Sean Gallagher - Musculoskeletal Disorders
Здесь есть возможность читать онлайн «Sean Gallagher - Musculoskeletal Disorders» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Musculoskeletal Disorders
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Musculoskeletal Disorders: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Musculoskeletal Disorders»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Hands-on guidance and tools for the prevention of musculoskeletal injuries in the workplace Musculoskeletal Disorders: The Fatigue Failure Mechanism,
Musculoskeletal Disorders: The Fatigue Failure Mechanism
Musculoskeletal Disorders — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Musculoskeletal Disorders», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Osteocytes are believed to be the bone‐sensing cells involved in mechanotransduction and thus the key regulators of bone remodeling. The gap junctions mentioned earlier aid in this function. Also, the osteocyte cell membrane is surrounded by interstitial fluid and extracellular matrix in which microtubules are embedded in order to transmit extracellular matrix mechanical changes to the osteocyte’s actin filaments (Bakker et al., 2009). Osteocytes also communicate with surrounding cells via the release of biochemical factors and signaling molecules, such as bone morphogenetic proteins (BMPs), prostaglandin E2 (PGE2), and nitric oxide (NO) (Klein‐Nulend, Bacabac, & Bakker, 2012).
Osteocytes are also actively involved in maintaining the bony matrix. They express osteoblast stimulating factor‐1 after mechanical or muscular loading (Klein‐Nulend & Bonewald, 2008). Osteocytes send inhibitory signals to osteoclasts to prevent bone loss during normal loading (Nakashima et al., 2011). Local damage (microcracks) of the osteoid matrix can compromise the osteocyte environment, disrupting the fluid flow, consequently reducing nutrients and oxygen supply to the embedded cells and creating oxidative stress (Al‐Dujaili et al., 2011).
Osteoclasts—reallocate and remodel bone
Osteoclasts differentiate after the fusion of bone marrow‐derived mononuclear precursor cells of the monocyte–macrophage lineage in a process termed osteoclastogenesis. Osteoclasts are large multinucleated cells with a ruffled bottom in contact with the bone matrix ( Figure 3.17d). They work in concert with osteoblasts in the constant turnover and remodeling of bone. They do this via their ability to secrete hydrochloric acid and other degradative enzymes, which, once activated, dissolve the bone matrix, creating a resorption pit underneath the cell. Osteoclasts are regulated by parathyroid hormone, calcitonin (from the thyroid gland), and pro‐inflammatory cytokines (Boyce & Xing, 2007; Brabnikova Maresova, Pavelka, & Stepan, 2013; Nakashima & Takayanagi, 2011). As mentioned earlier, osteoclast activation is also mediated by the binding of osteoblast or osteocyte produced RANKL (a protein that plays an essential role in the recruitment, differentiation, activation, and survival of osteoclasts) (Burgess et al., 1999). Estrogen has a dual effect: Its presence increases bone formation and reduces bone resorption by enhancing osteoblast proliferation and function (Ernst, Heath, & Rodan, 1989; Majeska, Ryaby, & Einhorn, 1994); it also reduces bone turnover by reducing osteoclast activity (Hofbauer et al., 1999).
