Just as there is no single location in the brain for pain, no one brain region is responsible for the itch sensation. Indeed, in a general, low-resolution sense, the brain regions activated by itch and pain are similar. Itch activates both sensory-discriminative regions, like the thalamus and the primary and secondary somatosensory cortices, and more affective-emotional-cognitive regions, like the amygdala, insula, anterior cingulate, and prefrontal cortex. (For the pain circuit, see figure 6.4.) Both pain and itch also ultimately activate regions involved in motor planning and coordination to produce and modulate withdrawal and scratching responses, respectively. 18
There are diverse forms of brain and spinal cord damage that can result in chronic itch. These include traumatic injury, certain types of stroke, brain tumors, infections, multiple sclerosis, and other autoimmune disorders. Chronic itch can also result from damage to the sensory nerves (from compression, trauma, tumors, diabetes, or infection). 19As in the case of pain, the interactions between the sensory nerves and the brain are complex, and when the sensory nerves conveying itch are damaged, aberrant itch signals are propagated to the brain. The continued bombardment of the brain by these signals (or the absence of normal itch signals) can ultimately rewire the brain’s itch circuits. People with amputated limbs, for example, can have phantom itch as well as phantom pain.
One of the most common forms of itch that results from damage to neurons follows the disease called shingles. Shingles, a common infection of sensory nerves by the herpes zoster virus, is characterized by a painful rash, most often affecting the elderly or those with compromised immune systems. Shingles destroys sensory neurons and, particularly when it occurs on the head, can ultimately result in a chronic maddening itch that cannot be effectively treated with antihistamines or steroids.
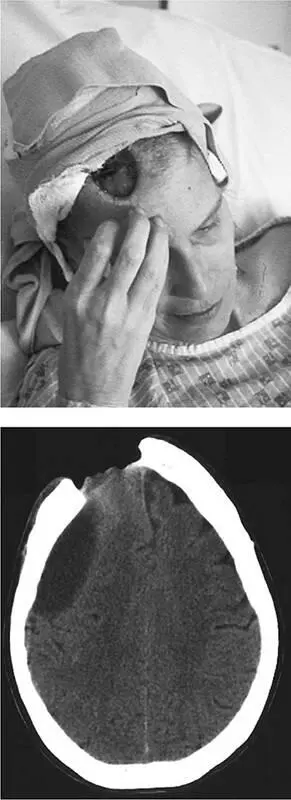
The most dramatic case of itch following shingles in the medical literature is that of M., a thirty-nine-year-old woman who developed shingles and was successfully treated with an antiviral drug. 20Shortly thereafter she felt itching and numbness on her right forehead, which she began to scratch with her fingernails. When M. sought medical attention for the problem, her internist found no infection or allergic reaction in her skin, and the itch was not relieved by anti-inflammatory creams. She was then told that her itch was psychiatric in origin—the result of depression and an obsessive-compulsive disorder. However, treatment with drugs for those conditions also failed to alleviate her itch. During the day M. could sometimes resist the urge to scratch, but at night she would scratch furiously during sleep. She tried wearing caps to bed but in the morning would always find the cap removed and blood on her pillow. With time she scratched away a patch of her hair at the itchy spot, and a scab formed. One morning ten months after her shingles had resolved, she was horrified to find a foul greenish liquid running down her face.
M. arrived at the emergency department at Massachusetts General Hospital, where it was soon determined that she had scratched through skin and skull to reach her now-exposed brain (figure 7.3); the greenish liquid was her own cerebrospinal fluid. The surgeons formed a skin graft to cover the wound, but M. soon scratched it away in her sleep. She was then outfitted with a foam helmet and mitts secured to her wrists with strong tape, to wear at bedtime. Psychiatric testing conducted at this time revealed that she did not in fact suffer from obsessive-compulsive disorder or hallucinate, yet her uncontrollable scratching made her a danger to herself. She spent two years confined to a locked medical ward, and today, years later, lives independently. She has been able to control her nocturnal scratching and has adopted coping strategies: If she must scratch, she’ll do it gently with a soft, rolled-up cloth. The brain damage from her scratching has left her partially paralyzed on the left side and has changed her personality, as often occurs with frontal-lobe damage.
