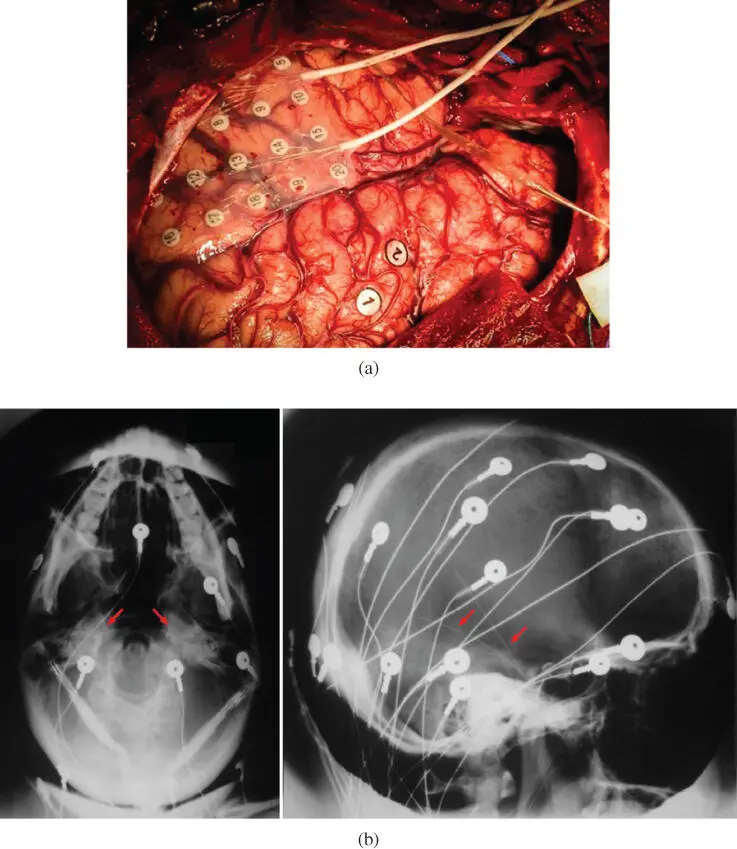
The EEG systems with their electrodes mounted over the cortex are called electrocorticography (ECoG) systems and those for measuring deep brain signals from deeper areas of the brain, are called intracranial EEG. In some applications, such as recording the neuron activities from the hippocampus, the measurement can be done by using multichannel electrodes inserted through human foramen ovale holes from both sides of the face. Figure 3.5a and bshows an ECoG and foramen ovale (FO) implant for deep brain source measurements.
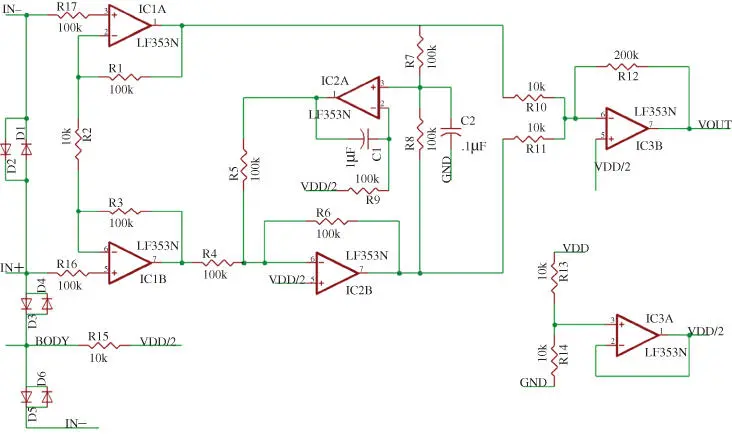
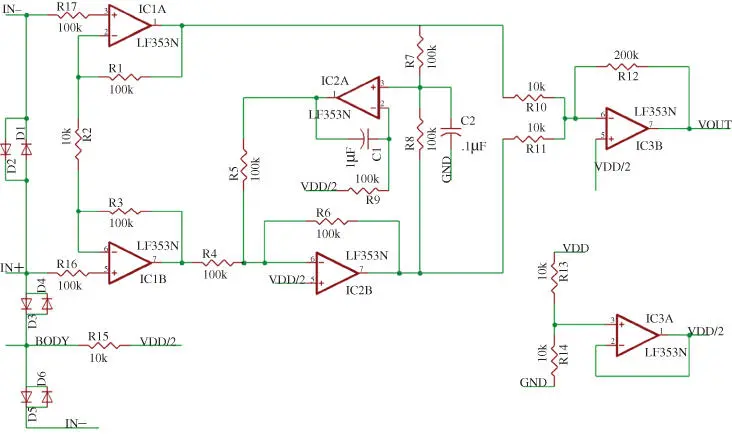
Figure 3.4 A simple EEG differential amplifier used in EEG or EMG systems.
