A paradigm for the process by which T helper (Th) cells influence the development of different types of immunity (such as cytotoxic T cells, activated macrophages, antibodies, and the IgE response) has emerged in recent years. The simplest form of this paradigm is the Th1/Th2 cell model, in which there are two subtypes, Th1 and Th2, that control the development of acquired immunity ( Figure 4-9). Both Th1 and Th2 cells are descended from the same cell type, Th0. The decision to produce Th1 cells is triggered in part by PMN production of IL-12, which stimulates NK cells to produce IFN-γ, which in turn stimulates Th0 cells to differentiate into the Th1 form. Extracellular antigens stimulate differentiation of Th0 cells to develop into Th2 cells. IL-4 is required for Th2 differentiation and is later produced by mature Th2 cells. Cytokines produced by Th1 cells, such as IFN-γ, or by Th2 cells, such as IL-4, induce a positive feedback loop that leads to further differentiation of Th0 cells into Th1 or Th2 cells, respectively, and inhibits production of the other cell type. Later in the course of combating infection, the balance between Th1 and Th2 differentiation is eventually restored.
A third, more recently discovered pathway is the Th17 pathway ( Figure 4-9), so called because Th17 cells are CD4+ Th cells and CD8+ cytotoxic T cells that produce IL-17. The main protective role of the Th17 pathway is thought to stimulate proinflammatory reactions that lead to recruitment of PMNs and neutrophils in tissues. Th17 cells also produce other cytokines, including IL-22, which induces antimicrobial peptide production by epithelial cells that protect against extracellular bacteria and fungi.
Th2 cells activate eosinophils and stimulate B cells to produce antibodies of the IgG1 class (the most effective opsonizing antibodies) as well as antibodies of the IgE class (the class associated with the allergic or antimetazoan response). Th2 cells also produce IL-10 and IL-13, cytokines that downregulate some cells of the immune system. Thus, the Th1-type response is the most desirable type of response to viral and intracellular bacterial infections. The Th2-type response produces the more effective opsonizing antibodies, which are important for clearing extracellular bacterial pathogens. An example of the type of Th1 or Th2 response that is elicited and its importance in disease outcome is illustrated in Box 4-3.
Box 4-3.
The Th1/Th2 Response and the Outcome of Leprosy and Tuberculosis
Some people who contract tuberculosis, caused by Mycobacterium tuberculosis, or leprosy, caused by Mycobacterium leprae, develop a systemic form of the disease. In the case of tuberculosis this is called miliary tuberculosis, while in the case of leprosy this is called lepromatous leprosy. Other people develop a more localized form of the disease and, although there is damage in the area of infection, bacteria do not spread so readily to internal organs. What causes some people to develop the localized type of infection and others to develop the more dangerous systemic form of infection? What both M. tuberculosis and M. leprae have in common is that they enter and replicate in macrophages. An explanation based on the Th1/Th2 response has been proposed and seems to be supported by the evidence so far.
In people who are able to elicit a robust Th1-type immune response that leads to generation of activated macrophages, the numbers of invading bacteria are greatly reduced and the infection tends to be localized. In people who do not mount a strong Th1-type immune response, but instead mount a Th2-type response, which does not contribute to activation of macrophages but rather to production of antibodies, the bacteria reach high numbers in macrophages and subsequently disseminate throughout the body. Thus, balance between the Th1- and Th2-initiated paths of immune response to infection has critical practical implications for patients. This is one of many reasons why immunologists are trying to understand the complex interplay of cytokines that controls this crucial decision. Obviously, understanding this decision is crucial to the development of effective vaccines and therapies. Indeed, in cases for which a vaccine might not be available, development of pharmaceutical drugs capable of directing the Th1-Th2 decision branching could potentially manipulate the immune response to favor the more effective one against a particular infection. Recent evidence suggests that Treg and Th17 cells play important roles in directing the Th1-Th2 decision branching.
Source:
Modlin RL. 1994. Th1-Th2 paradigm: insights from leprosy. J Invest Dermatol 102:828–832. [PubMed] [CrossRef]
Sadhu S, Khaitan BK, Joshi B, Sengupta U, Nautiyal AK, Mitra DK. 2016. Reciprocity between regulatory T cells and Th17 cells: relevance to polarized immunity in leprosy. PLoS Negl Trop Dis 10:e0004338.
A fourth pathway that contributes to T cell regulation, the so-called Treg pathway (or Th3 pathway), has now been identified. The Treg cells produce additional regulatory compounds that control the differentiation of Th0 cells. Treg cells maintain tolerance to self-antigens and modulate autoimmune responses and serve to suppress other immune cells, particularly once invading pathogens have been cleared from the body. Cytokines produced by Treg cells can direct the outcome of an immune response, tipping the balance between one dominated by a Th1 or a Th2 pathway (as in Box 4-3).
