1 ...7 8 9 11 12 13 ...21 Table 1-5 Clinical studies assessing the epidemiological association between periodontitis and T1DM
| Type of study |
Study, country |
Subjects |
Findings |
| Case-cohort |
Firatli 109, Turkey |
44 subjects with T1DM and 20 healthy controls. Length of the study: 5 y. |
CAL was higher in the T1DM subjects. Positive correlation between the duration of diabetes and CAL. Fructosamine was correlated with the Gingival Index in the T1DM group. |
| Case-control |
Ajita et al 110, India |
28 subjects with T1DM and 20 healthy controls. |
T1DM had greater Bleeding Index, PPD and CAL. Patients diagnosed for diabetes for shorter duration of time (4–7 y) showed Bleeding Index-disease severity correlation. |
| Kaur et al 111, Germany |
145 subjects with T1DM paired with 2647 healthy controls, and 182 T2DM paired with 1314 healthy controls. |
T1 and T2DM had greater CAL. After age stratification, the effect of T2DM was only statistically significant in the 60–69-year-old subjects. T1DM was positively associated with tooth loss. The association between T2DM and tooth loss was statistically significant only for females. |
| Silvestre et al 112, Spain |
90 subjects with T1DM and 90 healthy controls. |
T1DM had greater Bleeding Index, PPD and CAL. Deficient metabolic control and presence of diabetic complication were associated with higher BoP and PPD. |
| Lalla et al 113, USA |
350 children with T1DM and 350 healthy (6–18 y old). 7% had T2DM. |
DM had increased gingival inflammation and CAL than healthy controls with OR ranging from 1.84 to 3.72. |
| Al-Shammari et al 114, Kuwait |
29 subjects with T1DM of ≤ 5 y duration and 29 subjects with T1DM of > 5 y duration. |
T1DM of > 5 y duration had greater number of missing teeth and CAL. Patients with one or more DM complications had greater number of missing teeth and CAL. |
| Pinson et al 115, USA |
26 subjects with T1DM and 24 healthy controls. |
No differences in CAL, PPD, recession, Gingival Index, Plaque Index, gingival fluid flow, or BoP. Site-specific comparison measurements showed the Gingival Index to be somewhat higher among the T1DM subjects. Examination of interaction effect plots showed the T1DM subjects to have higher average Gingival Index for most teeth and higher or the same Plaque Index levels on all teeth relative to controls. |
| Case-control |
Seppälä et al 116, Finland |
38 dentate subjects with a mean duration of 18 years of T1DM. |
After 1 and 2 y from baseline, the poorly controlled T1DM subjects exhibited higher BoP than T1DM subjects. After 2 y from baseline, the poorly controlled T1DM subjects exhibited more sites with loss of approximal alveolar bone than T1DM subjects. |
| Seppälä et al 117, Finland |
38 dentate subjects with a mean duration of 18 years of T1DM. |
At baseline and after 1 and 2 y from baseline the poorly controlled T1DM subjects had more gingivitis and BoP than the controlled T1DM subjects. |
| de Pomme- reau et al 118, France |
85 subjects with T1DM and 38 healthy controls. |
T1DM children had more gingival inflammation than healthy controls. |
| Cross-sectional |
Patiño Marín et al 119, Mexico |
35 subjects with T1DM with HbA1c between 6.5% and 7%; 35 subjects with T1DM with HbA1c > 7%; 35 subjects without T1DM; 35 subjects with T2DM; and 35 subjects without T2DM. |
No differences among in frequency of caries, filled teeth, missing teeth, prosthetic restoration, bacterial dental plaque, Calculus Index, PPD and CAL between T1DM and healthy controls. T2DM subjects had more missing teeth, calculus, PPD and CAL. |
| Patiño Marín et al 120Mexico |
20 subjects with uncontrolled T1DM, 20 subjects with controlled T1DM, and 40 healthy controls. |
The imbalance of glucose of subjects with T1DM was associated with more frequency of periodontal disease. |
BoP = bleeding on probing; CAL = clinical attachment level; HbA1c = glycated haemoglobin; OR = odds ratio; PPD = pocket probing depth; T1DM = type 1 diabetes; T2DM = type-2 diabetes.
SUMMARY
● The prevalence of diabetes is 13.1% among subjects with periodontitis and 9.6% among subjects without periodontitis according to a 2018 meta-analysis.
● There is strong evidence for an association between periodontitis and glycaemic status, expressed as HbA1c, fasting blood glucose levels and/or glucose tolerance test, the latter in people without diabetes.
● HbA1c is significantly reduced at 3 to 4 months following periodontal therapy. However, there are insufficient data to demonstrate that this effect is maintained after 6 months.
● Some studies identified that periodontitis increases insulin resistance (HOMA-IR levels) in people with diabetes.
● People with diabetes and periodontitis are more likely to suffer from diabetes-related complications than people with diabetes only.
1.3 Cellular and molecular mechanisms
The principal mechanisms that link oral infection with systemic diseases are:
● metastatic spread of infection from the oral cavity as a consequence of transient bacteraemia
● metastatic spread of cellular injuries because of the circulation of oral bacterial toxins
● metastatic spread of inflammation triggered by oral bacteria 121.
