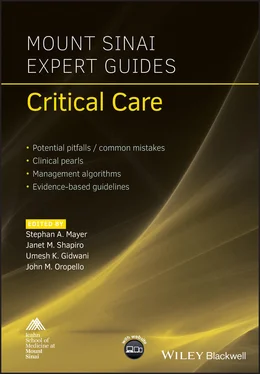
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
It is critical to understand the physiology of the shock that you are treating, and the receptor targets for each vasoactive medication, so that you can tailor therapy to the particular clinical situation.
Low preload (LVEDP)
In distributive, obstructive, or hypovolemic shock, proper fluid resuscitation is critical to improving blood pressure, cardiac output, and end‐organ perfusion. Monitoring of hemodynamic parameters and filling pressures can be helpful in this setting.
In mixed shock states, invasive hemodynamic monitoring can be useful in determining the predominant mechanism of shock and to customize therapy to the physiology of the patient.
Receptors affected by vasoactive medications
Vasoactive medications often work as agonists or antagonists of adrenergic or parasympathetic receptors. These selected receptors represent the principal targets for vasoactive therapy in the intensive care setting ( Table 12.2).
Key principles of vasoactive medication use
Diagnose and understand mechanism causing hypotension:
Physical examination, urine output, laboratory testing, imaging, and invasive hemodynamic monitoring can be important tools to differentiate the nature of the patient’s shock.
Dosage and selection of medication should be titrated to achieve a blood pressure sufficient to maintain end‐organ perfusion, as evidenced by metrics such as mentation, urine output, and blood lactate levels.
Critically ill patients also require frequent re‐evaluation for further hemodynamic insults, response to therapy, or side effects that may require changes in therapeutic strategy. Table 12.2 Action of vasoactive medications.ReceptorLocationActionα‐1 adrenergicVascular smooth muscle (peripheral, renal, coronary)Systemic vasoconstriction – increased SVRα‐2 adrenergicVascular smooth muscle and central nervous systemVasodilation – decreased SVR Sedationβ‐1 adrenergicCardiac muscleIncreased heart rate (chronotropy) and contractility (inotropy) Increased cardiac output Minimal vasoconstrictionβ‐2 adrenergicVascular smooth muscle (peripheral and renal)Vasodilation Reduced SVRDopamine (D1)Vascular smooth muscle (peripheral, renal, splanchnic, coronary, cerebral)Vasodilation in capillary bedsAcetylcholine (ACh)Parasympathetic nervous system (heart, sinoatrial and atrioventricular nodes, GI tract, eyes)Has chronotropic effects on heart Atropine is an antagonist of muscarinic ACh receptors Atropine can stimulate or accelerate AV node conductionPhosphodiesterase 3 (PDE‐3)Cardiac muscle and vascular smooth muscleIncreased contractility (inotropy) and improves diastolic relaxation (lusitropy) VasodilationVasopressin (V1, V2)Vascular smooth muscle and renal collecting ductV1 – stimulation causes vasoconstriction V2 – mediate water reabsorption in renal collecting system
Tailor vasoactive therapy to correct the specific hemodynamic derangements underlying the hypotension:This requires understanding adrenergic receptors and mechanisms of action.An example of this principle is the use of a pure alpha‐adrenergic agonist such as phenylephrine for hypotension resulting from cardiogenic shock. It might seem intuitive to use such a drug to improve hypotension from inadequately contracting the left ventricle. However, understanding the effect of such a drug on the hemodynamic equations noted above will allow you to conclude that phenylephrine use would be counterproductive. It would lead to decreased stroke volume from an increased afterload on the weakened left ventricle without the benefit of inotropic support.
Most vasoactive drugs act on multiple receptors, and many agents activate different receptors depending on the dose administered:The best example of this is dopamine, which preferentially stimulates β‐1 receptors at low doses and α receptors at higher doses.Similarly, dobutamine can increase myocardial contractility by stimulating β‐1 receptors. However, it can cause vasodilation by simultaneous activation of β‐2 receptors.The principle is to understand that vasoactive medications can have mixed hemodynamic effects, and often have different responses based on dose.
A given vasoactive agent can have both direct actions and reflex actions:The vascular system is closely regulated by multiple physiologic mechanisms including the autonomic nervous system that seeks to ensure cardiovascular stability.For example, phenylephrine‐induced vasoconstriction can lead to increased mean arterial pressure, which may lead to baroreceptor activation and a compensatory reflex bradycardia.