Production of Antibodies by B Cells
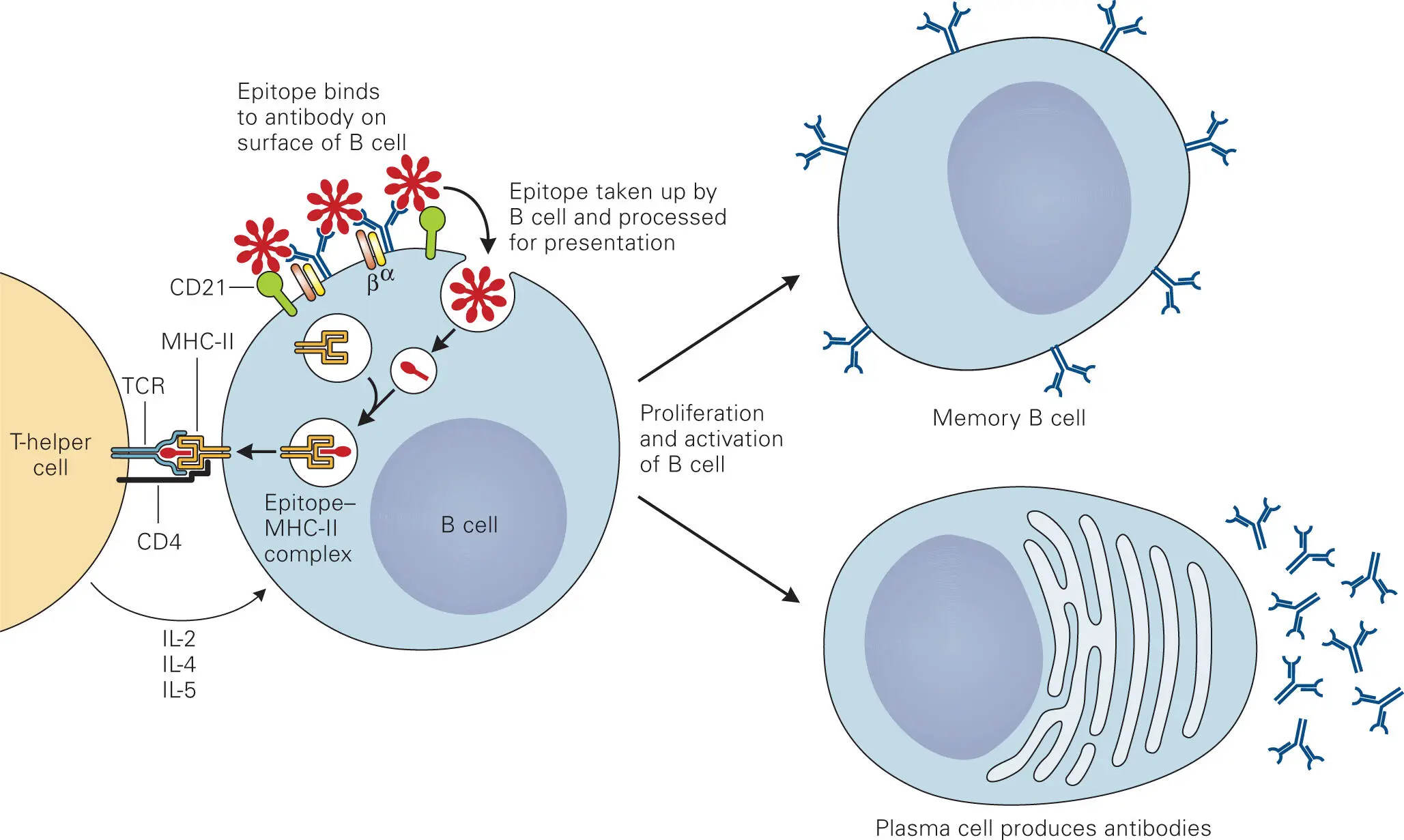
Two signals are required to activate B cells to differentiate into plasma cells and produce antibodies ( Figure 4-10). This failsafe costimulatory mechanism makes sense, considering the dire consequences of not strictly controlling antibody production. One mechanism that activates B cells is the associated Th cells that mature in the thymus gland (thymus-dependent antigens). Resting B cells are not dividing, but they do express a single type of membrane immunoglobulin (mIg) on their surfaces. There are an enormous number (>1010) of resting B cells displaying mIg molecules with different antigen specificities on their surfaces! The mIg molecules interact with a membrane-bound transducer protein to form the B cell receptor (BCR). When an antigen binds to the Fab regions of two mIg molecules, linking them together, a signal is sent to the B cell that can lead to cell proliferation, if a second signal is detected. The second signal is generated by endocytosis and presentation of the antigen on the MHC II-antigen complexes on the surface of the same B cell. The use of MHC II helps B cells find the activated Th cells that are displaying TCRs specific to the displayed antigen, which ensures specific responses to a particular antigen. Binding of a Th cell to the B cell involves a set of multiprotein contacts similar to those that occur between other APCs and T cells ( Figure 4-10). This binding causes the Th cell to produce additional surface receptors that lead to even tighter binding between the antigen-stimulated B cell and the Th cell. This tight binding stimulates the B cell to produce and display cytokine receptors and the Th cell to produce cytokines, which in turn stimulate the B cell to proliferate and differentiate into the mature form of B cells, called plasma cells, that secrete antibodies.
