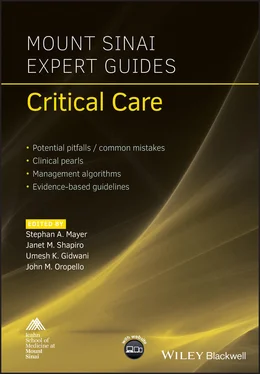
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Examination of the neck should note any masses or goiters as well as tracheal deviation from the midline. One should note neck circumference, the ability to flex and extend the neck, as well as thyromental distance.
Table 1.1 Predictors of difficulties with mask ventilation and/or intubation.
| Predictors of difficult mask ventilation | Predictors of difficult laryngoscopy |
|---|---|
| Edentulous | Overbite |
| Age 55 years or older | Small mouth opening <3 cm |
| Male patient | Mallampati class III or IV |
| Presence of facial hair | Thyromental distance <3 fingerbreadths |
| Obesity | Neck circumference >43 cm (17 inches) |
| Obstructive sleep apnea | Limited cervical mobility |
Equipment
Proper preparation is essential for all airway management situations.
Essential equipment includes oxygen source (wall or tank), suction, bag‐mask ventilation circuit, direct and/or video laryngoscopes, endotracheal tubes of several sizes, supraglottic airway device, blood pressure/ECG/pulse oximetry, and CO2 detection device.
Supraglottic airway devices include the laryngeal mask airway (LMA) which is inserted into the patient’s mouth and sits above the glottis. As these devices do not protect against aspiration of gastric contents, in the ICU they are generally limited to rescue devices in situations where mask ventilation and endotracheal intubation are difficult.
While numerous types of direct laryngoscopes are available, the two most common are the Macintosh blade (MAC) and the Miller blade. Both come in multiple sizes, but typically a MAC 3 or Miller 2 are suitable for a standard‐sized adult.
In recent years, video laryngoscopes, a form of indirect laryngoscopy, have become readily available in most institutions. Video laryngoscopes differ from one another in the shape of the blade, proper position when inserted into the mouth, location of the video source, and reusable/disposable parts. Glidescope® has its own (non‐disposable) stylet which accompanies the unique shape of its blade. One potential problem with video laryngoscopy is that, while it may provide a clear view of the glottic opening, one still may have difficulty maneuvering an endotracheal tube into proper position.
Endotracheal tubes (ETTs) are also available in various materials and sizes. Most commonly used in the ICU are ETTs made from polyvinyl chloride with a beveled tip to allow better visualization of insertion, a side hole (Murphy’s eye) to prevent total occlusion in the event of a mucous plug, and an inflatable cuff. ETTs are sized according to internal diameter in millimeters and the appropriate size for adults is typically 7.0–8.0 mm. Bear in mind that if bronchoscopy is needed, ETTs smaller than 7.5 mm may be too narrow to accommodate an adult bronchoscope.
Positioning
Proper patient positioning is of utmost importance and should be achieved prior to any airway intervention, particularly if direct laryngoscopy is to be attempted. Proper positioning can be the difference between a successful and unsuccessful laryngoscopy attempt.
With the provider standing at the head of the bed, the patient’s head should be as far towards the head of the bed as possible. The height of the bed should be to the provider’s preference.
Proper positioning creates a direct line of sight from the patient’s mouth to the larynx. This is accomplished using approximately 30° of cervical flexion using pillows/blankets along with extension of the atlanto‐occipital joint, the classic ‘sniffing position.’
Positioning obese patients may be particularly challenging. This can be accomplished by forming a ramp, elevating the upper back and shoulders in order to accommodate adequate cervical flexion. Confirming horizontal alignment of the external auditory meatus with the sternal notch can be a useful guide.
Preoxygenation
Adequate preoxygenation should be provided in all but the most emergent situations.
The aim is to replace nitrogen in the lungs with oxygen. This increases the length of time before desaturation when the patient is apneic (‘apnea time’), providing a margin of safety in case ventilation and intubation become difficult.
Preoxygenation can be performed using a facemask, continuous or bilevel positive airway pressure, or a high flow nasal cannula (HFNC) providing 100% oxygen at flows of at least 10 L/min. It typically requires approximately 3 minutes of normal tidal volume breathing to achieve an end‐tidal oxygen concentration of approximately 90%.
Given normal functional residual capacity (FRC) of about 2 L, and an oxygen consumption rate of about 200–250 mL/min, a properly preoxygenated adult should have an apnea time of about 5–8 minutes before significant desaturation. Reductions in apnea time should be expected in conditions in which FRC is decreased (i.e. obesity, pregnancy, tense ascites) or conditions of increased oxygen consumption (i.e. sepsis, pregnancy, hyperthyroidism).
Bag and mask ventilation
The ability to ventilate a patient using a bag and mask is by far the most important skill for any airway provider to master. The inability to intubate the trachea is not fatal if mask ventilation is possible, making it a vital component of the ASA difficult airway algorithm.
Relative contraindications to mask ventilation are full stomach/regurgitation risk, severe facial trauma, and unstable cervical spine fractures.
Mask ventilation is performed with the provider holding the mask in his or her left hand with the mask over the patient’s nose and mouth with the third, fourth, and fifth digits holding the mandible and lifting the face into the mask while the thumb and index finger form a ‘C’ shape around the collar aspect of the mask near the connection to the circuit. As the bag is squeezed one should note chest rise and condensation in the mask, and should hear no air escape which would indicate a leak due to an inadequate seal. Care should be used not to compress the submandibular tissue as this can collapse the airway and make ventilation more difficult.
If mask ventilation proves difficult, one can employ a two‐handed technique in which one provider holds the mask in both hands with their thumbs on top of the mask and remaining digits on the mandible lifting the face into the mask while an assistant squeezes the bag. Oral and nasal airways can also be useful as they pull the tongue and epiglottis away from the posterior wall of the pharynx, allowing more airflow.
Laryngoscopy and confirmation of placement
After ensuring proper preparation, equipment set‐up, functioning monitors, positioning and preoxygenation, the patient is typically administered an apnea‐inducing medication as well as a paralytic agent, both of which are chosen based on patient conditions as well as the clinical situation. It should also be noted that in certain conditions such as cardiac arrest, induction agents may not be necessary.
When the patient is deemed appropriately anesthetized, the laryngoscope is held in the provider’s left hand while the right hand opens the patient’s mouth using his or her thumb and index finger in a scissoring motion. The laryngoscope is then inserted into the mouth using care not to damage the patient’s lips or teeth. In the case of the curved MAC blade, the tongue is swept to the left and the tip of the blade placed in the vallecula just anterior to the epiglottis, while the straight Miller blade is inserted in midline position beneath the epiglottis. The handle of the laryngoscope is lifted upwards and anteriorly, exposing the vocal cords. The handle should never be tilted backwards as this can result in dental damage. The ETT is then inserted through the vocal cords under direct visualization. After ETT insertion, the stylet (if used) is removed as is the laryngoscope. The pilot balloon is then inflated with air using a 10 mL syringe to no more than 30 mmHg of pressure.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.