Extracellular matrix
Bone is a material constructed of a flexible collagenous matrix that is intermingled with rigid mineral crystals. Thus, bone is harder and less pliable than tendons or cartilage. The extracellular matrix of bone is produced by osteoblasts and consists of inorganic and organic components. For example, osteoid is defined as the unmineralized, organic portion of the bone matrix that forms prior to the maturation of bone tissue; it is composed primarily of collagen type I. In both unmineralized and mineralized bone, the organic component of bone (40% of bone’s dry weight) include collagen type I fibers (90% of the organic matrix and ~97% of the collagenous proteins) and a number of noncollagenous proteins, such as osteocalcin and bone sialoprotein, which may orchestrate mineralization (Hu, Peel, Ho, Sandor, & Clokie, 2009; Robey et al., 1993). The inorganic component of bone represents about 60% of the dry weight of bone matrix and is composed mainly of abundant calcium and phosphorus, as well as smaller amounts of bicarbonate, citrate, magnesium, potassium, and sodium. Calcium forms hydroxyapatite crystals with phosphorus, although it is also present in an amorphous form (Junqueira & Carneiro, 2005; Khurana, 2009). Calcium hydroxyapatite crystals are arranged parallel to collagen fibers. This orientation maximizes the collagen’s resistance to tensile (stretch) forces and calcium hydroxyapatite’s resistance to compressive forces (Gartner & Hiatt, 2007; Sela, Amir, Schwartz, & Weinberg, 1987). In life, bones also have a large amount of water (~25% of the total bone weight) (Ailavajhala, Oswald, Rajapakse, & Pleshko, 2019; Ailavajhala, Querido, Rajapakse, & Pleshko, 2020).
Organization
According to their anatomical shape, bones are classified into four general categories: long, short, flat, and irregular bones. We will focus here on long bones. Long bones have two extremities (epiphyses), a cylindrical tube in the middle (diaphysis, also known as shaft of the bone), and a transitional zone between them (metaphyses) ( Figure 3.18). The epiphysis is the expanded end of the bone that is covered by articular cartilage. The metaphysis is the junctional region between the epiphysis and the diaphysis and includes the growth plate (physis). The diaphysis is the shaft of long bones and is located in the region between metaphyses. The growth plate is a zone of endochondral ossification (cartilage‐to‐bone conversion) that mediates growth in bone length in an actively growing cartilage‐to‐bone region (Yang, 2010).
Bone tissue can also be classified by texture, matrix arrangement, maturity, or developmental origin (Yang, 2010). There are two main subtypes of bone: cortical and trabecular bone. Both types are chemically identical, but differ in terms of their structure, arrangement, and cell density. Approximately 80% of bone is cortical bone, with the remainder as trabecular bone (Carter & Hayes, 1977).
Trabecular bone (also known as cancellous or spongy bone) has numerous cavities ( Figure 3.18). It is found mainly at the ends of many long bones and in areas like the ears and nose (Cooper, Milgram, & Robinson, 1966). Individual trabeculae are extensively connected and are oriented along the lines of mechanical stress on the bone in question. Trabecular bone is more metabolically active than cortical bone because of its much larger surface area for remodeling.
Cortical bone is dense in texture with few or no cavities, although it does contain pores for blood vessels, for example ( Figures 3.18and 3.19). Cortical bone is typically seen as the hard outer shell that surrounds trabecular bone or the centrally located marrow cavity. It is surrounded externally and internally by a periosteum and endosteum, respectively (Yang, 2010). Cortical bone is organized into Haversian systems or osteons ( Figure 3.19), in which the lamellae are concentrically organized around a vascular canal, the Haversian canal. The blood supply of cortical bone enters from the periosteum via Volkmann canals, which also connect Haversian canals with each other (Brooks, 1963).
Lamellar bone is mature bone in which collagen fibers are arranged in parallel. It is located in both trabecular bone and cortical bone, the latter concentrically organized around a vascular canal.
