1 ...6 7 8 10 11 12 ...29 4 No
5 No
Comments: Gingival bleeding is a common finding in other local conditions such as in acute ulcerative and plasma cell gingivitis, or systemic diseases such as Wegener disease and scurvy. The lack of necrosis of interdental papillae (seen in acute ulcerative gingivitis) and the erythematous and edematous red attached gingivae (in plasma cell gingivitis) or the erythematous swollen‐like‐strawberries gingivae (in Wegener disease) and the ulcerated, swollen gingivae with deep pocketing (in scurvy) exclude the above diseases from the diagnosis.
Q2Which laboratory tests are routinely used for the diagnosis of this condition?
1 White blood count
2 Immunophenotypic analysis with flow cytometry
3 Bone marrow biopsy
4 Urine analysis
5 Cerebral fluid biochemical analysis
Answers:
1 White blood count shows an increased number of lymphocytes (>10,000 cells/mm3).
2 The flow cytometric analysis of the bone marrow aspiration cells and peripheral blood cells with the use of a series of monoclonal antibodies allow the identification of hematologic malignancies including chronic lymphocytic leukemia (CLL).
3 Bone marrow biopsy is used in undiagnosed cases of blood dyscrasias showing the replacement of bone marrow cells with pathologic lymphocytes.
4 No
5 No
Comments: Urinalysis and cerebrospinal fluid (CSF) analysis are useful only in a diagnosis of aggressive leukemias like CLL, involving bladder and brain respectively.
Q3Which other conditions are associated with this disease?
1 AnemiaThrombocytopeniaEosinophiliaComplement deficiencyParaproteinemiaAnswers:Anemia is a very common complication of CLL due to: (i) bone marrow accumulation of abnormal lymphocytes inducing the replacement of stem cells producing red cells; (ii) increased production of tumor necrosis factor (TNF) that suppresses red blood cell production; (iii) increased red cell destruction by circulated auto‐antibodies; and (iv) medications used for treatment of CLL that suppress red cell production.Thrombocytopenia is responsible for the increased bleeding tendency among patients with CLL.Eosinophilia is sometimes a preclinical sign of various hematological malignancies including lymphomas and CLL.Complement deficiency is a common finding and seems to limit CD20 monoclonal cytotoxicity in treatment’s efficacy for these patients.Monoclonal proteins are present in significant number of patients with CLL.
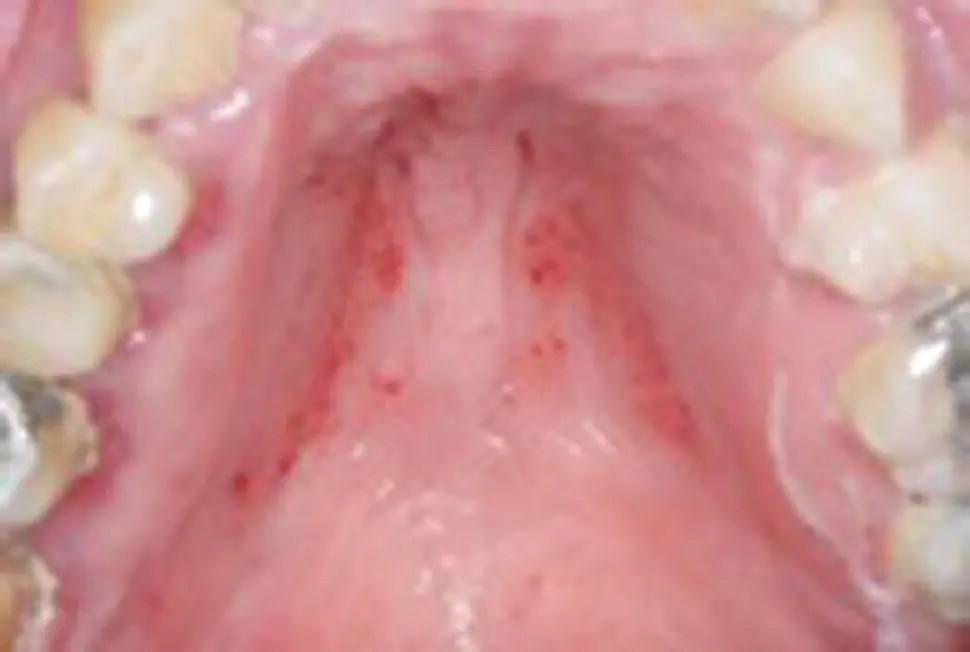
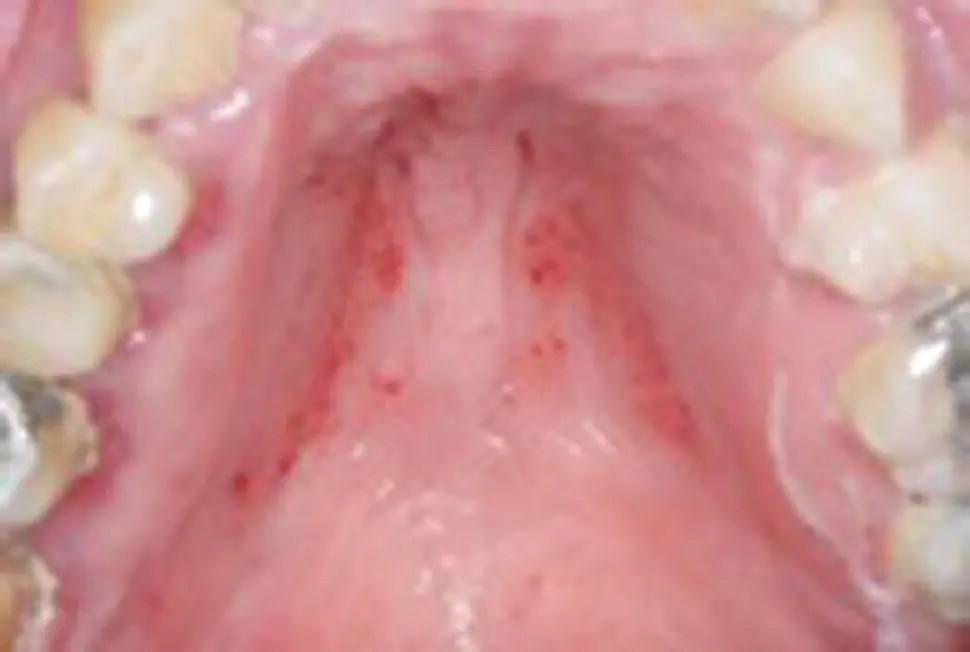
Figure 1.9
CO: A 32‐year‐old woman was presented with red spots on her palate.
