The perception of pain is multidimensionaland occurs in several cortical sites. S1and S2are associated with the sensory‐discriminative features of pain. The earliest activation of cortex in response to pain is in the “S2” sensory‐discriminative area (Granovsky et al. 2008). The medial limbic cortex, ( rostral anterior cingulatecortex) mediates the affective, motivational aspects of pain. Other structures contribute to the impact of pain on motor behavior ( basal gangliaand cerebellum), sympathetic tone ( insula), and alertness ( periaqueductal gray) (Liu et al. 2011). It is arguable whether all are properly referred to as “perception” but a better term has not arisen. Perception occurs as a complex temporal and spatial series of events varying with the type, severity, and persistence of pain. Neuropathic pain results in strong activation of affective and motivational centers in the brain. Unfortunately, persistent pain may be associated with brain atrophy (Baliki et al. 2011).
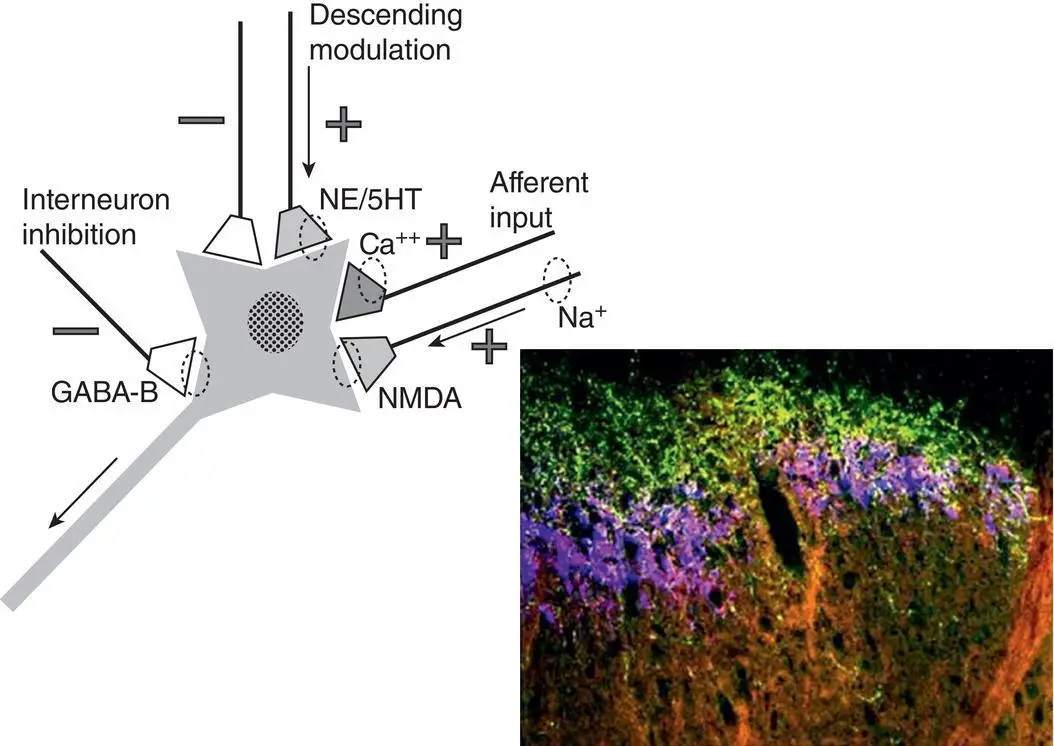
Pain modulation occurs at every level of the nervous system including end‐organs, peripheral nerve, spinal dorsal hornand rostral centers. Key modulation events occur in the dorsal spinal cord where descending fibers, especially from the nucleus raphe magnocellularis(NRM) synapse and control the transmission of nociceptive signals from primary afferent neurons onto second order neurons ( Figure 2.2). This is an important form of gating which has the potential to constrain “pain from accessing the CNS.” The NRM is situated in the ventral midline at the pontomedullary junction. It contains both “ON” and “OFF” cells. ON cellshave the capacity to sensitize an animal to noxious stimuli, effectively turning the pain system “on,” whereas OFF cellshave the capacity to decrease the transmission of nociceptive signals from primary to secondary afferent, effectively turning pain sensitivity “off.” More recently, a role for non‐neuronal cells has been recognized in nociceptive modulation (see Chapter 29).
