6.4 Symptoms and signs of shock
The signs and symptoms seen in the various forms of shock are primarily due to organ dysfunction resulting from inadequate tissue perfusion. The presentation is also partly influenced by the pathology causing the shock syndrome.
This is the most common form of shock encountered on the labour ward. The signs of hypovolaemia are:
Fetal heart rate abnormalities
Increase in maternal heart rate
Cold, pale, sweaty, cyanosed skin with delayed capillary refill
Alteration of mental state
Tachypnoea
Fall in urine output
Narrowed pulse pressure
Hypotension (late sign)
An increase in the heart rate occurs in compensation for hypovolaemia (1000–1500 ml blood loss) or vasodilatation, both of which can cause hypotension and shock. A maternal heart rate of more than 100 beats/min should be considered sinister, until proven otherwise. Most, but not all, women will become tachycardic if bleeding significantly, but paradoxical bradycardia also occurs. Vagal stimulation caused by cervical stimulation (e.g. products in the os) or peritoneal irritation can produce bradycardia profound enough to cause shock. Medications such a beta‐blockers and labetalol (alpha‐ and beta‐blocker) will prevent a tachycardic response to hypovolaemia and this may be falsely reassuring in the assessment of the bleeding patient.
Skin, capillary refill, mental state and urine output
The skin, kidneys and brain can be thought of as ‘end organs’ that reflect the adequacy of perfusion to tissues.
Capillary refill time (CRT)
This is an indication of skin perfusion. It can be assessed by compressing a fingernail, or pressing on the sternum, for 5 seconds. The test is normal if colour returns within 2 seconds of releasing compression (i.e. a CRT of less than 2 seconds – the time taken to say the words ‘capillary refill’). If the patient is in a cold environment, CRT, especially peripherally, will be unreliable.
If the woman is conscious and talking sensibly, she is not only breathing through an open airway, she is perfusing her cerebral cortex with sufficient oxygenated blood (50% of the normal cardiac output). Increasing hypovolaemia and subsequent cerebral hypoperfusion cause alterations in the level of consciousness. These alterations may begin with agitation and, if untreated, may proceed through confusion and aggression to eventual unresponsiveness and death.