Responsiveness to the vasoactive medications can decrease over time due to a phenomenon known as tachyphylaxis:Up‐titration of doses or initiation of new agents with different receptor targets must be done regularly.
Central line access and arterial line monitoring are a must:Catecholamines and vasopressor agents are given as continuous infusions due to their short half‐lives. They carry significant risks of peripheral extremity ischemia due to potent vasoconstriction as well as skin necrosis if they extravasate. Central venous access is usually necessary.With all intravenous vasoactive infusions, invasive hemodynamic monitoring with an arterial line is needed because of rapid hemodynamic changes and side effects such as arrhythmias
Vasoactive medications in focus
| Epinephrine | |
| Receptor binding | α‐1, β‐1, β‐2 |
| Pharmacology | β receptor predominant at lower doses, α receptor predominant at higher doses |
| Dosing range | 0.01–0.10 μg/kg/min (for 70 kg adult, that is 0.7–7 μg/min) |
| Clinical scenarios to consider use | Cardiac arrest Extreme hemodynamic collapse Additional agent when already on several vasopressors Shock after cardiac surgery Right ventricular failure Anaphylaxis |
| Clinical pearls | Reserved for refractory or severe shock despite multiple vasopressors or extreme hemodynamic compromise Associated with decreased mesenteric, coronary, and renal blood flow and regional ischemia resulting in a lactic acidosis |
| Norepinephrine | |
| Receptor binding | α‐1, β‐1, β‐2 |
| Pharmacology | Less β receptor activity than epinephrine α receptor predominant at higher doses |
| Dosing range | 0.01–3 μg/kg/min (for 70 kg adult, that is 0.7–210 μg/min) |
| Clinical scenarios to consider use | Septic shock (first line) Cardiogenic shock (first line) Vasoplegia after cardiac surgery |
| Clinical pearls | If norepinephrine requirements are increasing, evaluate volume status and pH Norepinephrine has been demonstrated to be equivalent to other vasopressor agents, including dopamine, with less adverse events, including tachyarrhythmias In cardiogenic shock, mortality was lower with norepinephrine than with dopamine. This has led to use of norepinephrine as first line agent for cardiogenic shock, including shock from an acute myocardial infarction The Surviving Sepsis Campaign guidelines recommend norepinephrine as the first line agent for septic shock |
| Dopamine | |
| Receptor binding | α‐1, β‐1, β‐2, D1 |
| Pharmacology | Binds DA receptors at low doses, promoting vasodilation particularly in the splanchnic circulation Binds adrenergic receptors at higher doses, leading to vasoconstriction |
| Dosing range | 0.5–3 μg/kg/min, predominantly D 1agonism 3–10 μg/kg/min, weak β‐1 agonism; promotes norepinephrine release >10 μg/kg/min, increasing α‐1 receptor agonism: Vasodilation of capillary beds (low dose)Increased contractility and chronotropy (medium dose)Vasoconstriction (high dose) |
| Clinical scenarios to consider use | Cardiogenic shock complicating acute myocardial infarction with moderate hypotension(SBP 70–100 mmHg); however, this has largely been replaced by norepinephrine Symptomatic bradycardia (temporizing measure) |
| Clinical pearls | While often used as a vasopressor agent that can be used peripherally while central access is being set up, extravasation of dopamine is not benign Renal dosing of dopamine for acute kidney injury was hypothesized to be of use due to vasodilation and improved blood flow to the splanchnic circulation at lower doses (1–3 μg/kg). However, clinical trials have not shown a benefit and it is currently not recommended for this use |
| Dobutamine | |
| Receptor binding | β‐1, β‐2, minor α‐1 |
| Pharmacology | Synthetic catecholamine with preferential β‐1 agonism (3:1 ratio of β‐1 to β‐2), inotropic effect β‐2 activity causes vasodilation, which makes dobutamine an inodilator Progressive α‐1 agonism at high doses causes vasoconstriction |
| Dosing range | 2–40 μg/kg/min Dose in ICU for cardiogenic shock rarely exceeds 10 μg/kg/min |
| Clinical scenarios to consider use | Acute decompensated systolic heart failure Refractory septic shock associated with low cardiac output (also known as ‘hypodynamic’ or ‘cold’ sepsis, a relatively small subset of patients) Pharmacologic stress testing (e.g. for ischemia, viability, aortic stenosis severity) |