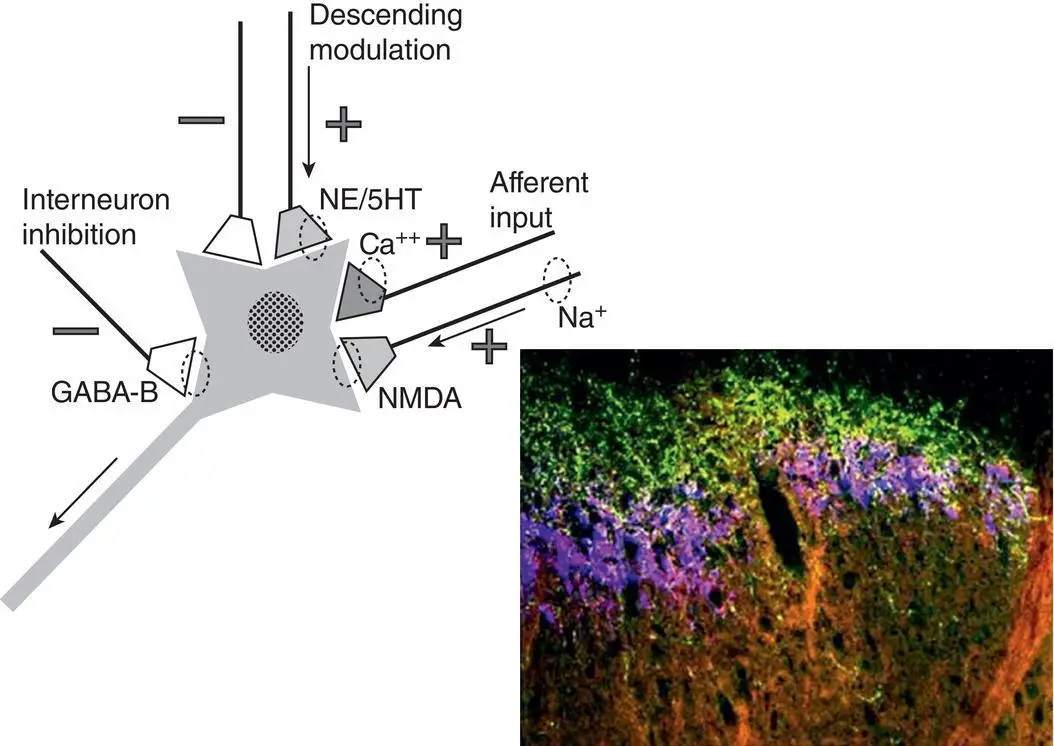
Figure 2.2 Transmission and modulation events in the spinal dorsal horn. Influences on nociceptive processing include: descending inhibition and facilitation, afferent inputs from the periphery and local inhibitory circuits. This is a key site of drug action.
In summary, pain experience arises from the normative functioning of the nociceptive processing system, a complex sub‐system of the nervous system including both neuronal and non‐neuronal elements. Understanding the component elements of the pain processing system: transduction, transmission, perception, and modulation, may aid clinicians in thinking about patients with pain, and lead them to develop more effective diagnostic and treatment plans.
1 Baliki, M.N., Schnitzer, T.J., Bauer, W.R., and Apkarian, A.V. (2011). Brain morphological signatures for chronic pain. PLoS One 6 (10): e26010.
2 Fernández‐Carvajal, A., Fernández‐Ballester, G., Devesa, I. et al. (2012). New strategies to develop novel pain therapies: addressing thermoreceptors from different points of view. Pharmaceuticals 5 (1): 16–48. https://doi.org/10.3390/ph5010016.
3 Granovsky, Y., Granot, M., Nir, R.‐R., and Yarnitsky, D. 'Correspondence information about the author David Yarnitsky (2008). Objective correlate of subjective pain perception by contact heat‐evoked potentials. Journal of Pain 9 (1): 53–63.
4 Liu, C.C., Franaszczuk, P., Crone, N.E. et al. (2011). Studies of properties of “Pain Networks” as predictors of targets of stimulation for treatment of pain. Frontiers in Integrative Neuroscience 5: 80.
5 Ringkamp, M., Raja, S., Campbell, J., and Meyer, R. (2013). Peripheral mechanisms of cutaneous nociception. In: Wall and Melzack’s Textbook of Pain, 6e (eds. M.M. SB, M. Koltzenburg, I. Tracey and D. Turk). Philadelphia, PA: Elsevier Saunders.
6 Stucky, C.L., Dubin, A.E., Jeske, N.A. et al. (2009). Roles of transient receptor potential channels in pain. Brain Research Reviews 60 (1): 2–23.
7 Tominaga, M., Caterina, M.J., Malmberg, A.B. et al. (1998). The cloned capsaicin receptor integrates multiple pain‐producing stimuli. Neuron 21 (3): 531–543.