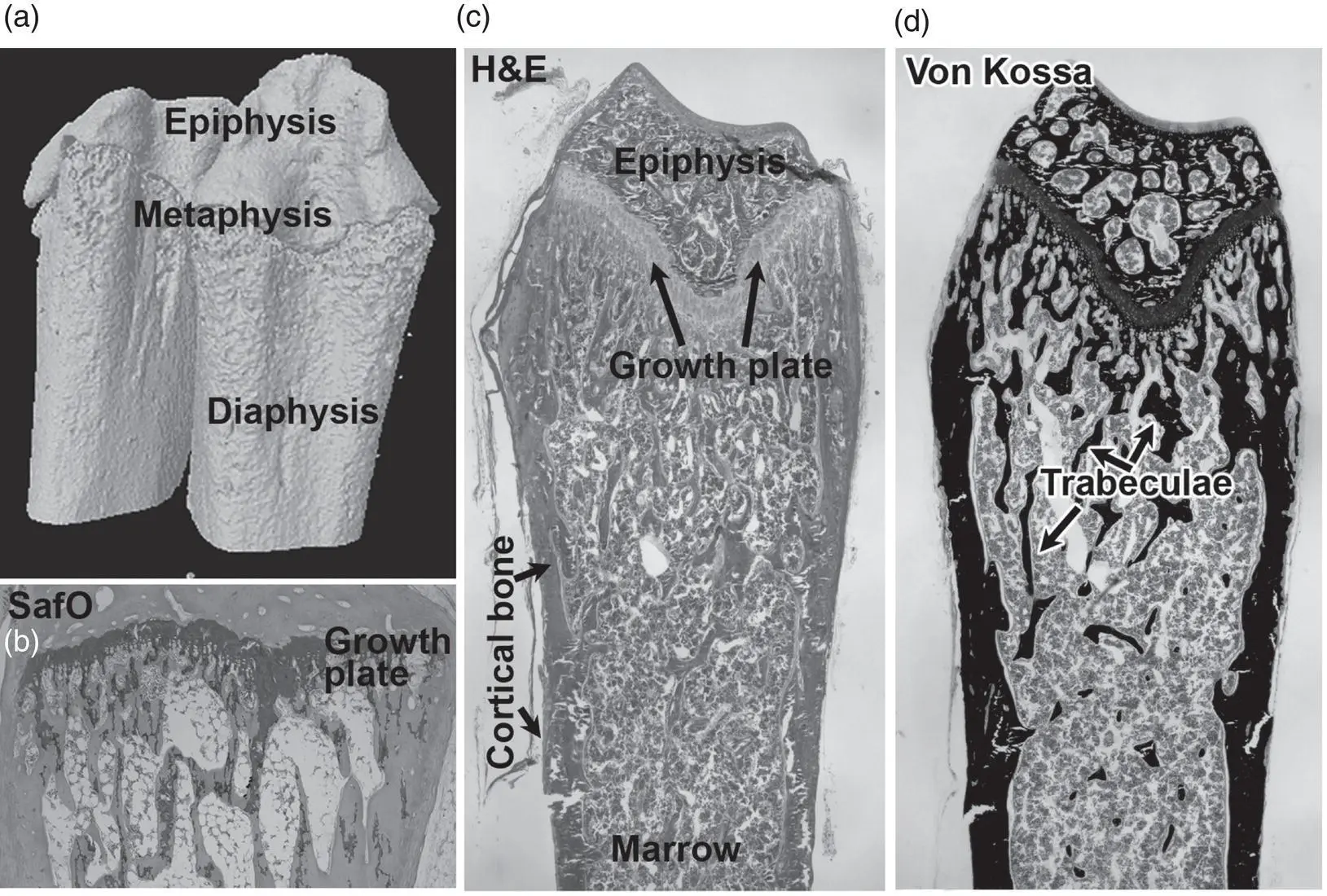
Figure 3.18 The organization of long bones. (a) Three‐dimensional micro computed tomographic image of a rat’s radius and ulna bones at the level of the wrist. (b) Staining a section of the radius with safranin O (Saf O) shows the location of cartilage in the epiphyseal plate (growth plate) and trabecular bone). (c) Hematoxylin and eosin staining showing the location of the growth plate proximal to the epiphysis, trabecular bone within the bone marrow region, and denser cortical bone on the outer edge of the bone. (d) Von Kossa staining of calcified trabecular and cortical bone.
