Of particular importance, lactate and central venous saturation measurements from VBGs have been used to direct resuscitation efforts.
Normal CVP is 2–8 mmHg.
Internal jugular, subclavian vein, femoral vein.
Rates of up to 15%.
Inadvertent arterial puncture and/or cannulation, pneumothorax, hemothorax, cardiac arrhythmias, venous air embolism, infections.
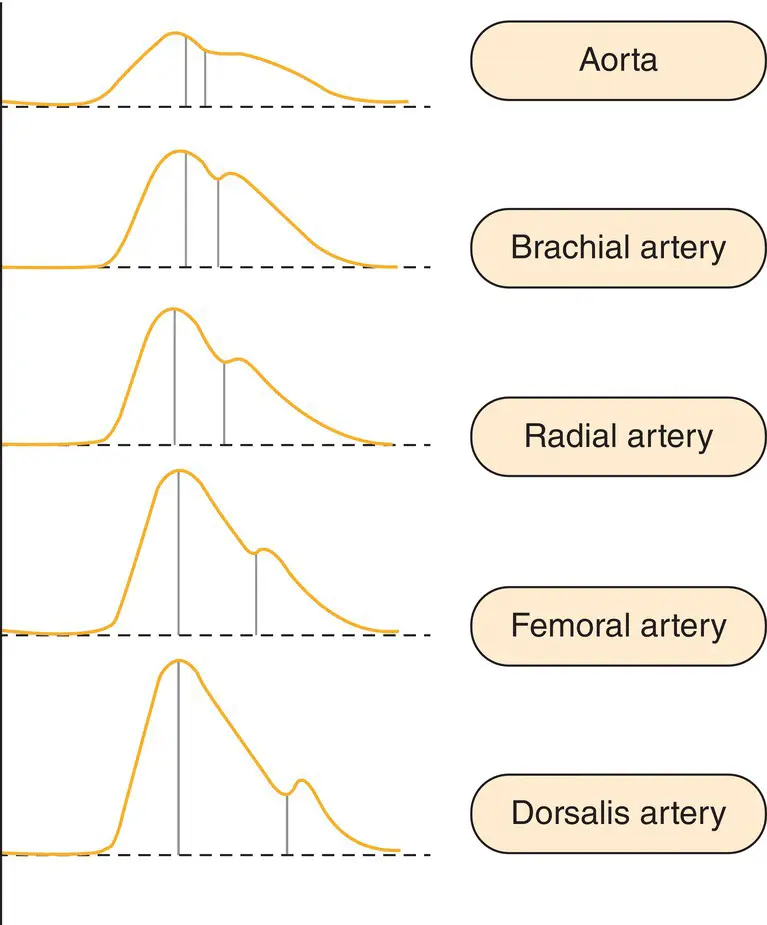
As the heart beats, a CVP waveform is produced. There are three waves and two descents ( Table 11.1and Figure 11.2).
Controversy regarding the utility of CVP monitoring
Use of CVP to guide fluid management has been heavily debated. CVP is not useful as a static measurement. Trending the CVP can be useful to determine a patient’s response to a fluid challenge.
Useful measurements depend on proper calibration, normal pulmonary resistance, and right heart function.
Pulmonary artery catheter monitoring
Background
Swan and Ganz first described the pulmonary artery catheter (PAC) in 1970 and it was widely used in the 1980s. However, as more trials were published in the 1990s and 2000s, its popularity declined.
Connors et al. published a prospective randomized trial in 1996 finding an increased cost, length of stay, and mortality in critically ill patients with a PAC.
The Fluid and Catheter Treatment Trial compared mortality, ventilator‐free days, and ICU length of stay among patients with acute lung injury and found no significant benefit to PAC in PAC‐directed resuscitation. The use of PAC resulted in no difference in LOS in the ICU or mortality.