3 What are the major types of pain?
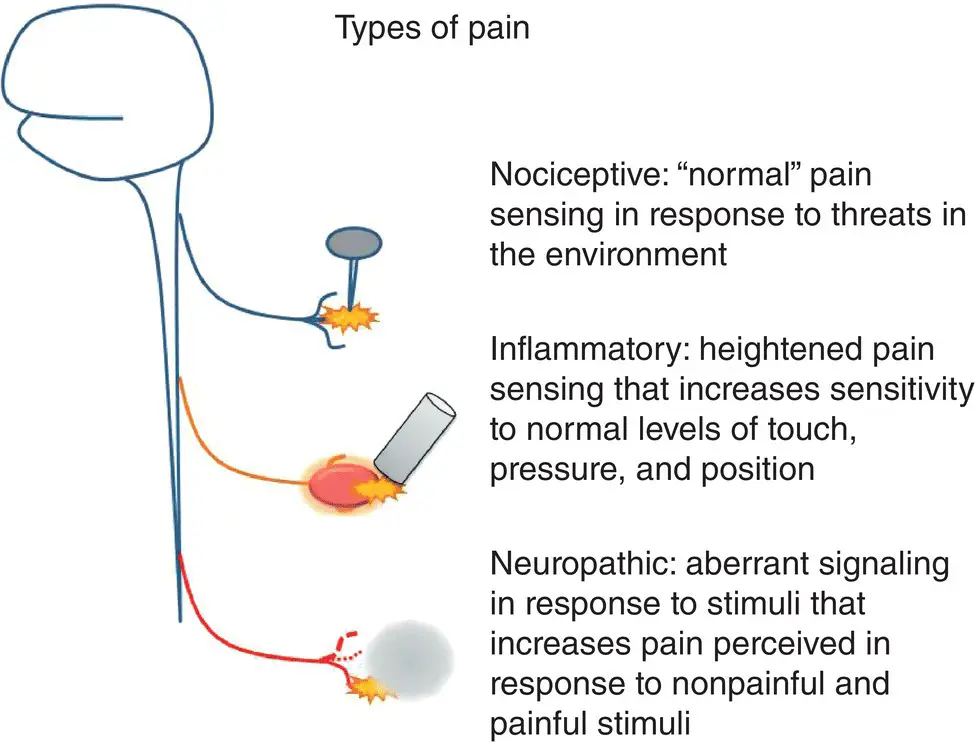
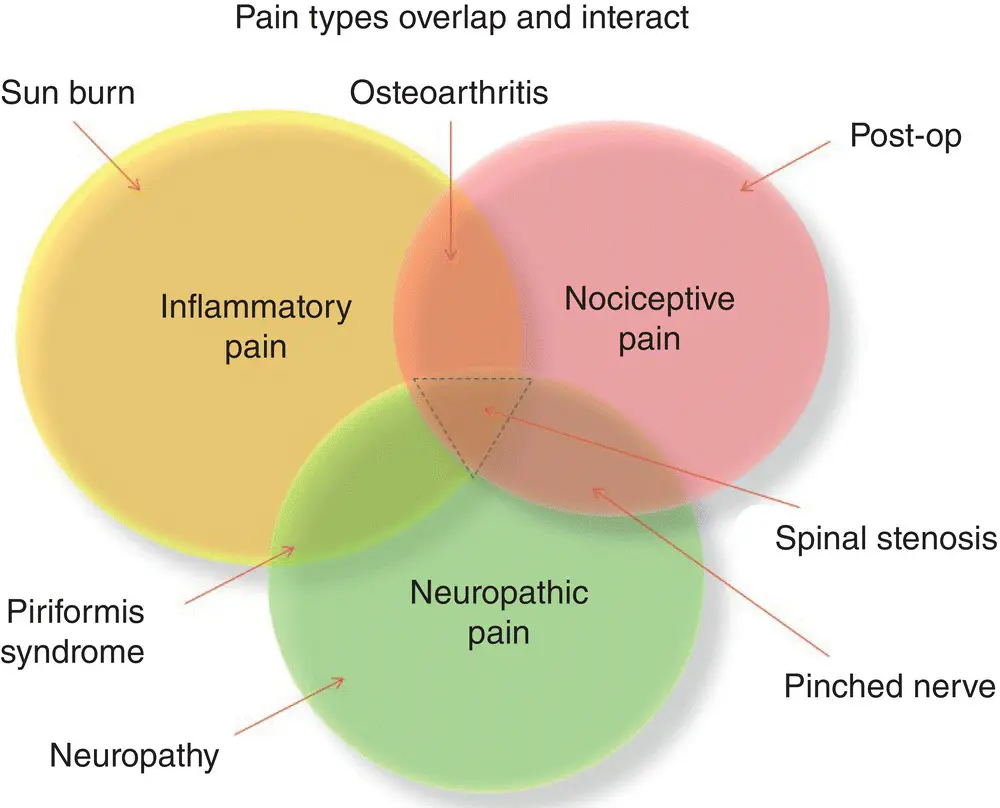
The best approach to understanding and designing effective treatment plans for pain is to view the origins of the problem in terms of basic pain mechanism. This is because the pain mechanism has a major impact on: (i) the potential to diagnose a specific condition, (ii) choose an effective treatment, (iii) prognosticate the patient's course in therapy, and (iv) guide the patient in self‐management. There are three major mechanism‐based types of pain: nociceptive, inflammatory, and neuropathic ( Figures 3.1and 3.2).
