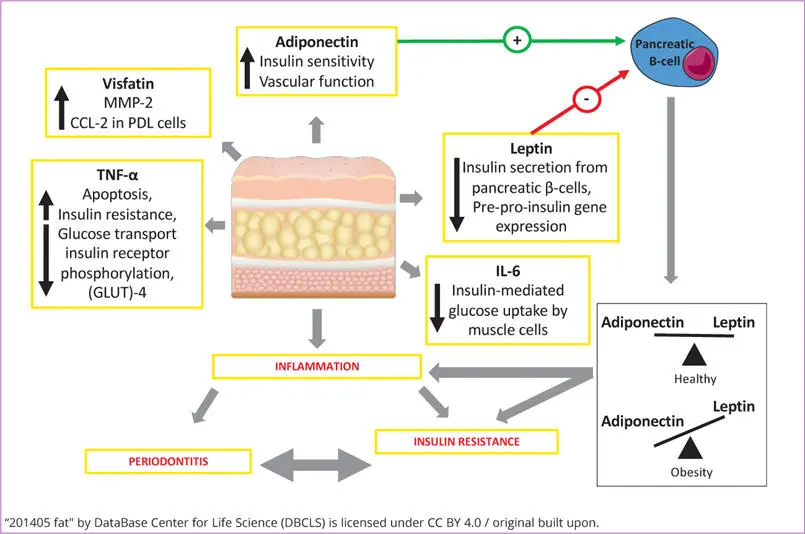
Another important adipokine is visfatin. It is increased in obesity and other systemic diseases. Visfatin can generate reactive oxygen species (ROS) comprising both superoxide and hydrogen peroxide (H 2O 2) and producing oxidative stress 166. Nokhbehsaim et al 167observed that visfatin upregulates gene expressions of matrix-metalloproteinase (MMP)-1 and C-C motif chemokine ligand (CCL)-2 in periodontal ligament cells. MMP-1 plays a critical role in modelling and remodelling of the periodontal extracellular matrix by degradation of collagens 167. Clinical studies have already demonstrated that gingival levels of MMP-1 are enhanced at sites of periodontitis and can be reduced by periodontal treatment 168 , 169. Therefore, it could be a molecule by which obesity mediates its detrimental effects on the periodontium.
Studies have shown that visfatin and leptin increase the synthesis of pro-inflammatory and proteolytic molecules, whereas adiponectin downregulates the production of these molecules in periodontal cells 145. This might explain the association with obesity and compromised healing after periodontal therapy, as well as poor periodontal regeneration. However, the mechanisms underlying the association between obesity and periodontitis or compromised periodontal healing are not well understood. Taken together, adipokines not only contribute to the subclinical inflammatory state in obesity, but also are a critical mechanistic link between obesity, diabetes and periodontal infection (Fig 1-4). Increased plasma levels of these pro-inflammatory adipokines, as observed in a number of systemic diseases, could make affected individuals more susceptible to periodontal infection and destruction.
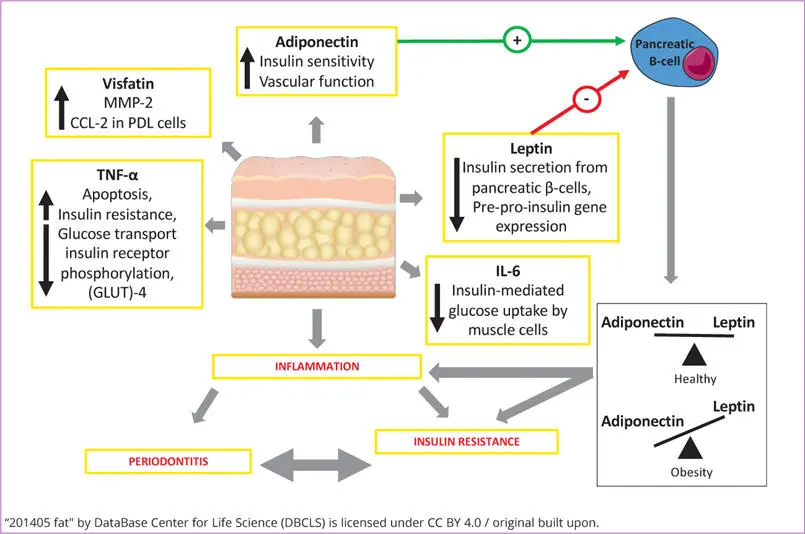
Fig 1-4 The role of adipokines in inflammation (CCL-2 = C-C motif chemokine ligand 2; IL = interleukin; MMP = matrix metalloproteinase; PDL = periodontal ligament cell; TNF-α = tumour necrosis factor alpha).
