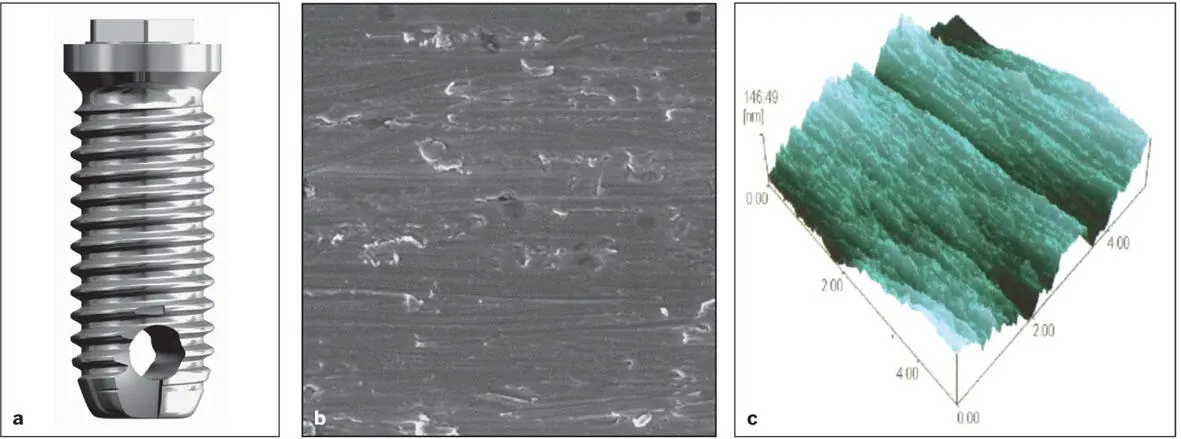
The original dental implants developed by Professor Brånemark and his colleagues were prepared with a machined surface ( Fig 1-4). These machined-surface implants were predictable in bone sites of favorable quantity and quality, such as the mandibular symphysis region, but were problematic when restoring posterior quadrants in partially edentulous patients. Since then, numerous surface treatments (eg, sandblasting, acid etching, titanium grit blasting, electrolytic processes) designed to change the microtopography of the implant surface have evolved that have significantly improved the osteoconductivity of titanium implants, making these implants highly predictable in less favorable sites, such as when restoring the posterior quadrant of the maxilla in partially edentulous patients (see chapter 11).
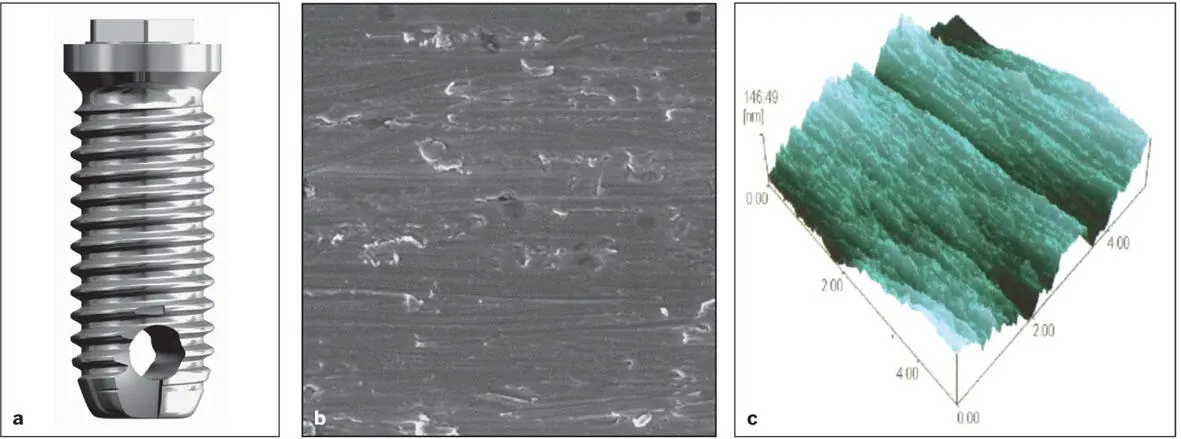
Fig 1-4 (a) The original Brånemark machined-surface implant. (b and c) Machined-surface topography.
Prerequisites for Achieving Osseointegration
Uncontaminated implant surfaces
The osteoconductivity of implant surfaces is impaired if they become contaminated with organic molecules; if this occurs, the surface charge is changed from positive to negative, the surface becomes less wettable, and upon implant placement, adsorption of plasma proteins is inhibited. However, implant surfaces can be decontaminated by exposure to ultraviolet light. 9, 10Decontaminating implant surfaces with ultraviolet light (photofunctionalization; see chapter 2) enhances adsorption of plasma proteins initially after implant placement and promotes more rapid differentiation of mesenchymal stem cells into osteoblasts once they reach the surface of the implant.