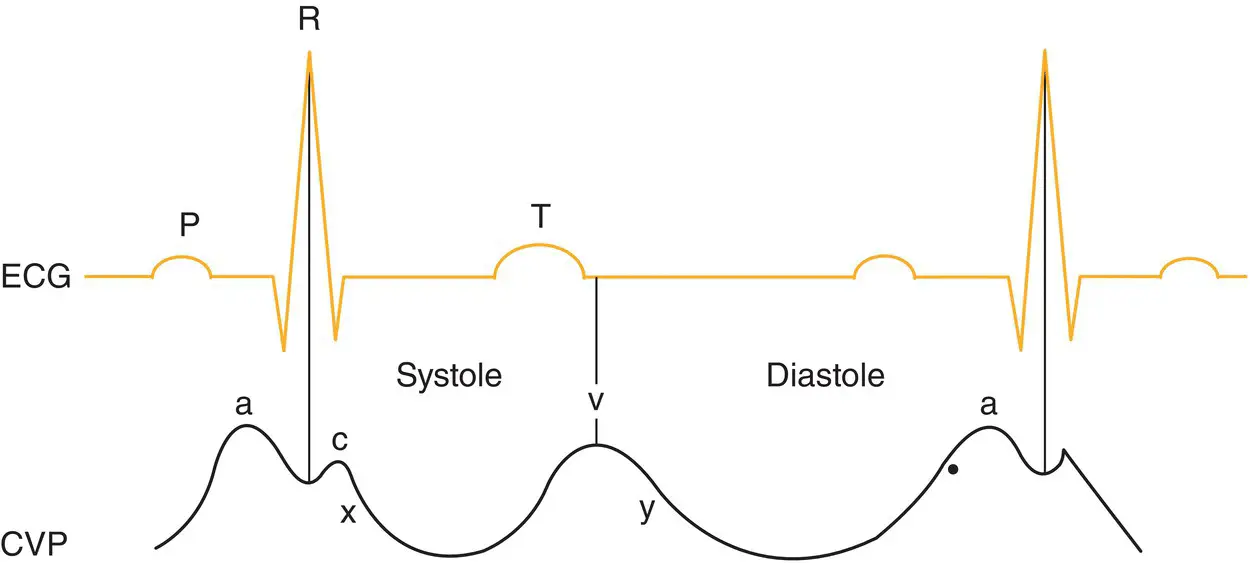
The PAC requires placement of a balloon‐tipped catheter into the right atrium, across the tricuspid valve, into the right ventricle, and across the pulmonary valve, until it is ‘wedged’ into a pulmonary artery. At each anatomic location different pressure waveform profiles will be seen ( Figure 11.3).
Acute MI with progressive hypotension or suspected mechanical complications.
Acute right ventricular failure.
Intraoperative/perioperative care:Vascular surgery.Cardiac surgery.Moderate/high risk patients receiving goal‐directed resuscitation.
Undifferentiated shock.
Right atrial pressure (0–8 mmHg).
Right ventricular pressure (systolic 20–30, diastolic 0–5 mmHg).
Pulmonary artery pressure (systolic 20–30, diastolic 8–12 mmHg).
Pulmonary artery wedge pressure (PAWP): surrogate for left ventricular preload (4–12 mmHg).
Cardiac output (CO)/cardiac index: measured using the thermodilution technique (reliability of measurement is affected by tricuspid or pulmonary regurgitation or intracardiac shunts):Normal CO: 4–8 L/min.Normal CI: 2.5–4 L/min/m2.
Stroke volume (SV) = CO/HR:Normal: 60–120 mL/beat.
Systemic vascular resistance (SVR) = 80 × [(MAP – RAP)/CO]:Normal: 1600–3000 dyn·s/cm5.
Pulmonary vascular resistance (PVR) = 80 × [(mean PAP – mean PAWP)/CO]:Normal: 37–250 dyn·s/cm5.
Rates of 5–10%.
Bleeding, hematoma, arterial puncture/cannulation, pneumothorax, hemothorax, tachyarrhythmias, right bundle branch block, complete heart block, pulmonary artery rupture, myocardial perforation, infection.
Ultrasound echocardiography is an operator‐dependent hemodynamic assessment, which is a quick and non‐invasive measurement tool. Its effectiveness has not yet been proven in randomized clinical trials.
Cardiac function and anatomy can be assessed using five standard views ( Table 11.2).