1.3.4 Oxidative stress
ROS have emerged as important signalling molecules in various cellular processes. These molecules originate from molecular oxygen and can damage proteins, lipids and DNA if not neutralised by anti-oxidant substances. Their production is central to the progression of many inflammatory diseases, but at physiological concentrations, they act as second messengers to regulate mitosis, apoptosis and cell differentiation. ROS, such as superoxide, can rapidly combine with nitric oxide (NO) to form reactive nitrogen species (RNS), such as peroxynitrite, leading to a nitrosative stress, which adds to the pro-inflammatory burden of ROS 170. Oxidative stress is induced by an imbalance between excessive ROS production and anti-oxidant mechanisms. Increased levels of ROS leading to a state of oxidative stress have been implicated in the pathogenesis of a large number of diseases, including cardiovascular diseases 171and diabetes 172. Several animal and human studies have demonstrated a crucial role of ROS in periodontal tissue destruction 173 - 175.
In physiological and, even more, in pathological conditions, adipokines induce the production of ROS, generating oxidative stress and, in turn, production of further adipokines. Upon activation, immune cells generate free radicals, which promote an inflammatory status. For instance, TNF-α, IL-1 and IL-6 induce an increase in ROS and RNS in macrophages and monocytes. Consequently, ROS also induce further release of pro-inflammatory cytokines and expression of adhesion molecules and growth factors, such as connective tissue growth factor, insulin-like growth factor-1, platelet-derived growth factor, and vascular cell adhesion molecule-1 176.
The comorbid presence of periodontitis with diabetes has been shown to associate with reduced plasma small molecule antioxidant capacity and increased plasma protein carbonyl damage. In the same study, diabetes patients with periodontitis had reduced beta-cell function (HOMA-b), elevated hsCRP and lower levels of HDL-cholesterol. The study concluded that the comorbid presence of periodontitis with T2DM was associated with increased peripheral oxidative stress and dyslipidaemia 177.
Evidence that obese patients exhibit a generalised systemic inflammatory state was provided in a study of the impact of bariatric surgery on peripheral blood neutrophil phenotypes prior to and 3 months following gastric band placement. Peripheral neutrophils from obese patients demonstrated excessive ROS and pro-inflammatory cytokine production relative to non-obese controls, as well as exaggerated neutrophil extracellular trap (NET) formation and impaired directional chemotactic accuracy. Such features are consistent with a high propensity for tissue damage. Bariatric surgery led to a normalisation of neutrophil ROS, NET and cytokine production, but chemotactic accuracy remained impaired. The data pointed towards a reduced ability of peripheral neutrophils in obese patients to eliminate infection, whilst at the same time a propensity for neutrophil-mediated tissue damage during physiological reactions 178.
Bastos et al 133observed higher levels of GCF markers of lipid peroxidation in DM patients, which was correlated with clinical parameters of periodontitis and GCF concentrations of inflammatory mediators. In addition, Atabay at al 174observed an increase in the levels of malondialdehyde and protein carbonyl groups, two oxidative stress biomarkers, and decreases in the levels of total antioxidant capacity in GCF from obese subjects with periodontitis, compared with normal-weight controls. This study shows that the combination of obesity and periodontitis appears to facilitate a pro-oxidative state with diminished antioxidant capacity within periodontal tissues. Thus, in the presence of sufficient primary aetiological factors capable of inducing periodontitis, such as poor plaque control, obesity may exacerbate periodontal tissue destruction and disease severity 179.
1.3.5 Nitric oxide
Nitric oxide (NO) appears to be one of the most important free radicals involved in periodontitis and it has dual effects. In low concentrations, it induces relaxation of blood vessels, reducing blood pressure, preventing platelet aggregation and adhesion, limiting oxidation of low-density lipoprotein (LDL), inhibiting proliferation of smooth muscle cells, and decreasing the expression of pro-inflammatory genes that are associated with atherogenesis. However, when NO is highly expressed, mainly by the enzyme inducible nitric oxide synthase (iNOS), it can interact with O 2 •−leading to the production of peroxynitrite, which post-transcriptionally modifies proteins and negatively affects their function 180. Several studies have already demonstrated that iNOS increases NO expression in periodontitis and that its inhibition reduces osteoclast differentiation, and consequently bone loss 174 , 175.
In an animal study, Campi et al 181observed that ligature-induced periodontitis led to the development of endothelial dysfunction. The inducible nitric oxide synthase (NOS)-derived NO and cyclooxygenase-2 (COX-2)-derived prostanoids were among the endothelial factors that mediated the observed dysfunction. In diabetes, both NO and COX-2 are also increased, as discussed further below. A meta-analysis, including 30 studies, showed that serum or plasma NO levels are higher in both T1DM and T2DM patients compared with non-diabetes controls. These studies support the hypothesis that high levels of nitrate and nitrite (the stable NO product) are associated with adverse clinical events observed in diabetes patients, such as endothelial dysfunction, insulin resistance, pancreatic beta-cell dysfunction and possible increase of severity and incidence of periodontitis 182.
Читать дальше





![John Bruce - The Lettsomian Lectures on Diseases and Disorders of the Heart and Arteries in Middle and Advanced Life [1900-1901]](/books/749387/john-bruce-the-lettsomian-lectures-on-diseases-and-disorders-of-the-heart-and-arteries-in-middle-and-advanced-life-1900-1901-thumb.webp)