Normal values for both the non‐pregnant and the pregnant state are given in Table 5A.1. To interpret a blood gas, review the following:
Check PaO2 (normal values 11–13 kPa ON AIR): if it is low, then the patient is hypoxaemic
Check the pH value: to determine the direction of primary change (normal, acidosis or alkalosis); compensation is always incomplete
Check PaCO2, which is determined by breathing (alveolar ventilation): a low PaCO2 (hyperventilation) indicates a respiratory alkalosis or respiratory compensation for a metabolic acidosis; a raised PaCO2 (hypoventilation) indicates respiratory acidosis – note that PaCO2 does not rise to compensate for a metabolic alkalosis
Check standard bicarbonate (the bicarbonate value adjusted to what it would have been if the PaCO2 were normal): if the standard bicarbonate is raised then there is either a metabolic alkalosis or metabolic compensation for a respiratory acidosis; if the standard bicarbonate is low then there is either a metabolic acidosis or metabolic compensation for a respiratory alkalosis
Check base excess: if it is negative then there is a metabolic acidosis; if it is positive then there is a metabolic alkalosis
Table 5A.1 Blood gases in non‐pregnant and pregnant women
|
pH |
PaCO 2 |
Standard bicarbonate |
Base excess |
|
| Normal values |
7.34–7.44 |
4.7–6.0 kPa |
21–27 mmol/l |
–2 to +2 mmol/l |
|
| Values in pregnancy |
7.40–7.46 |
3.7–4.2 kPa |
18–21 mmol/l |
No change |
|
|
Increased |
Decreased |
Decreased |
|
|
| Respiratory acidosis |
↓ |
↑ |
↑ |
+ve |
Hypoventilation leading eventually to compensatory renal retention of bicarbonate |
| Respiratory alkalosis |
↑ |
↓ |
↓ |
–ve |
Hyperventilation leading to renal excretion of bicarbonate |
| Metabolic acidosis |
↓ |
↓ |
↓ |
–ve |
Excess metabolic acid leading to respiratory hyperventilation to compensate Raised lactate in most types of shock |
| Metabolic alkalosis |
↑ |
|
↑ |
+ve |
Excess metabolic alkali but no respiratory compensation compensation |
Appendix 5.2 Radiology in the pregnant woman
Imaging using ionising radiation is often part of the management of seriously ill patients. Patients and healthcare workers are often concerned that the doses of radiation used may be harmful to the fetus ( Table 5A.2). A chest X‐ray confers a minimal amount of radiation to the fetus and is the equivalent of 1 week of background radiation in London. If a chest X‐ray is clinically indicated as a first line investigation in chest pain or breathlessness it should be performed.
Table 5A.2 Safety of different imaging techniques
| Investigation |
Radiation dose (mGy) |
First trimester |
Breastfeeding |
| Chest X‐ray |
<0.01 |
Safe |
Safe |
| CT head scan * |
|
Safe |
Avoid |
| MRI head scan * |
|
Avoid |
Safe |
| CTPA * |
<0.13 |
Safe |
Avoid |
| V/Q scan |
|
Safe |
Avoid |
| CT abdomen * |
|
Safe |
Avoid |
| Ultrasound |
|
Safe |
Safe |
*Express and discard breastmilk for 24 hours if using contrast.
Ultrasound, computed tomography (CT) scans of the head and chest and magnetic resonance imaging (MRI) are safe throughout pregnancy. Gadolinium contrast should be avoided.
For women with suspected pulmonary embolism and a normal chest X‐ray, a lung perfusion scan should be requested in preference to CT pulmonary angiography (CTPA) because the radiation dose to maternal lung and breast tissue is lower.