As another brain scanning modality, magnetoencephalography (MEG) is used to measure the magnetic fields produced by the electric currents in the brain. MEG and EEG look very similar. The advantage of MEG over EEG is its insensitivity against the changes in the tissue density, so it can be effectively used for more accurate brain source localisation. However, the system is complex, bulky, expensive, and not easily available for long-term patient monitoring, and requires a high maintenance cost.
ECG (also called EKG) is used to measure the electrical activity of the heart muscle nerves. The activity stems from pumping the blood through the right supraventricular down into the right ventricle and circling upward from the left ventricle to the left supraventricular and pumping into the arteries. Often 10–14 electrodes are used with reference to the arm, wrist or foot to capture the state of different heart sections.
The systems for measuring electrical activity of the body don't involve any time delay and therefore processing of EEG, MEG, EMG, and ECG doesn't suffer any fading, clutter, or time overlapping of the signals. On the other hand, the effective frequency range falls below 500 Hz, which requires low processing power and bandwidth.
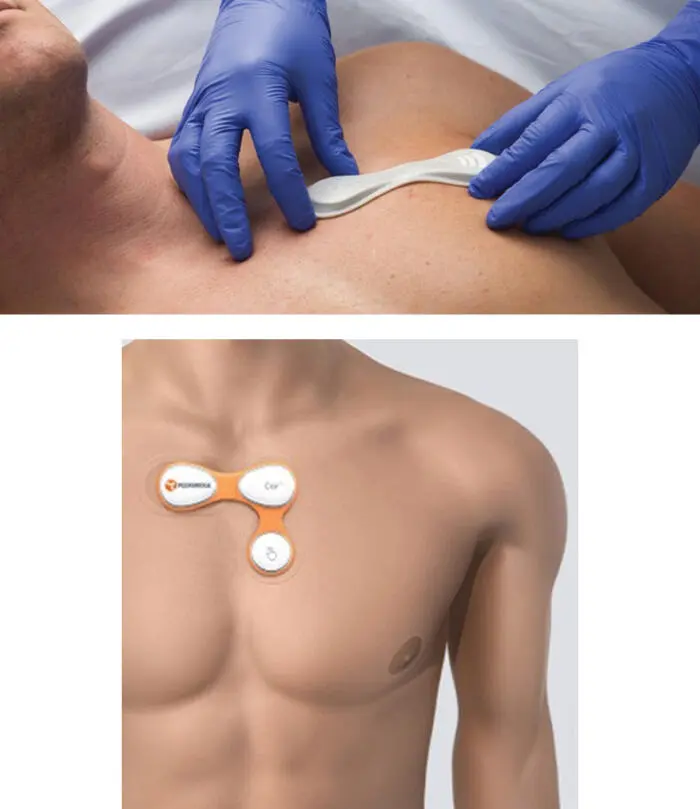
There have been efforts to miniaturise these sensors with wireless capability. As an example, Figure 3.6shows a new patch type ECG system which includes wireless connection to remote devices.
On the other hand, heart and lung sounds can be heard and recorded using electronic stethoscopes. They are sensitive microphones isolated from the surrounding environment when placed on the skin around the heart or back side of the body, so the ambient noise is greatly reduced. Most heart abnormalities as well as problems in the lung which cause wheezing or crackling can be easily heard and recorded through these systems. In some recent models, such as Modell 3200 by the Littman company ( Figure 3.7), the stethoscope can also transmit sound signals via Bluetooth to the remote device for observation, archiving, and analysis.