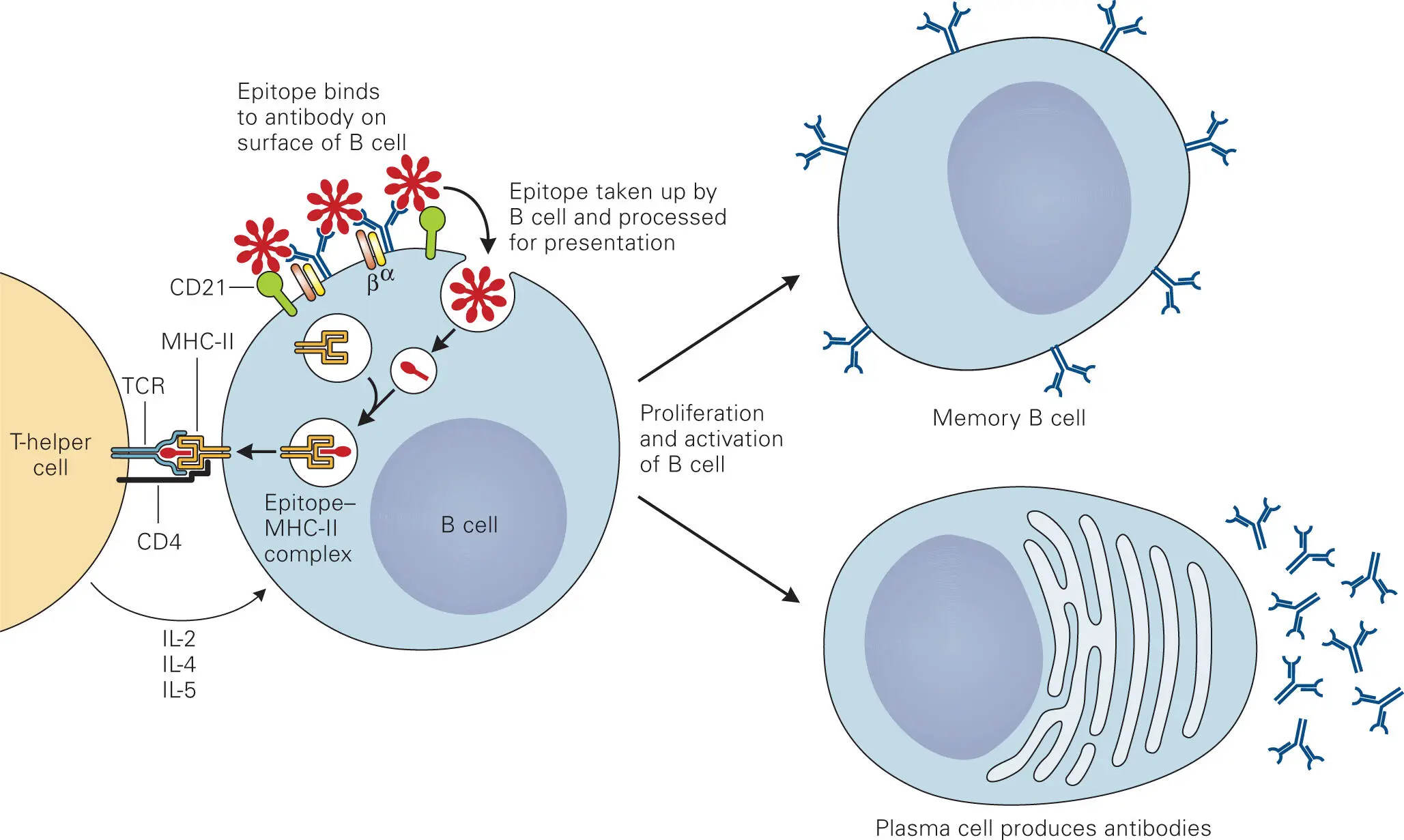
Figure 4-10. The Th2 cell binds and activates B cells presenting the same epitope on their MHC II. The B cell receptor complex is comprised of membrane-bound immunoglobulin (mIg), which can be of isotype IgM, IgD, IgA, IgG2, or IgE, the signaling mediator proteins Igα and Igβ, and the CD21 complement receptor that recognizes iC3b and promotes B cell activation. For simplicity, many of the other proteins involved in binding and activating the B cell (e.g., CD54, CD11a/CD18, CD2, CD58, CD80/70, CD28) are omitted. Stimulation of B cells through interactions of CD40 on the B cells with CD40 ligand expressed by Th cells and through cytokines produced by Th cells results in proliferation of the B cells and conversion into antibody producing cells, called plasma cells. A fraction of the activated B cells become memory B cells.
Читать дальше