| Clinical pearls | Tolerance develops after a few days of therapy Ventricular arrhythmias can occur at any dose Dobutamine significantly increases myocardial oxygen demand so do not use in patients with acute coronary syndromes, severe and unstable coronary disease, or ongoing ischemia Dobutamine has inotropic properties that increase myocardial contractility and cardiac output, while the vasodilatory effects further improve cardiac output by reducing afterload. This makes dobutamine an ideal agent in decompensated heart failure. Remember to use an agent such as norepinephrine as the initial agent if shock and hypotension are present |
| Milrinone | |
| Receptor binding | PDE‐3 |
| Pharmacology | PDE‐3 inhibitor PDE‐3 inhibition increases intracellular cAMP concentrations, enhancing contractility and promoting vascular smooth muscle relaxation Relatively long half‐life (2–4 hours) Renal elimination |
| Dosing range | 0.125–0.75 μg/kg/min (renal adjust) |
| Clinical scenarios to consider use | Acute decompensated systolic heart failure Right ventricular failure |
| Clinical pearls | Fewer arrhythmogenic and chronotropic side effects compared with catecholamines, but vasodilatory effects can worsen hypotension that limits the use of milrinone in patients with shock Can be useful if adrenergic receptors are downregulated or desensitized in setting of chronic heart failure, or after chronic β‐agonist administration Potent pulmonary vasodilator so can be useful in right ventricular (RV) failure by lowering pulmonary vascular resistance (RV afterload) Long half‐life (2–4 hours); hypotension can persist for longer so short‐term infusions may be more beneficial than continuous infusions |
| Phenylephrine | |
| Receptor binding | α‐1 |
| Pharmacology | Pure α‐1 agonism Minimal inotropic and chronotropic effect Rapid onset, short half‐life |
| Dosing range | 0.4–9.1 μg/kg/min (for 70 kg adult, that is 28–637 μg/min) Bolus administration possible, usually 0.1–0.5 mg every 5–15 minutes |
| Clinical scenarios to consider it | Dynamic intracavitary gradient: ‘suicide ventricle’ after transcatheter aortic valve replacement (TAVR), anteroapical STEMI, hypertrophic cardiomyopathy with systolic anterior motion of the mitral valve and LV outflow obstruction, and Takotsubo cardiomyopathy Inadvertent combination of sildenafil and nitrates Hypotension during PCI or anesthesia‐related hypotension Hypotension in the setting of atrial fibrillation with rapid ventricular rate Aortic stenosis with hypotension Vagally mediated hypotension during percutaneous diagnostic or therapeutic procedures |
| Clincial pearls | Phenylephrine increases MAP by raising SVR (afterload), and therefore is particularly useful when SVR <700 dyn·s/cm 5Increased afterload can result in decreased stroke volume and cardiac output in patients with pre‐existing cardiac dysfunction |
| Contraindicated in patients with SVR >1200 dyn·s/cm 5, which is most patients with cardiogenic shock Lower concentration (20 μg/mL) available which can be infused peripherally while awaiting central line placement Generally not recommended for septic shock unless serious arrhythmias happen with norepinephrine Can cause reflex bradycardia |
| Vasopressin | |
| Receptor binding | V1, V2 |
| Pharmacology | Agonism of V1 receptors on smooth muscle causes vasoconstriction Agonism of V2 receptors in nephron induces translocation of aquaporin water channels to plasma membrane of collecting duct cells |
| Dosing range | Fixed dose: 0.04 units/min |
| Clinical scenarios to consider it | When avoiding β agonism is desired (e.g. left ventricular outflow obstruction, tachyarrhythmia) or when trying to reduce dose of first line agent Hypotension accompanied by severe acidosis Second line agent in refractory vasodilatory/septic shock |
| Clinical pearls | Vasoconstrictive effect is relatively preserved despite conditions of hypoxia and acidosis (which can attenuate effects of catecholamines) Doses above 0.04 units/min have been associated with coronary and mesenteric ischemia and skin necrosis Rebound hypotension often occurs after withdrawal of vasopressin. To avoid this, the dose is slowly tapered by 0.01 units/min every 30 minutes |
Reading list
Интервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.