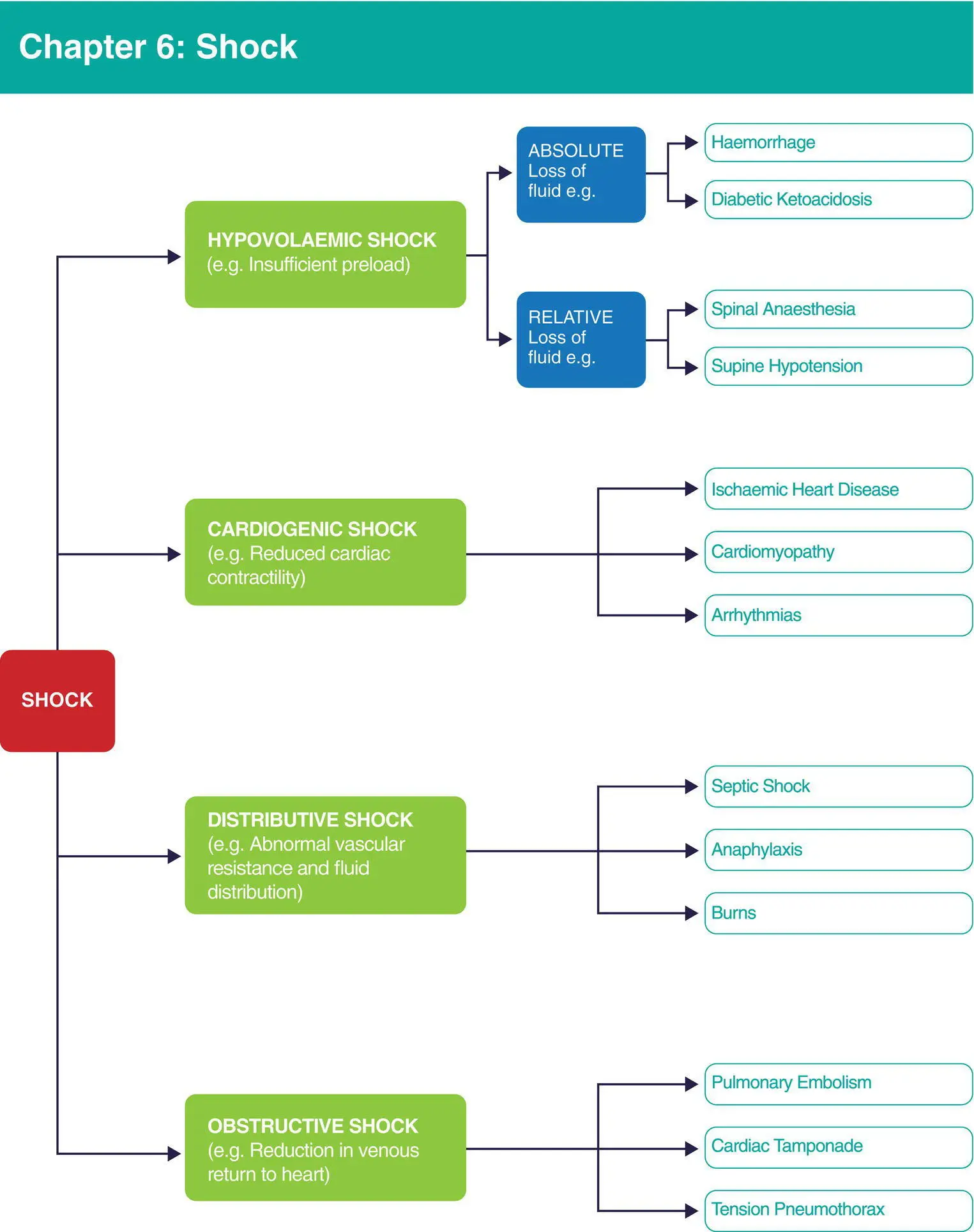
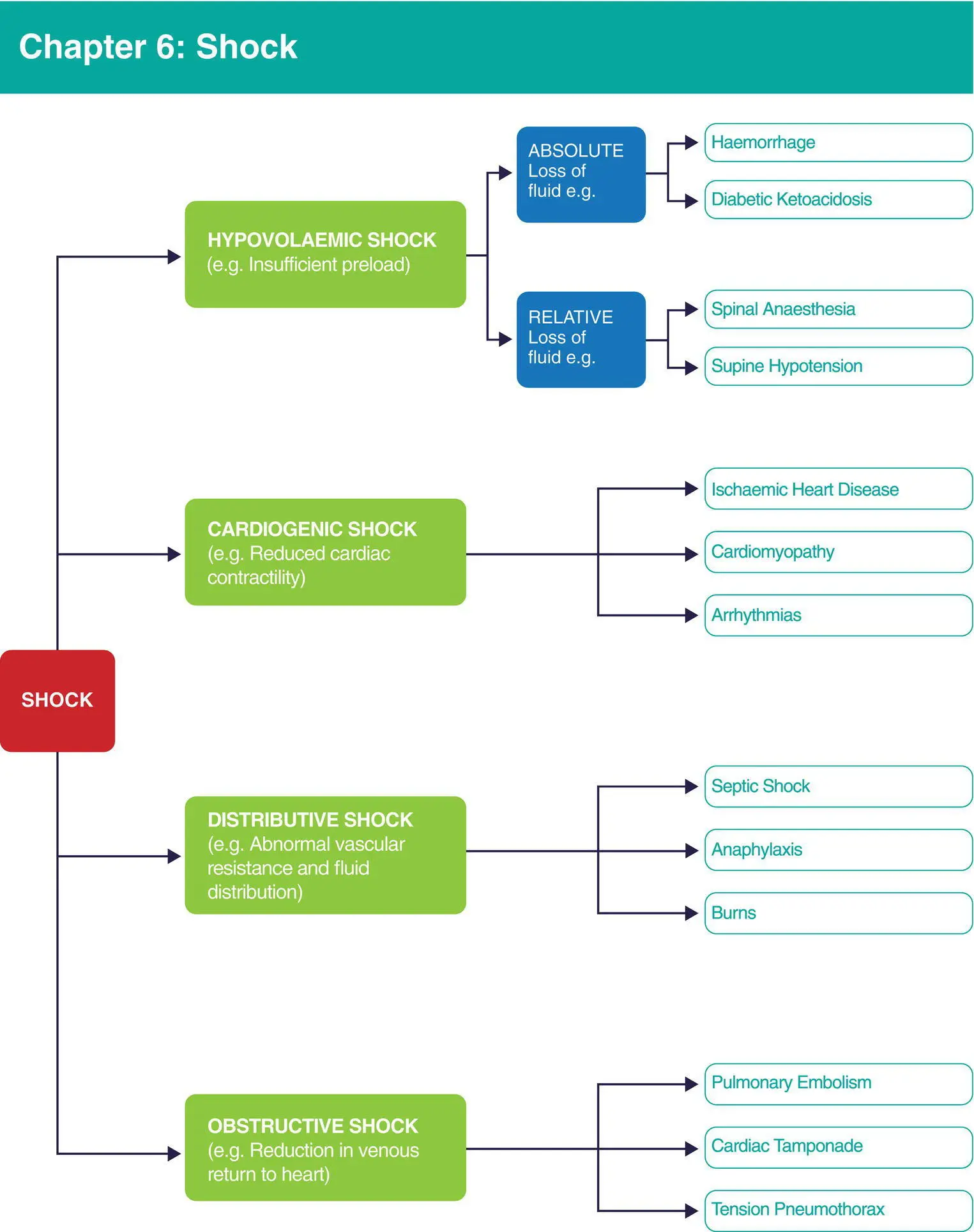
Algorithm 6.1 Shock
After reading this chapter, you will be able to:
Define and recognise shock
Discuss the principles of treatment of hypovolaemic shock
Recognise the physiological changes to the cardiovascular system in pregnancy and how they affect the presentation of hypovolaemic shock
Identify other shock syndromes and understand their management
Shock is defined as a life‐threatening failure of adequate oxygen delivery to the tissues. If left untreated, shock results in sustained multiple organ dysfunction, end‐organ damage and death. It occurs when the cardiovascular response to systemic challenges such as blood loss or sepsis is inadequate.
Decreased blood perfusion of tissues, inadequate blood oxygen saturation or increased oxygen demand from the tissues result in failure of adequate oxygen delivery.