Stroke volume can be estimated with echocardiography:SV = π × R2 × velocity time interval (VTI) of the left ventricular outflow tract (LVOT) (R= radius of LVOT in cm).Parasternal long axis view is used to measure diameter of the LVOT.Apical five chamber view is used to measure the VTI with pulsed Doppler.
Routine measurements of the size of the IVC and collapsibility with respiration can be used to estimate right atrial pressure (RAP) and fluid responsiveness in patients via the subcostal view on echocardiography.
Size ≤2.1 cm, collapses >50% during inspiration = RAP 0–5 mmHg.
Size >2.1 cm, collapses >50% during inspiration = RAP 5–10 mmHg.
Size >2.1 cm, collapses <50% during inspiration = RAP 10–20 mmHg.
Table 11.2 Echocardiography views.
| View |
Findings |
| Parasternal long axis |
Pericardial effusion, LV/RV size and function, septal kinetics |
| Parasternal short axis |
Pericardial effusion, LV/RV size and function, septal kinetics |
| Apical four chamber |
Pericardial effusion, LV/RV size and function |
| Subcostal four chamber |
LV/RV size and function, preferred view in cardiac arrest |
| Inferior vena cava longitudinal view |
Determine preload sensitivity |
1 Bolt, J. Clinical review: hemodynamic monitoring in the intensive care unit. Crit Care 2002; 6:52–9.
2 Conners AF, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA 1996; 276:889–97.