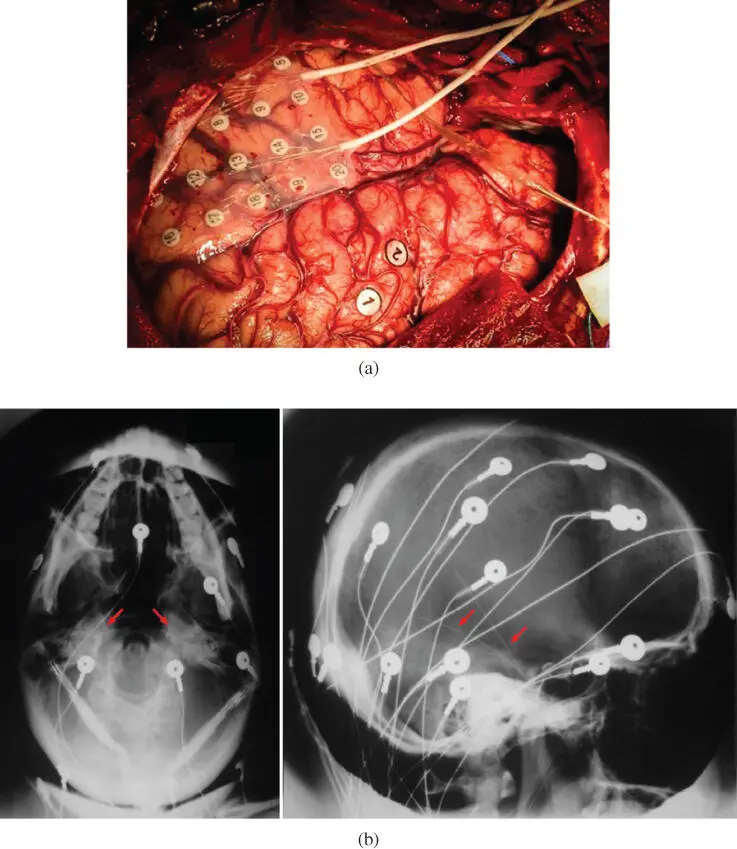
Figure 3.5 (a) ECoG and (b) foramen ovale electrodes denoted by pointers. In this setup, a scalp EEG has also been used. ( See color plate section for color representation of this figure )
One of the challenging problems in assessing the recorded stethoscope data is separation of heart and lung sounds for automatic diagnosis. The difficulty stems from the fact that sound signals are subject to delay and for their separation a robust convolutive source separation technique is required. Although many solutions have been proposed by signal processing researchers [37–40], design of a clinically usable system which can effectively separate these two sound signals is still being researched.
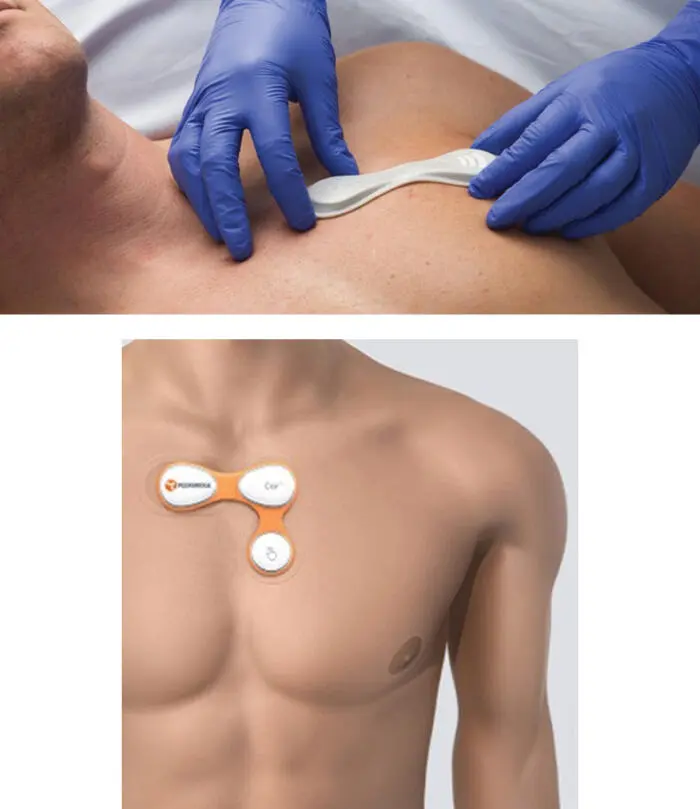
Figure 3.6 New patch type ECG systems including electrodes and wireless connection.