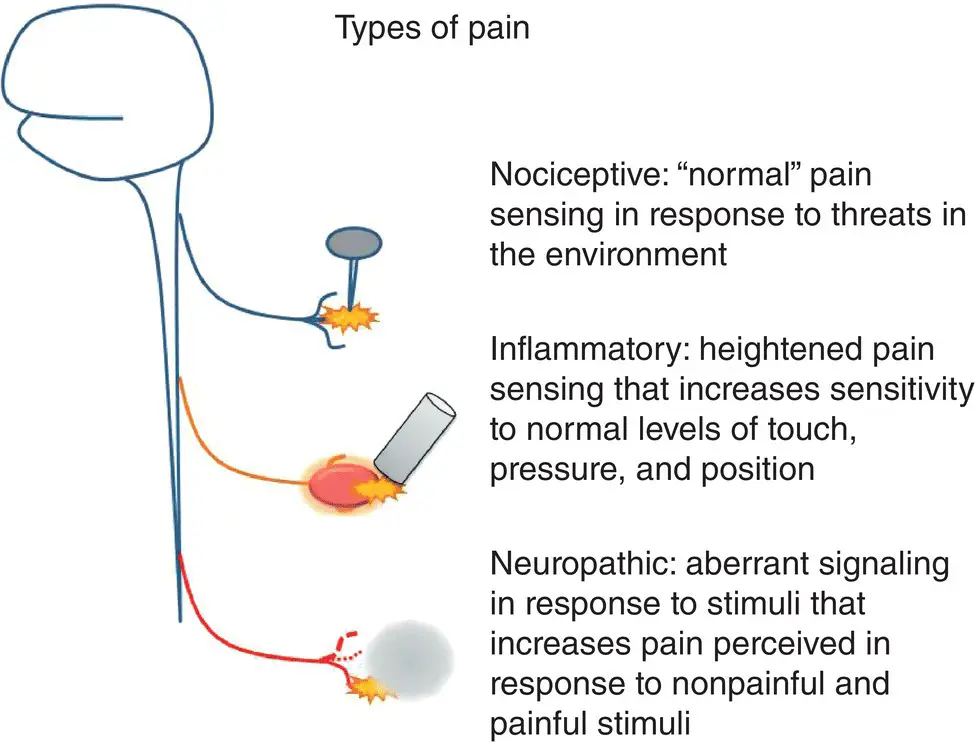
Figure 3.1 The basic mechanisms of pain.