Creation of congruent, nontraumatized implant sites
Careful preparation of the implant site is important to obtaining osseointegration of a titanium implant in bone on a consistent basis ( Fig 1-5). In an ideal situation, the gaps between the wall of the osteotomy and the implant are small, the amount of damaged bone created during surgical preparation of the bone site is minimal, and the implant remains immobilized during the period of bone repair. Under these circumstances, the implant becomes osseointegrated a very high percentage of the time (95% or greater with the modern microrough implant surfaces). During surgical preparation of the site, excessive bone temperatures (ie, above 47ºC) should be avoided because they create a zone of necrotic bone in the wall of the osteotomy site, which leads to impaired healing and an increased likelihood of a connective tissue interface forming between the implant and the bone (see Fig 1-5).

Fig 1-5 (a) Semiguided surgical drill guide. Note the bushings (drill sleeves) incorporated within the drill guide. (b) Implants are being placed. (c) Implants in position.
A similar outcome is seen if excessive torque is employed to improve initial implant stability or if osteotomes are used to compress the bone adjacent to the osteotomy site in order to achieve a similar outcome (so-called “osteodensification”). Excessive compression of the bone adjacent the osteotomy site increases its density but does not improve initial implant anchorage. This practice results in cell death and increases the width of the zone of necrotic bone adjacent to the osteotomy site. Within 1 day of implant placement, the condensed bone interface exhibits microfractures and osteoclast activity. The subsequent resorption of this zone of necrotic bone around the circumference of the implant increases the dip in implant anchorage seen 7 to 10 days following initial implant placement and if the implant is loaded immediately, theoretically increases the likelihood of implant failure. 11, 12Finite element modeling, mechanical testing, and immunohistochemical data collected at various time intervals during the osseointegration period have shown that osteodensification results in excessive interfacial strains, marginal bone resorption, and no improvement in implant stability. 12
Primary implant stability
Osseointegration is obtained more consistently when initial primary stability of the implant is achieved in the surrounding bone. This is particularly important when one-stage surgical procedures are employed, and is obviously necessary if the implant is to be immediately placed into function (ie, immediate loading or immediate provisionalization). In attempting to establish initial primary stability, often the implant site is underprepared when the bone is porous or soft. If the implant is not stable in its prepared osteotomy site, many clinicians prefer to replace it with an implant of a slightly larger diameter. This was particularly necessary when machined-surface implants were routinely employed. Today, implant surfaces are considerably more bioreactive, and unstable implants (so-called “spinners”) have a reasonable chance of achieving osseointegration when the wound is closed primarily and as long as the clot remains undisturbed during the initial period of healing.
Appropriate initial implant stability is especially essential when considering immediate loading or immediate provisionalization (ie, inserting a prosthesis at the time of implant placement). Recently, an increasing number of implant companies are introducing thread designs with aggressive pitch and drill sequences that result in bone compression. Some of these systems require high insertion torque. However, as mentioned previously, excessive insertion torque appears to actually delay healing and may compromise the quality of implant bone anchorage ultimately achieved. 11, 12These studies have generated considerable debate because previously, many clinicians maintained that high torque values were beneficial and resulted in improved initial implant stability, which in turn led to better outcomes when implants were immediately loaded or immediately provisionalized with a prosthesis. 13, 14According to Cha et al 11and Wang et al, 12excessive compression of trabecular bone associated with higher torque levels leads to a relatively thick layer of damaged necrotic bone abutting the surface of the implant, and this layer must be resorbed before contact osteogenesis can begin. This is not surprising because it known that high compressive forces shut off angiogenesis and local microvascular blood flow, and the resultant biochemical cascades of cytokines and cellular reprograming leads to bone resorption. In fact, compressive stress on the leading edge of orthodontic tooth force vector is responsible for bone remodeling that is necessary for successful orthodontic movement. The data in this study is also consistent with the findings of many clinicians, who have recorded significant decreases in implant stability levels 7 to 10 days following implant placement. 15The levels rebound, but the patient is instructed to avoid mastication for the first 6 weeks following implant placement, and restorative dentists are advised to avoid manipulations of the prosthesis for at least 12 weeks. 16
Implant stability during the healing phase
It was thought that micromovement of the implant could disturb the tissue and vascular structures necessary for initial bone healing. 17Furthermore, excessive micromovement of the implant during healing was thought to induce the detachment of the fibrin clot from the implant surface. Actually, it is well known that an optimal amount of strain is beneficial and necessary for most cellular function, from neurons to cardiac cells to osteoblasts and many more. Each cell type is known to respond to stress state (compression, tension, shear) and strain magnitude. The Frost model 18, 19describes a range of optimal microstrain that promotes osteoblast bone remodeling and homeostasis. When insufficient microstrain exists, the bone cells can actually stop producing bone, leading to an osteoblast/osteoclast imbalance. Furthermore, a slight increase above the optimal strain range can promote bone deposition. However, excessive microstrain can lead to necrosis and resorption. The healing processes are highly dependent on the microstrain status. Excessive micromovement tends to produce a connective tissue–implant interface (fibro-osseointegration), while appropriate microstrain can promote a healthy bone-implant interface. These phenomena have clinical significance. For example, immediate loading of dental implants provides a unique challenge. Implants placed into function immediately must be sufficiently stable so as to reduce micromovement to physiologic levels during healing. Otherwise, the implant may fail to osseointegrate.
Читать дальше