A reduction in cardiac output and a reduction in perfusion pressure will reduce the blood perfusion of tissues. Cardiac output is the product of stroke volume (the volume of blood pumped out of the heart with each beat) and heart rate.
Stroke volume is dependent on preload (filling status), cardiac contractility (pumping strength) and the afterload (vascular resistance – the resistance against which the myocardium has to pump). Shock may result if any of the these components are compromised.
During normal homeostasis, organ perfusion is regulated by local metabolic and microcirculatory factors within a set range of arterial pressures. This is called autoregulation. Beyond this range, blood flow to the organ is primarily determined by the pressure differential between the arterial and venous systems.
The blood supply to vital organs is maintained at lower blood pressures than that to non‐vital organs. In shocked states, blood is preferentially supplied to the brain and the heart at the expense of perfusion elsewhere. Unfortunately for the fetus, the uterus does not count as one of the woman’s vital organs, hence placental blood supply is not maintained in the presence of a life‐threatening challenge to the mother. The resulting fetal compromise is an early and important indicator of maternal shock.
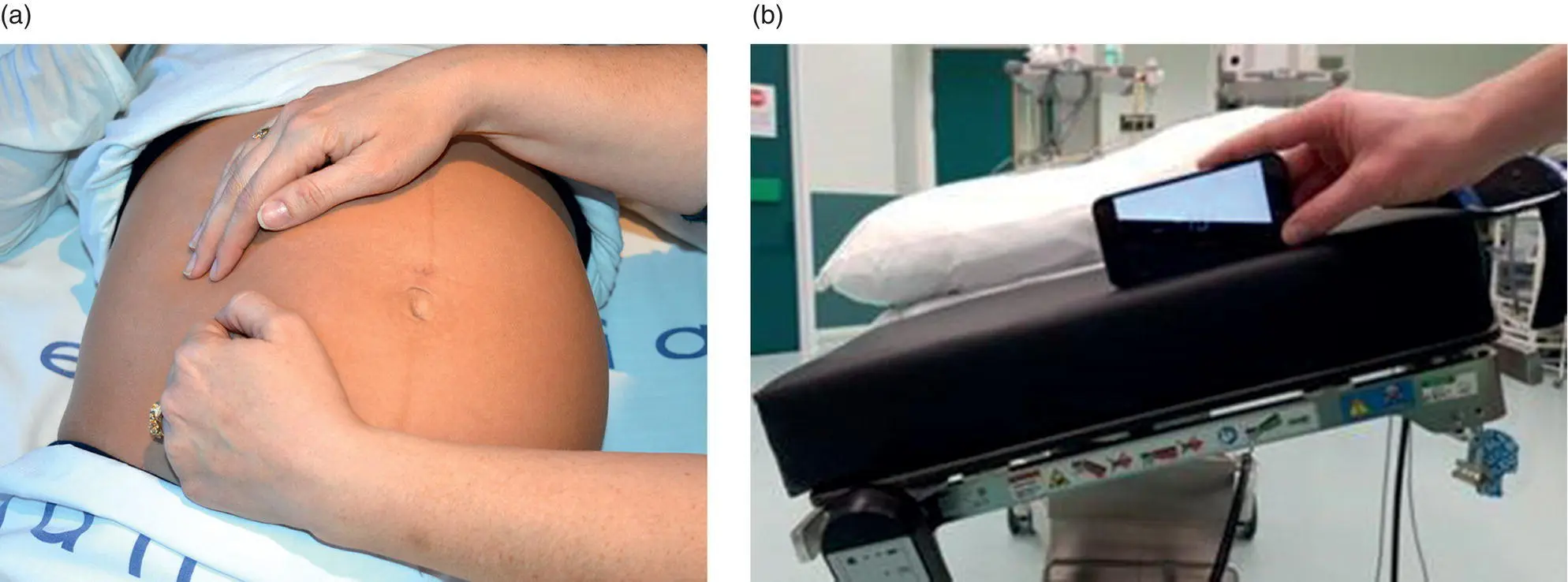
6.2 Aortocaval compression and supine hypotension syndrome
In the pregnant woman in a supine position, the uterus compresses the vena cava, reducing venous return to the heart from 20 weeks’ gestation. Vena caval obstruction and aortic compression can reduce cardiac output by up to 30%. The woman may experience symptoms such as nausea, vomiting or lightheadedness. This is known as supine hypotension syndrome. The reduction in venous return impacts on placental blood flow, which lacks autoregulation.