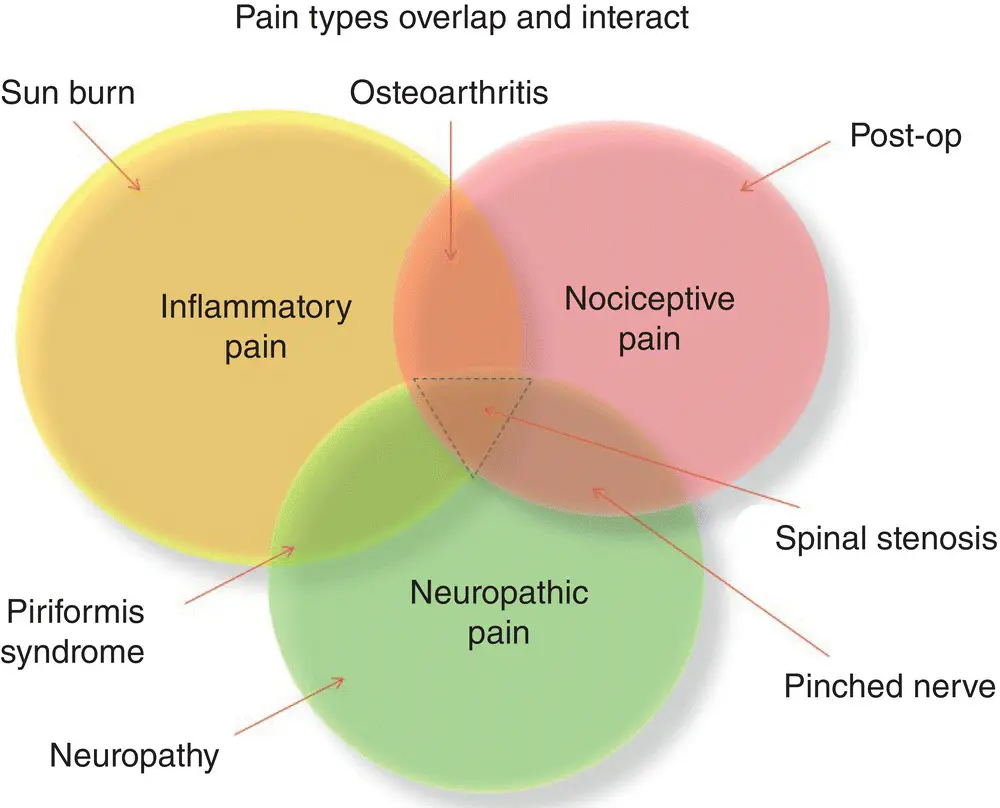
Figure 3.2 How basic pain mechanisms interact.
Nociceptive painis pain arising from acute injury. It is signaled by the normal functioningof the nociceptive processing system ( Chapter 2). Primary afferents in the various parts of the body are activated by peripheral signaling molecules or direct energy transfer. Currently we know that all of the body is innervated by afferents with some exceptions: the nucleus pulposus of the vertebral disc, the brain parenchyma, and cartilage. Signaling molecules involved in nociception include: protons, bradykinin, histamine, acetylcholine and others (Ringkamp et al. 2013). Direct energy transfer can occur from pressure‐type stimuli, thermal stimuli (hot and cold), or electric shock. A specific nociceptive stimulus may be sensed by multiple primary afferents, as there is no one afferent that is exclusively responsible for pain. Thermal stimuli are sensed by multiple fiber types, for example when touching a hot stove, there is “ first pain” that provokes an immediate withdrawal response, mediated by Aδ fibers, and “ second pain” mediated by C fibers that behaviorally reinforce avoidance of damaging stimuli. Nociceptive pain intensity is highly variable depending on personal and contextual factors. Nociceptive pain can be highly responsive to treatments; ideal treatment varies with the intensity, focality, and cause of the pain. In general, mild‐to‐moderate nociceptive pain responds well to over‐the‐counter analgesics, e.g. NSAIDs, acetaminophen; severe nociceptive pain may require opioids or special management strategies such as nerve blocks. Nociceptive pain has a good prognosis, but evidence indicates that very strong nociceptive stimuli may predispose patients to chronic pain.
Inflammatory painis established by exposure to inflammatory signaling molecules and includes pain in response to normally non‐painful stimuli. A classic example of this is osteoarthritis: at first, normal walking activity is uncomfortable; later with continued disease, unbearable. Common examples include sunburn, in which light touch fibers are recruited to signal pain making a bag strap intolerable, and ingrown toenails which can make the pressure of a comfortable shoe excruciating. In inflammatory pain, the primary afferents in the body undergo sensitization by inflammatory signaling molecules, including: Nerve Growth Factor (NGF), Tumor Necrosis Factor‐alpha (TNFα) Interleukin 6 (IL6), bradykinin, protons, and other substances (Ringkamp et al. 2013). The sensitization of the nerve endings results in long‐lasting changes in afferent signaling, termed “ phenotypic switching.” Potentially reversible, the phenotypic switch means that the afferents formerly responsible for nonpainful sensations now signal pain. This is how the pressure of a bag strap or shoe becomes uncomfortable once inflammatory pain signaling is activated. If peripheral inflammation resolves, this increased pain signaling may be reversible. In other situations, such as osteoarthritis, inflammation persists and the pain continues. Inflammatory pain may respond to NSAIDs or corticosteroids, however it is also important to address the origins of inflammatory pain. Specific “ disease‐modifying” therapies include physical therapy, disease‐modifying drugs, ergonomic adaptations, or surgery.
Читать дальше