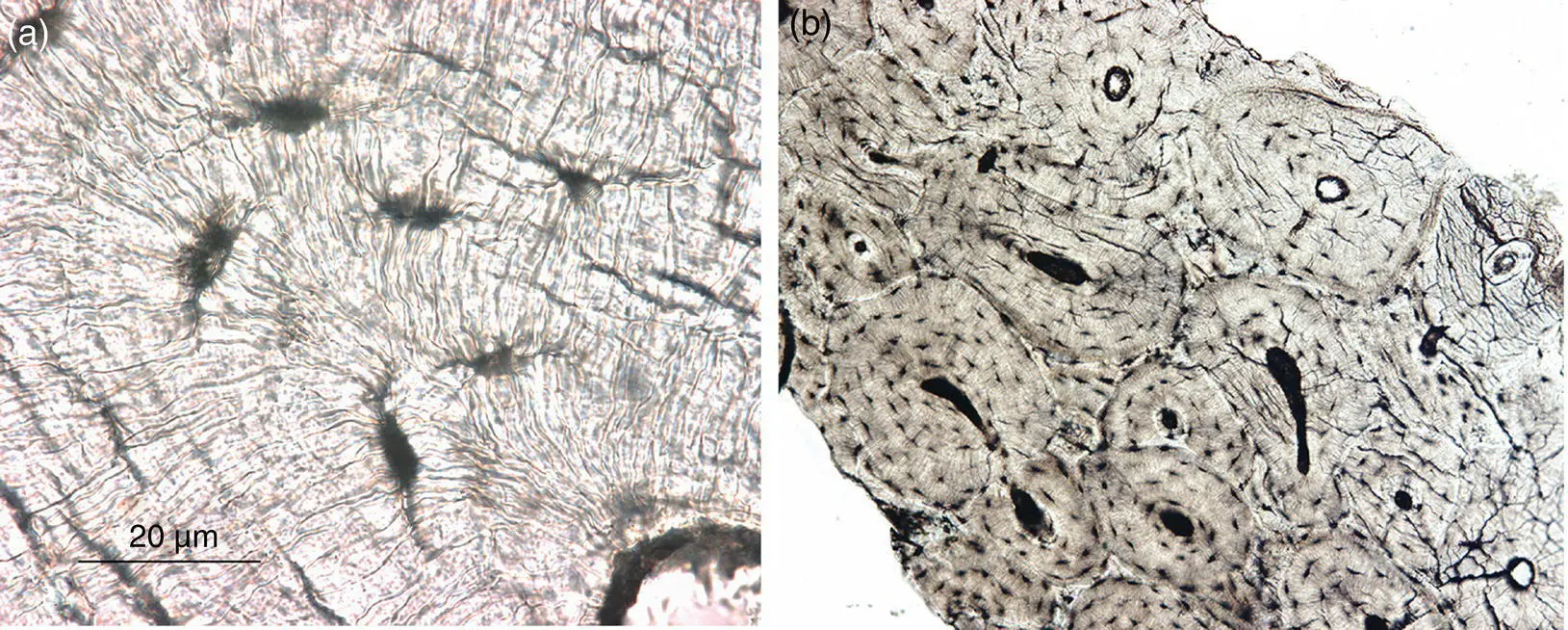
Figure 3.19 Osteons in cortical bone. (a) The osteocytes canaliculi are visible in the osteon. (b) Complete osteons (complete circles) and partial osteons left from past remodeling events are shown.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Musculoskeletal Disorders»
Представляем Вашему вниманию похожие книги на «Musculoskeletal Disorders» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Musculoskeletal Disorders» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.
![Ally Carter - [Gallagher Girls 02 ] - Cross My Heart & Hope To Spy](/books/262178/ally-carter-gallagher-girls-02-thumb.webp)


![John Bruce - The Lettsomian Lectures on Diseases and Disorders of the Heart and Arteries in Middle and Advanced Life [1900-1901]](/books/749387/john-bruce-the-lettsomian-lectures-on-diseases-and-disorders-of-the-heart-and-arteries-in-middle-and-advanced-life-1900-1901-thumb.webp)