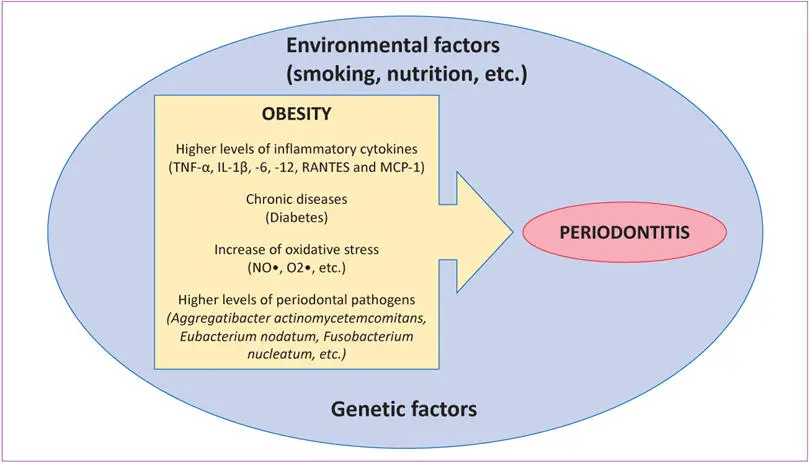
In obesity, the mechanism behind its impact on periodontitis is still controversial. However, inflammation and the role of cytokines are surely of great importance in explaining a possible mechanism. Obesity is associated with a state of chronic low-grade systemic inflammation. Evidence from animal and human studies demonstrates a clear association between weight regulation and inflammation, with abnormalities of innate and adaptive immune function, including elevated serum levels of inflammatory cytokines, such as IL-5, -10, -12, -13, interferon (IFN)γ and TNF-α and peripheral blood lymphocyte subpopulation levels 122. For example, in obese mice under a high-fat diet, pro-inflammatory T-helper cells 1 (Th1) and pro-inflammatory M1 macrophages, are activated and produce IFNγ, TNF-α, and IL-12 123 , 124, whereas the differentiation of naïve T cells into anti-inflammatory Th2 and the activity of regulatory T cells (Treg), are reduced 125. Moreover, as explained earlier, periodontal pathogen populations may be altered in obese subjects possibly leading to a higher virulence of the periodontal pathogens in those patients (Fig 1-1).
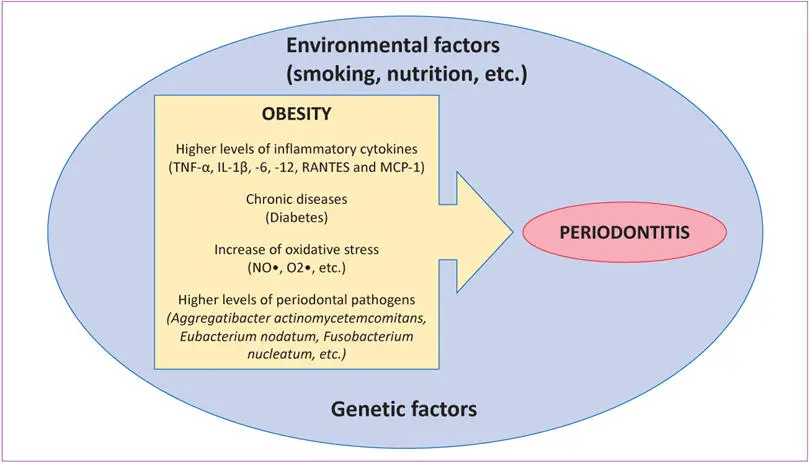
Fig 1-1 Potential mechanism linking obesity to periodontitis. Obesity increases the levels of inflammatory cytokines, oxidative stress and levels of periodontal pathogens, and can lead to diabetes mellitus, increasing the prevalence and severity of periodontitis. Environmental and genetic factors modulate both diseases. (IL = interleukin; MCP-1 = monocyte chemoattractant protein-1; TNF-α = tumour necrosis factor alpha.)
Many studies have demonstrated that adipose tissue cells (adipocytes, pre-adipocytes and macrophages) secrete cytokines and over 50 other bioactive substances collectively known as adipokines, explaining the low-grade systemic inflammation observed in obesity 126. However, there are conflicting results regarding which cytokines play the main role in an obesity-periodontitis association. For example, high levels of TNF-α in plasma 127and gingival crevicular fluid (GCF) 128were found in obese subjects. On the other hand, Saxlin et al 129observed that serum IL-6, but not TNF-α, may mediate the possible inflammatory effect of body weight on the periodontium.
Читать дальше





![John Bruce - The Lettsomian Lectures on Diseases and Disorders of the Heart and Arteries in Middle and Advanced Life [1900-1901]](/books/749387/john-bruce-the-lettsomian-lectures-on-diseases-and-disorders-of-the-heart-and-arteries-in-middle-and-advanced-life-1900-1901-thumb.webp)