Q2What other symptoms accompanied this breath disturbance?
1 Metallic taste
2 Burning sensation
3 Sense of xerostomia
4 Stomatodynia
5 Pruritus
Answers:
1 Taste alteration like metallic taste is a common symptom in patients with severe anxiety, and especially in those with halitophobia.
2 Burning sensation is part of the burning mouth syndrome and often appears together with the delusion of bad breath.
3 The sense but not the presence of dry mouth is a common finding in patients under severe stress, depression, and halitophobia.
4 Stomatodynia is a clinical complaint of patients with severe depression and anxiety and sometimes comes together with halitophobia.
5 Pruritus is a chronic itching of the skin of face and body that is caused by a number of factors among which anxiety plays an important role and is sometimes accompanied with halitophobia.
Q3Which other conditions have been linked with this condition?
1 Hypochondria
2 Brain tumor
3 Obsessive compulsive syndrome
4 Olfactory reference syndrome
5 Parkinson's disease
Answers:
1 Hypochondria is a somatic symptom disorder characterized by a persistent fear of having an undiagnosed disease which sometimes could cause bad breath.
2 No
3 This disorder is characterized by chronic, uncontrollable thoughts (i.e. worry about bad breath or fear of germs) and continuously repeated behaviors.
4 Olfactory reference syndrome is a psychiatric condition which involves a false belief of an existing body odor that is offensive to other individuals.
5 No
Comments: Both Parkinson's disease and brain tumors cause existing and not hallucinated bad breath, as it is easily detected by other people as a result of xerostomia, poor oral hygiene and main treatment side effects (drugs or surgery).

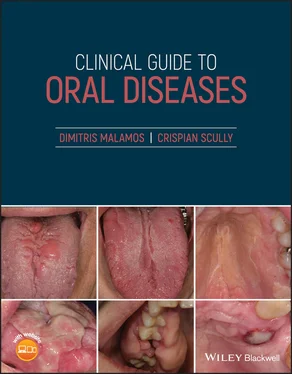
Figure 4.6
CO: A 67‐year‐old woman was presented with multiple bullae on her mouth which could easily break and leave painful ulcerations and bad breath as well.
HPC: The oral lesions appeared one year ago, as flaccid small bullae on the floor of the mouth and buccal mucosae which were easily broken with mastication, thus leaving scattered painful ulcerations. These lesions were accompanied by bad breath.
PMH: Chronic lymphocytic leukemia was diagnosed two months ago and partially responded to two courses of a combined chemotherapy with fludarabine, cyclophosphamide, and rituximab together with plasmapheresis.
OE: Multiple superficial erosions and not intact bullae were found on her palate, floor of the mouth and buccal mucosae. Her gingivae were erythematous, swollen, and bled with probing ( Figure 4.6). Nikolsky sign was positive as a small bulla which appeared with gingival rubbing, but is easily broken with slight pressure. Her oral hygiene was poor, causing periodontal problems and caries in her remaining teeth. Gingival biopsy revealed acantholysis at the lower epithelial layers with intra‐epithelial bulla formation and positive immune‐fluorescence (direct and indirect). The bad breath like rotten fruit was obvious and remained unchanged over the days.
Q1Which is the main cause of her bad breath?
1 Pemphigus vegetans
2 Paraneoplastic pemphigus
3 Benign mucous membrane pemphigoid
4 Caries
5 Periodontitis
Answers:
1 No
2 Paraneoplastic pemphigus was the cause of halitosis. This bad breath was attributed to excessive volatile gas production from numerous pathogenic bacteria which grew within the inflamed oral ulcerations in this woman with a positive history of hematological malignancy.
3 No
4 No
5 No
Comments: The halitosis from pemphigus vulgaris, pemphigoid, or paraneoplastic lesions is indistinguishable and the diagnosis of the responsible bullous disorder should be based on the patient's clinical and histological characteristics, immunological profile and association or not with serious diseases. The bad breath was also reinforced by the patient's chronic periodontitis, caries, and inadequate tooth brushing.
Q2Which of the neoplasms below is mostly related with this bullous condition?
1 Carcinomas
2 Non‐Hodgkin lymphoma (NHL)
3 Thymoma
4 Sarcomas
5 Melanomas
Answers:
1 No
2 NHL is the most frequent hematologic neoplasm that is associated with paraneoplastic pemphigus.
3 No
4 No
5 No
CommentsAll these tumors usually preexist the oral lesions in paraneoplastic pemphigus, with a declining association starting with NHL, followed by a chronic lymphocytic leukemia, carcinomas, sarcomas, and least likely, melanomas.
Q3Which auto‐antibodies (abs) are characteristics of a paraneoplastic pemphigus?
1 Desmoglein 1 abs
2 Desmoglein 3 abs
3 Anti‐smooth muscles abs
4 Anti‐neutrophil cytoplasmic abs
5 Plakins (envo; peri; desmo) abs
Answers:
1 No
2 Desmoglein 3 rather than 1 Abs have been implicated with the pathogenesis of paraneoplastic pemphigus.
3 No
4 No
5 Envoplakins (210 kDa); periplakins (190 kDa) and desmoplakins (250 kDa) play a crucial role in combination with cellular immunity in the pathogenesis of paraneoplastic pemphigus.
Comments: Auto abs against desmoglein 1 are detected in pemphigus foliaceus but rarely in paraneoplastic. Anti‐smooth muscle and anti‐neutrophils cytoplasmic abs are not found in paraneoplastic pemphigus, but are pathognomonic of autoimmune liver disease and necrotizing vessel vasculitides.

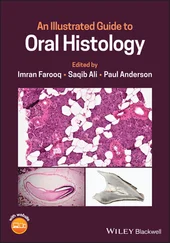
Figure 4.7
CO: A 37‐year‐old man presented for an evaluation of his repellent odor.
HPC: His breath had a strong acetone like odor and was first perceived two months ago by his therapist who tried to help him to stop his drinking habit.
PMH: His medical history did not reveal any serious diseases or drug abuse apart from alcoholism that was diagnosed five years ago, and treated with counseling and use disulfiram (Antabuse) drug over the last two months.
OE: The oral examination revealed a neglected dentition with missing teeth, decays, and external stains as well as mature plaque and food debris on most of his remaining teeth whose gingivae were inflamed ( Figure 4.7). A strong acetone‐like odor was easily noticed and remained unchanged during his examination.
Q1Which is the main cause of his halitosis?
1 Alcohol overuse
2 Poor oral hygiene
3 Caries
4 Gingival disease
5 Drug‐induced
Answers:
1 No
2 No
3 No
4 No
5 Dusilfiram‐induced halitosis is the answer. This drug is used to stop alcoholism by inhibiting acetaldehyde dehydrogenase and inducing a hangover effect after alcohol consumption. The metabolism of this drug enhances the acetone concentration in the blood which is finally transferred to the pulmonary alveoli and excreted into exhaled air, thus producing the characteristic odor.
Comments: Halitosis induced by periodontitis has a chronic, constant fruity odor in contrast with the acetone‐like odor induced by dusilfiram, while the halitosis from poor oral hygiene, caries, and alcohol use are temporary and can disappear with brushing, restorations, and withdrawal of alcohol.
Читать дальше