HPC: The red palatal lesions were asymptomatic and discovered by her GDP during her regular dental check‐up last week.
PMH: Her medical history revealed an asymptomatic HIV infection over the last 14 months and a few opportunist lung infections this winter. She was on no medication at the moment apart from a few broad antibiotics taken for her respiratory infections. Her HIV infection was probably caught after a blood transfusion given 10 years ago to recover after a car accident. She was non‐smoker or drinker.
OE: A few scattered red spots on both parts of hard and occasionally soft palate and buccal mucosae. These lesions did not bleach with pressure, but were associated with severe periodontal disease regardless of her young age ( Figure 1.9) and cervical lymphadenitis.
Q1What is the cause of palatal petechiae?
1 Fellatio
2 Infectious mononucleosis
3 Nicotinic stomatitis
4 HIV‐induced thrombocytopenia
5 Rendu‐Osler‐Weber syndrome
Answers:
1 No
2 No
3 No
4 Palatal petechiae on this lady appear due to thrombocytopenia induced by HIV infection. This is one of the early manifestations of the disease such as atypical oral ulcerations, infections like pseudo‐membranous or erythematous candidiasis, reactivation of herpes zoster infection and acute ulcerative gingivitis/periodontitis.
5 No
Comments: Rendu‐Osler‐Weber syndrome can be easily excluded, as this is about having scattered telangiectasia since childhood, in contrast with the hemorrhagic spots (petechiae) that were found in this young lady. Asymptomatic petechiae are also seen on the soft palate and on margins of the hard with the soft palate after orogenital sex, which this lady had not reported. Asymptomatic palatal red spots are characteristics in nicotinic stomatitis, but the red spots there represent the inflamed duct openings of minor salivary glands and not petechiae. Palatal petechiae associated with general lymphadenopathy are also seen in patients with infectious mononucleosis, but the typically increased number of monocytes in the blood test and positive mononucleosis (mono) test, excludes this condition from diagnosis.
Q2Which is/are the difference/s between petechiae and purpura?
1 Size
2 Location
3 Reaction to pressure
4 Symptomatology
5 Shape
Answers:
1 Petechiae are hemorrhagic spots with a diameter of <5 mm while purpura have a 5–9 mm diameter.
2 No
3 No
4 No
5 Petechiae have round, regular lesions while the shape of purpura and ecchymoses may be irregular.
Comments: Both hemorrhagic lesions do not blanch with pressure, are usually asymptomatic and can be found anywhere in the body.
Q3What are the causes of thrombocytopenia apart from an HIV infection?
1 Leukemia
2 Epilepsy
3 Hepatitis C infection
4 Heavy alcohol consumption
5 Anorexia nervosa
Answers:
1 Thrombocytopenia is very common sign of an acute myelogenous and lymphocytic leukemia, as well as in advanced chronic lymphocytic and in progressive myelogenous leukemia. The reduced number of platelets has been attributed to: (i) bone marrow replacement by leukemic cells; (ii) increased destruction of platelets by swollen spleen or cytotoxic drugs for leukemia treatment; and (iii) immune destruction of platelets in some CLL cases.
2 No
3 Thrombocytopenia is a major problem in HCV+ patients as it interferes with various measurements for its diagnosis and follow‐up. The cause of thrombocytopenia is multifarious and is due to: (i) immunogenicity; (ii) direct bone marrow suppression; (iii) hypersplenism; (iv) decreased production of thrombopoeitin; and (v) drug reactions.
4 The chronic use of alcohol affects the production, survival time and functions of platelets while it also increases their destruction rate by an enlarged spleen leading to thrombocytopenia. The cessation of drinking within the second week raises the number of platelets again.
5 Anorexia nervosa causes thrombocytopenia. The reduced production of platelets is attributed mainly to low thrombopoietin rather than folic acid levels due to malnutrition.
Comments: Anti‐epileptic drugs such as valproate and levetiracetam but not the disease per se cause thrombocytopenia.

Figure 1.10
CO: A 42‐year‐old man was admitted with gingival bleeding since the previous night.
HPC: The bleeding started suddenly after eating a snack with potato chips and became more intense and constant on the lower molar gingivae. No similar bleeding episodes had been reported previously by him or his close relatives.
Читать дальше