3 Greenstein YY, Mayo PH. Critical care echocardiography. In: Oropello JM, Kvetan V, Pastores SM (eds) Critical Care. New York: McGraw‐Hill, 2017, pp. 1141–50.
4 Leatherman JW, Marini JJ. Clinical use of the pulmonary artery catheter. In: Hall JB, Schmidt GA, Wood LDH (eds) Principles of Critical Care, 2nd edition. New York: McGraw‐Hill, 1998, pp. 155–76.
5 Mark JB. Central venous pressure monitoring: clinical insights beyond the numbers. J Cardiothorac Vasc Anesth 1991; 5:163–73.
6 Monnet X, Teboul JL. Minimally invasive monitoring. Crit Care Clin 2015; 31:25–42.
7 Porter TR, et al. Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults: a report from the American Society of Echocardiography. J Am Soc Echocardiogr 2015; 28:40–56.
8 Weiner R, Ryan E, Yohannes‐Tomicich J. Arterial line monitoring and placement. In: Oropello JM, Kvetan V, Pastores SM (eds) Critical Care. New York: McGraw‐Hill, 2017, pp. 1085–92.
9 Yunen RA, Oropello JM. Pulmonary artery catheterization. In: Oropello JM, Kvetan V, Pastores SM (eds) Critical Care. New York: McGraw‐Hill, 2017, pp. 1245–61.
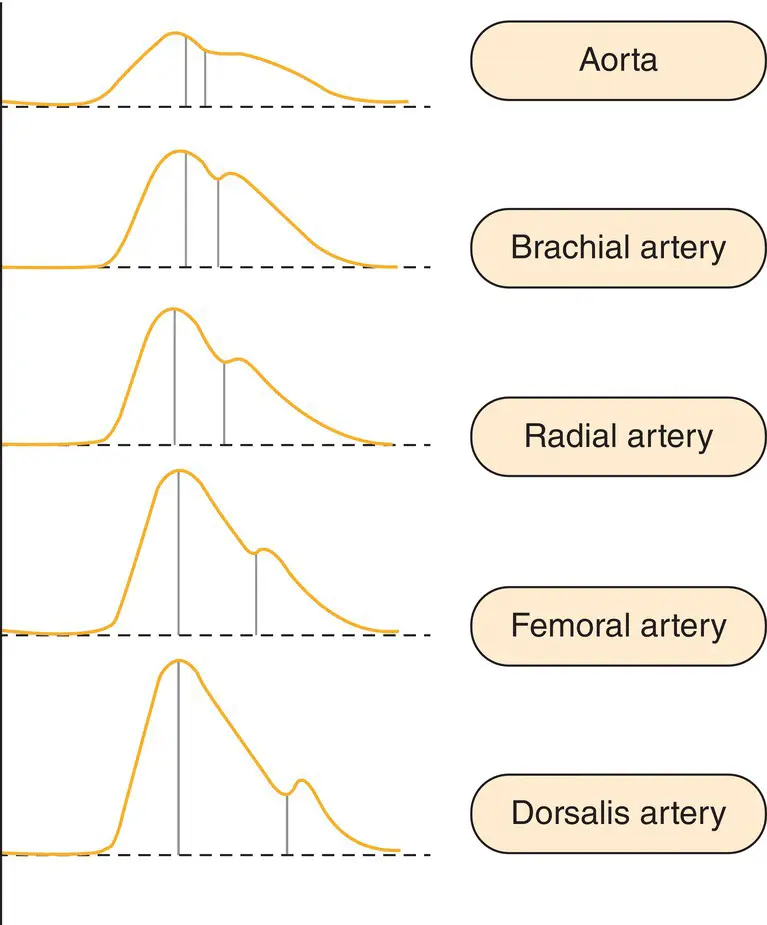
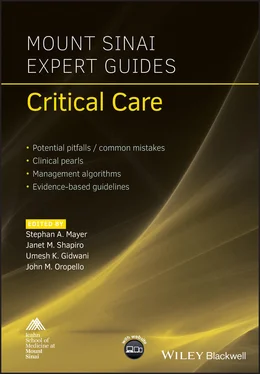
Figure 11.1 Arterial pressure waveforms at different locations in the vascular tree.
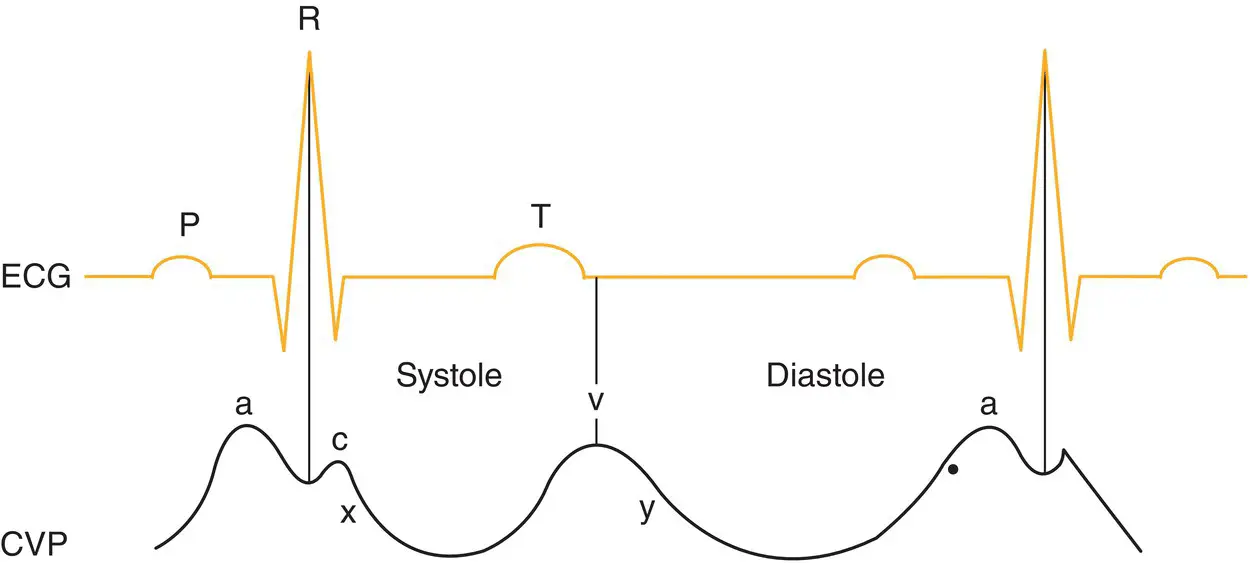
Figure 11.2 Components of the CVP waveform throughout the cardiac cycle.