This is caused by an increase in diastolic blood pressure, that reflects vasoconstriction occurring due to endogenous catecholamine release as a compensation for hypovolaemia.
The sign most commonly referred to in the context of shock, hypotension, is a very late sign in the obstetric population, developing only when significant blood loss has occurred. A successful outcome for the patient depends on the early recognition of shock, restoration of volume and control of haemorrhage.
Recognition of hypovolaemia
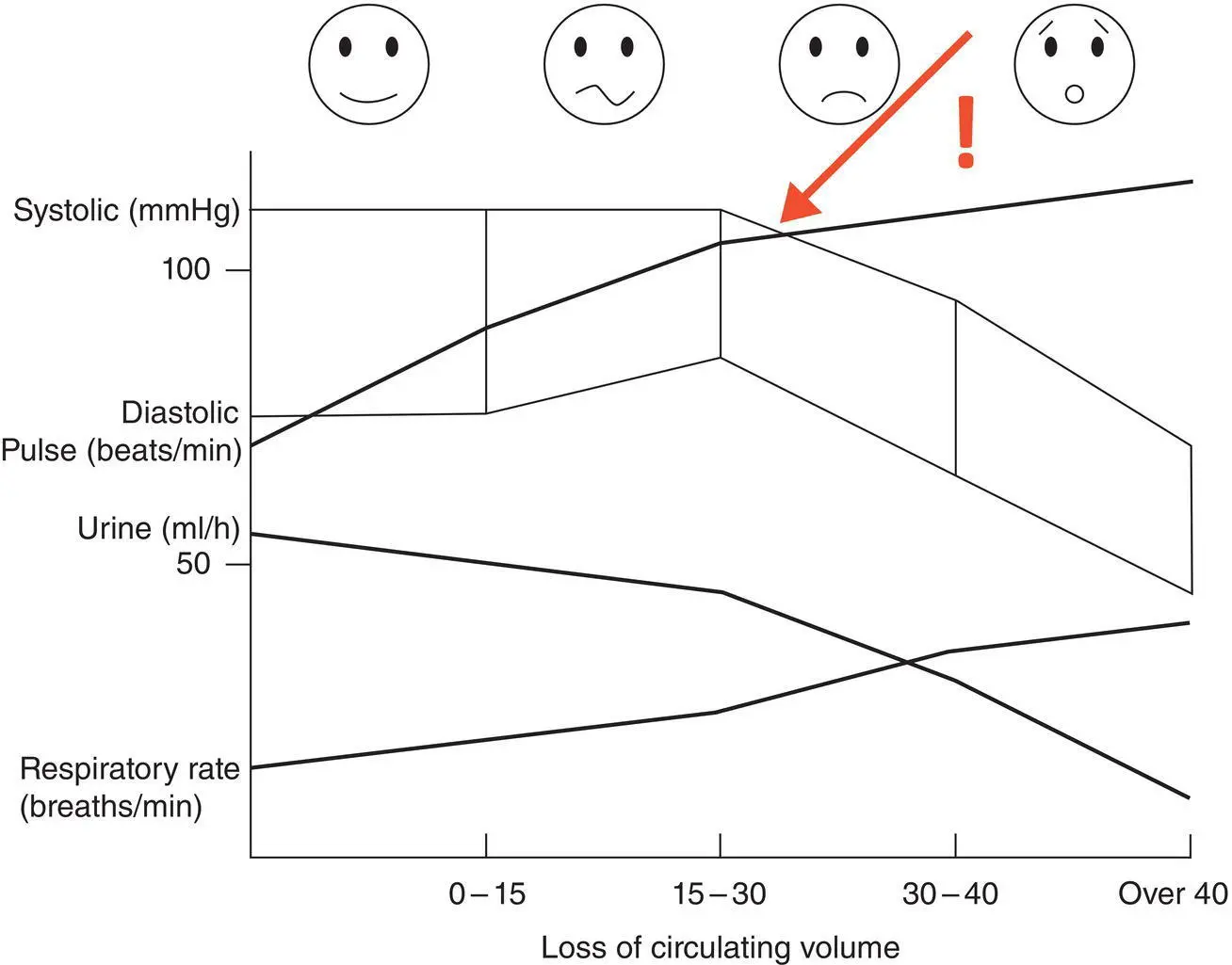
Maternal blood loss can be categorised into four classes of severity, as shown in Table 6.1and graphically in Figure 6.2.
To remember the different percentages in these classes of blood loss, think of the way of scoring in a tennis match!
Figure 6.2illustrates the various clinical signs seen in ongoing acute blood loss suffered by a pregnant woman related to the volume lost. The point where the pulse rate is a higher number than the systolic blood pressure is a sign of significant decompensation.
Table 6.1 Severity of blood loss during maternal haemorrhage
| Class |
Loss of circulating volume (%) |
Blood loss in a 70 kg pregnant woman (ml) |
Signs and symptoms |
| I |
0–15 |
<1000 |
Fully compensated due to blood diversion from the splanchnic pool. No symptoms. Minimal tachycardia is likely to be the only abnormal sign. No treatment needed in an otherwise healthy woman as long as the bleeding has stopped |
| II |
15–30 |
1000–2000 |
Peripheral vasoconstriction maintains systolic blood pressure. The woman may be aware of increased heart rate and may display agitation or aggression. Narrowed pulse pressure and tachypnoea are the keys to early detection, as heart rate is only modestly increased and systolic blood pressure remains normal. Peripheral vasoconstriction maintains blood pressure. Requires crystalloid fluid replacement |
| III |
30–40 |
2000–2700 |
Cardiovascular system shows signs of decompensation. The woman will look unwell. Tachycardia, tachypnoea, changes in mental status, fall in systolic blood pressure. Will require crystalloid and potential blood transfusion |
| IV |
>40 |
>2700 |