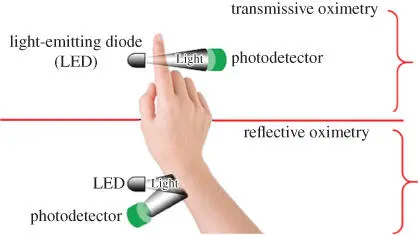
Oximeters are used to measure the blood oxygen saturation level (SpO 2). The traditional measure of SpO 2, called photoplethysmography, involves using two light beams in red and infrared wavelengths each sensitive to high and low blood oxygen levels respectively.
In principle, oximeters can operate in either transmissive or reflective mode. Those using an earlobe or finger measure the absorbed transmitted light through the tissue and others such as those used on the wrist work based on the reflective light by the tissue layers including the blood.

Figure 3.7 Electronic stethoscope; Littmann 3200 model.
In general, the SpO 2value is linearly dependent on the ratio between the transmitted infrared to red lights and decreases with this ratio. Figure 3.8shows oximeters used in different modes of oximetry.
It is logical to accept that the oximeter reading is also an indicator of heart rate as the blood oxygen changes following the heart pumping cycle. Figure 3.9shows two different oximeters with different recording modalities. The most important application of oximeters is in hospital intensive care units (ICUs) to ensure that the patient has normal breathing and heartbeat.
Amongst the other physiological measures, respiratory rate (RR) is important for the diagnosis of lung diseases and many other internal abnormalities. Therefore, it has an important role in healthcare and sport. In hospitals it is measured simply by the manual counting of breaths, conventional impedance pneumography, or an optical technique called end-tidal carbon dioxide (et-CO 2).
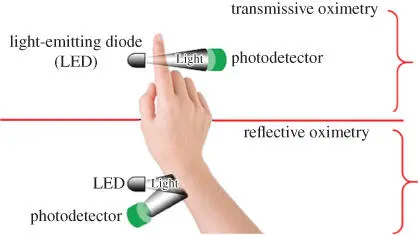
Figure 3.8 Pictorial illustration of the concepts of transmissive and reflective oximetry.

Figure 3.9 Two different models of oximeters: (a) digital pulse oximeter used on the finger and (b) wireless wrist pulse oximeter, both from Viatom.
The impedance pneumograph is a bioimpedance recorder for indirect measurement of respiration. Using superficial thoracic electrodes, the system measures respiratory volume and rate through the relationship between respiratory depth and thoracic impedance change [41].
In the et-CO 2system, a device called a capnometer uses a small plastic tube inserted in the patient's mouth. The capnometer tube accumulates the expelled CO 2in each breath. An infrared light is then emitted to the CO 2from a moving source. Following absorption of infrared radiation overtime, a variation with breathing rate will be induced. The et-CO 2-based systems are used in hospitals mainly for patients in critical conditions often within ICUs as well as ambulances for emergency checking of patient states. The capnographs, which look approximately like square waveform in normal conditions, significantly change during intubation, after cardiac arrest, ventilation problem, shock, emphysema, or leaking alveoli in pneumothorax, hypoxia due to asthma or mechanical obstruction, poor lung compliance, obese, and pregnancy [42].
Spirometry used for respiration monitoring is also one of the most common lung function tests. It measures the amount of air one can inhale and exhale. It also measures how fast the air can be emptied out of lungs. It is used to help diagnose breathing problems such as asthma and chronic obstructive pulmonary disease (COPD). During the test, the subject breathes in as much air as they can and then quickly blows as much air out as possible through a tube connected to a machine called a spirometer.
Читать дальше