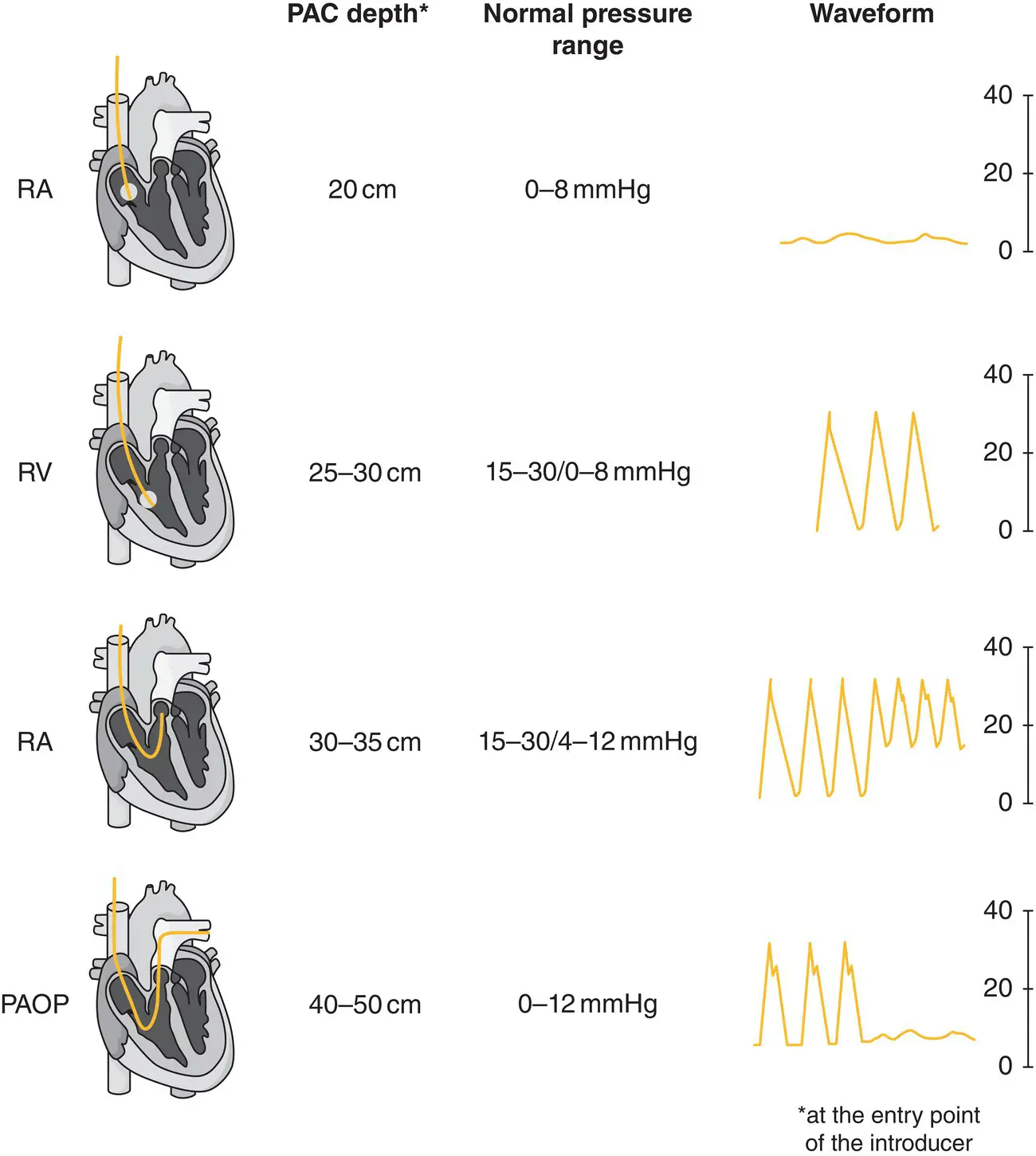
Figure 11.3 Placement of a pulmonary artery catheter. At different depths of catheter placement different waveform profiles will be identified.
Additional material for this chapter can be found online at:
Читать дальше