To prevent the effects of aortocaval compression, the pregnant woman should lie in the lateral position. Although a 15° tilt to the left ( Figure 6.1b) is advocated there is evidence that the effects of compression still occur. Manual displacement of the uterus off the inferior vena cava up and to the left, relieves compression more effectively ( Figure 6.1a). It is important to remember to relieve aortocaval compression in the initial management of the shocked woman to not exacerbate hypotension from other causes.
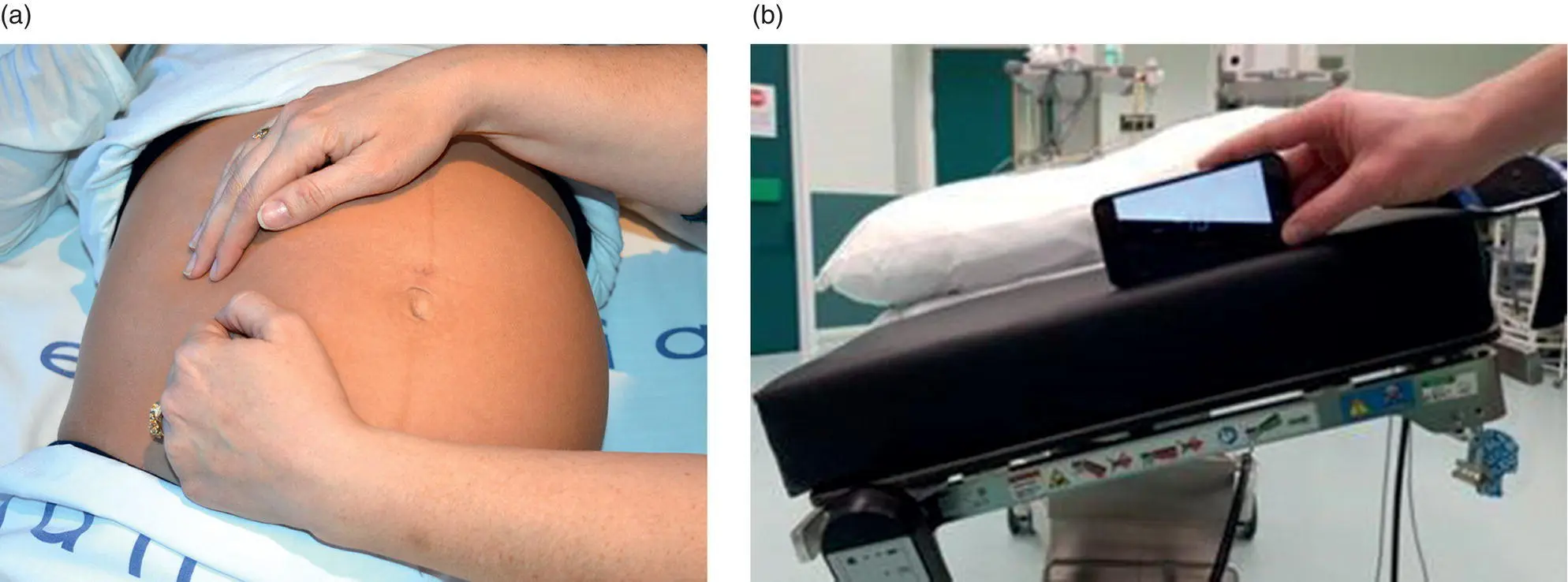
Figure 6.1 (a) Manual uterine displacement in the pregnant woman. (b) Fifteen degrees of left lateral tilt
Читать дальше