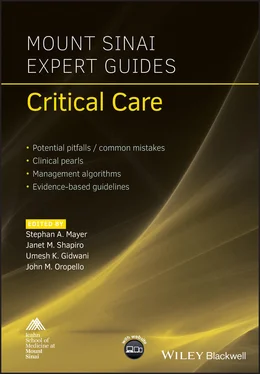
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Other mechanical life‐sustaining devices should also be considered when discussing withdrawal of care. Mechanical circulatory support devices, pacemakers, and defibrillators fall under this category and should be deactivated if a decision is made to withdraw care. Similar to symptom control after ventilator withdrawal, opioids, anxiolytics, and anticholinergic agents should be provided for patient comfort.
Reading list
1 Angus DC, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med 2004; 32(3):638–43.
2 Azoulay E, et al. Risk of post‐traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005; 171(9):987–94.
3 Cook D, Rocker G. Dying with dignity in the intensive care unit. N Engl J Med 2014; 370(26):2506–14.
4 Nelson JE, et al. for the Improving Palliative Care in the Intensive Care Unit Project. Models for structuring a clinical initiative to enhance palliative care in the intensive care unit: a report from the IPAL‐ICU Project (Improving Palliative Care in the ICU). Crit Care Med 2010; 38(9):1765–72.
5 O'Mahony S, et al. Preliminary report of the integration of a palliative care team into an intensive care unit. Palliat Med 2010; 24(2):154–65.
6 Swetz KM, Mansel JK. Ethical issues and palliative care in the cardiovascular intensive care unit. Cardiol Clin 2013; 31:657–68.
7 Temel JS, et al. Early palliative care for patients with metastatic non‐small‐cell lung cancer. N Engl J Med 2010; 363:733–42.
Additional material for this chapter can be found online at:
www.wiley.com/go/mayer/mountsinai/criticalcare
This includes multiple choice questions.
PART 2 Cardiovascular Critical Care
Section Editor: Umesh K. Gidwani
CHAPTER 11 Hemodynamic Monitoring
Josue Rivera1 and Leila Hosseinian2
1North Shore University Hospital, Manhassett, NY, USA
2Icahn School of Medicine at Mount Sinai, New York, NY, USA
OVERALL BOTTOM LINE
Patients requiring ICU care often require multiple forms of hemodynamic monitoring.
There has been a tremendous increase in usage of invasive hemodynamic monitoring in order to enhance our understanding of patients’ hemodynamics and helping to guide appropriate therapeutic interventions.
Although there is a paucity of evidence to support the use of many of these invasive monitors, they are very commonly used in the ICU.
Arterial lines
Indications
Direct arterial pressure monitoring is recommended for all ICU patients with hemodynamic instability who require inotropic or vasopressor medications as well as significant ventilatory deficits. This allows for continuous monitoring of blood pressure as well as access to the arterial circulation for the measurement of arterial oxygenation and frequent blood sampling.
As the pulse moves peripherally, the pressure waveform is distorted with higher systolic pressure and pulse pressure ( Figure 11.1).
Locations for placement
Radial artery: common site of cannulation. Check collateral flow of ulnar artery with the Allen’s test, which has low reliability.
Brachial artery: located in antecubital fossa, lack of collateral circulation, median nerve injury possible.
Axillary artery: can cause axillary nerve damage from hematoma or traumatic cannulation.
Femoral artery: prone to pseudoaneuryms and atheroma formation.
Dorsalis pedis and posterior tibial arteries: most distorted waveforms.
Contraindications
Deficiencies of collateral circulation (e.g. Raynaud’s phenomenon).
Complications
Rates of up to 10%.
Hematoma, bleeding, vasospasm, arterial thrombus, aneurysm, dissection, pseudoaneurysm, infection.
Advanced arterial hemodynamic monitoring
Multiple proprietary systems have developed algorithms for estimating cardiac output from the arterial waveform. Arterial pulse contour analysis can evaluate stroke volume to calculate cardiac output and examine stroke volume variation to assess fluid responsiveness.
Characteristics of the arterial pressure waveform are affected by changes in vascular compliance, aortic impedance, and peripheral arterial resistance, limiting the accuracy and utility of this class of monitors.
Pulse contour analysis
The principle is based on the hypothesis that stroke volume is proportional to the area under the curve of the systolic segment of an arterial waveform.
PiCCO system (Pulsion Medical Systems)
Pulse contour cardiac output (PiCCO) requires the insertion of a central venous catheter and a thermodilution arterial line.
It provides hemodynamic monitoring by combining pulse contour analysis and a transpulmonary thermodilution technique to provide a continuous display of PiCCO cardiac index (L/min/m2) and stroke volume (mL/kg).
Calibration of the PiCCO to more accurate transpulmonary thermodilution cardiac output measurements needs to be repeated every 8 hours, or more frequently if the patient is hemodynamically unstable.
Additional data derived from the PiCCO system include:Extravascular lung water index (mL/kg).Global end‐diastolic volume (measure of cardiac preload in mL/m2).Systemic vascular resistance index (dyn·s/cm5/m2).Stroke volume variation (%).
FloTrac™ system (Edwards Lifesciences)
Requires an arterial line.
Uses pulse contour analysis based on an algorithm to provide continuous cardiac output, stroke volume, and stroke volume variation in real time.
Provides an estimate of cardiac output using the standard deviation of the arterial pulse pressure around the mean arterial pressure and a conversion factor.
Calibration is not required.
Pulse power analysis
LiDCO system
Lithium dilution cardiac output (LiDCO) requires a peripheral or central arterial line.
Uses pulse power analysis rather than pulse contour analysis. The algorithm is based on the assumption that the net power change in the system in a heartbeat is the difference between the amount of blood entering the system, the stroke volume, and the amount of blood flowing out peripherally.
Requires calibration using transpulmonary lithium indicator dilution technique via a peripheral venous line. It is not as accurate when the patient is receiving lithium or certain neuromuscular‐blocking agents.
Central lines
CVP is measured via a central line at the level of the right atrium or vena cava. It is equal to the right ventricular end‐diastolic pressure.
CVP can be used to determine preload, the filling pressure of the heart. It has been used to estimate whether a patient is adequately resuscitated as well as helping to assess right ventricular function. Table 11.1 Waveform components.Waveform/descentPhase of cardiac cycleECGMechanical eventA waveEnd diastoleFollows P wavePressure increase due to atrial contractionC waveEarly systoleFollows R wavePressure increase due to tricuspid bulging into the right atriumV waveLate systoleEnd of T wavePressure increase due to systolic filling of the atriumX descentMid systoleDrop in atrial pressure due to atrial relaxationY descentEarly diastoleDrop in atrial pressure due to early ventricular filling
A central line allows for infusion of hypertonic solutions and medications that can damage peripheral veins. It also allows for serial venous blood analysis and venous blood gas (VBG).
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.