The neurological origin of M.’s terrible postshingles itch is not entirely clear. Her light-touch, temperature, and pain and itch perception are normal on all parts of her skin other than the chronically itchy spot on her right forehead. That particular region has severe tactile deficits, with little perception of light touch, temperature, or pain—which explains how she could scratch through her skin without being overwhelmed by pain. A tissue biopsy revealed that about 96 percent of the sensory nerves in that patch of skin had died, yet application of an anesthetic gel that blocks neural firing was able to provide temporary relief of the itch, suggesting that the few surviving nerve fibers were sufficient to trigger the unrelenting itch sensation. (Conversely, those same nerve fibers could also convey signals in response to scratching that would relieve the itch.)
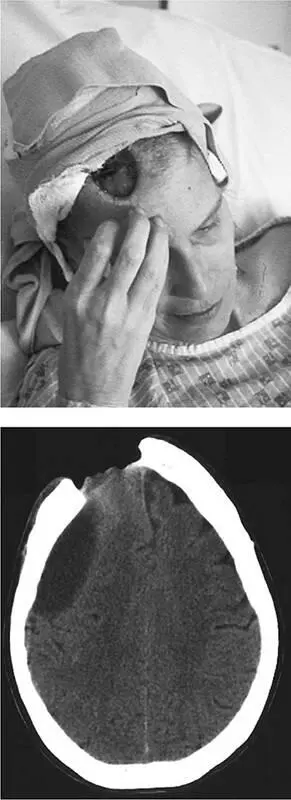
Figure 7.3Following an episode of shingles, this thirty-nine-year-old woman developed a terrible, unrelenting itch on her right forehead. The shingles had left her skin numb in that location, so she felt no pain as she scratched her way through skin and skull, ultimately contacting her brain. The bottom image shows a CT scan revealing the hole in the skull with the right frontal lobe protruding and damage to the underlying brain tissue. From A. L. Oaklander, S. P. Cohen, and S. V. Y. Raju, “Intractable postherpetic itch and cutaneous deafferentation after facial shingles,” Pain 96 (2002): 9–12, with permission of Elsevier.
In a sense, the portion of M.’s right forehead that has lost most of its nerve fibers is a lot like an amputated limb: The brain is receiving sparse and atypical information from a bodily region and is trying to interpret those signals. It’s also likely that the brain has rewired itself in response to the nerve damage and that the rewiring is involved in the chronic itch. The itch cannot result solely from activity in the itch centers of the brain, since blocking signals in the remaining forehead sensory nerves can provide temporary relief. It’s also unlikely that the brain is functioning entirely normally, and that the chronic itch is purely a result of aberrant signals in the sensory nerves. The most likely explanation is that the signals from the remaining sensory nerves trigger aberrant activity in the brain’s itch centers to create the hellish, unrelenting itch.

When people showed up for a free public lecture in the German university town of Giessen, they didn’t realize that they were to be the subjects of an unusual experiment. The title of the lecture, presented in cooperation with a public television station, was “Itching—What’s Behind It?” Video cameras in the hall were trained on the audience as well as on the speaker. The aim of the experiment was to determine if the itch sensation could be induced in the audience by showing pictures of fleas, mites, scratch marks on skin, and skin rashes. As a control, images of bathers and mothers with infants were also presented (soft, hydrated skin suggesting absence of itch). It’s not surprising that a significant increase in audience-member scratching frequency was induced by itch-related images. 21Subsequent experiments in a laboratory setting using itch-themed videos have confirmed this basic finding and have shown that the subjects need not be suffering from a preexisting skin condition in order to experience this socially contagious itch. 22One interesting proposal to explain this phenomenon was that people who were more empathetic were more likely to feel itchy themselves when they observed another person scratching. However, when personality questionnaires were given to subjects in these experiments, no correlation between empathy and social itch contagion was found. Instead, people with the greatest tendency to experience negative emotions (high neuroticism) were most likely to be subject to social itch contagion. 23
Читать дальше