Immediately life threatening. Tachycardia, fall in blood pressure, altered mental status, evidence of negligible urine output. Loss of >50% results in loss of consciousness, requiring immediate ‐surgery as well as massive transfusion |
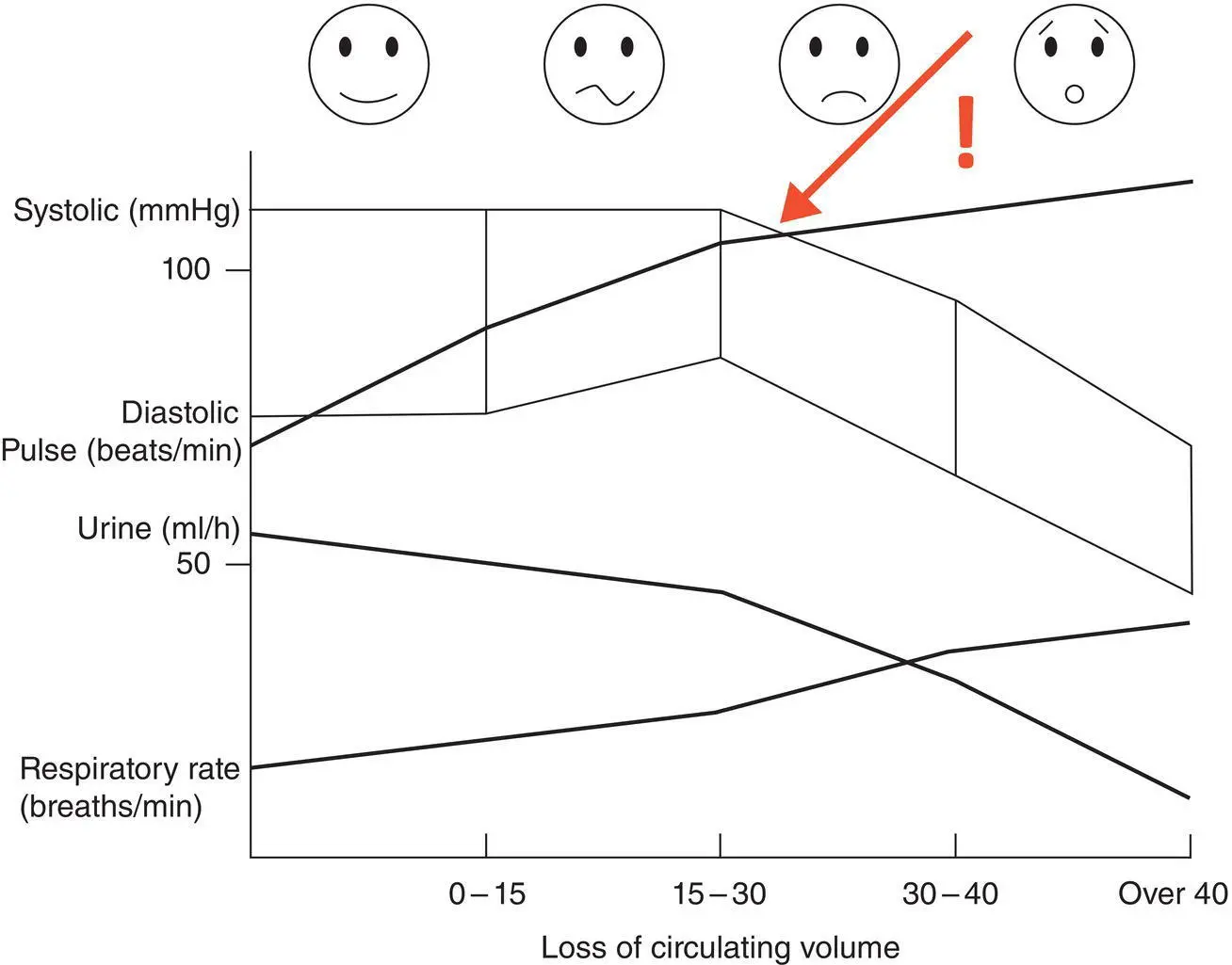
Figure 6.2 Clinical parameters following increasing blood loss in the pregnant and postpartum woman
Pitfalls in the recognition of shock in pregnancy
Some pregnant women do not mount a tachycardia, or can even produce a bradycardia. This can be paradoxical, due to vagal stimulation [see above] or if the woman is taking beta‐blocker medication
Women with pacemakers have a fixed upper heart rate
Athletes may have a very slow baseline heart rate
Haemoglobin concentration is a useful measure of blood loss, only after there has been fluid resuscitation
During the acute phases of loss, the haemoglobin concentration will not change. Rapid movement of fluid from the extracellular to the intravascular compartment and intravenous clear fluids, will result in a fall in haematocrit. A falling haematocrit may be the only indicator of a slow steady bleed. A rapidly falling haematocrit associated with early signs of hypovolaemia is suggestive of severe loss.
6.5 Principles of treatment
Hypovolaemic shock
Primary survey and resuscitation should be carried out according to the ABC principles. See Chapter 10for the management of A and B.
A diagnosis of hypovolaemic shock must be promptly followed by:
Restoration of adequate oxygen delivery to the tissues by restoration of adequate circulating volume and adequate oxygen carrying capacity (see Chapter 8for intravenous fluids)
Stopping the bleeding (see Chapter 28for major obstetric haemorrhage)
Consider haemorrhage to be of two types:
Compressible
Non‐compressible
Compressible haemorrhage is controllable by direct pressure, limb elevation, packing, by reduction and immobilisation of fractures or, in obstetric situations, compression of the uterus.
Non‐compressible haemorrhage occurs in a body cavity (chest, abdomen, pelvis or retroperitoneum). See Chapters 17, 18and 21for haemorrhage in trauma.
Septic shock complicating delivery may be caused by infection from the genital tract, but can occur with any source of infection, for example a urinary tract or chest infection.
Читать дальше