Table 3.1 Mediastinal lymph node stations with their anatomical correlations.
| Level |
Anatomical correlation |
| Superior mediastinal lymph nodes |
| 1 |
Highest mediastinal |
| 2 |
Upper paratracheal |
| 3 |
Prevascular and retrotracheal |
| 4 |
Lower paratracheal (including azygos nodes) |
| Aortic lymph nodes |
| 5 |
Aortopulmonary (AP) window or subaortic |
| 6 |
Para‐aortic (ascending aorta and phrenic) |
| Inferior mediastinal lymph nodes |
| 7 |
Subcarinal |
| 8 |
Paraesophageal (below carina) |
| 9 |
Pulmonary ligament |
| N1 lymph nodes |
| 10 |
Hilar |
| 11 |
Interlobar |
| 12 |
Lobar |
| 13 |
Segmental |
| 14 |
Subsegmental |
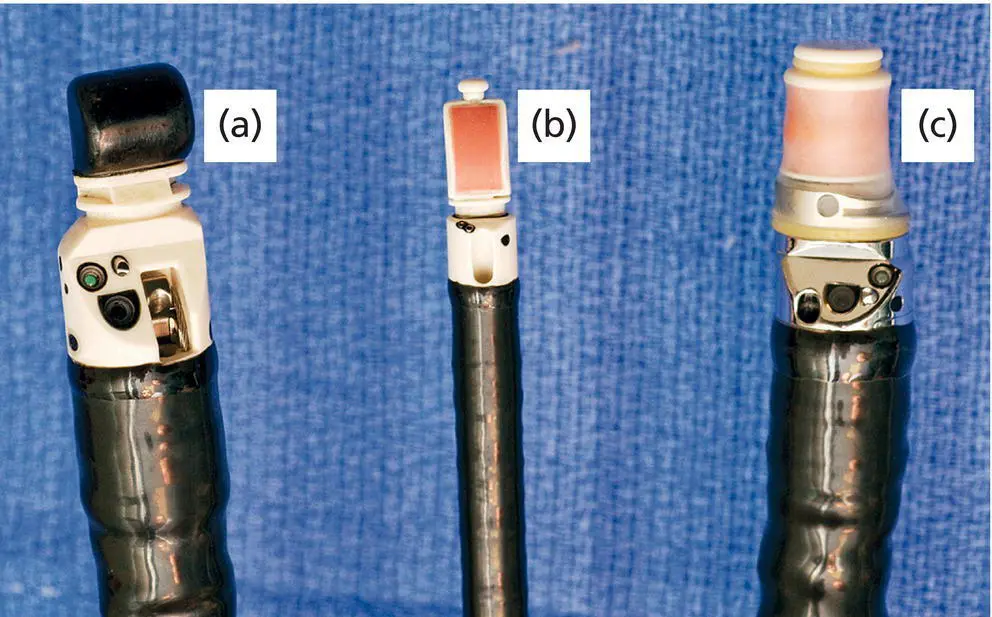
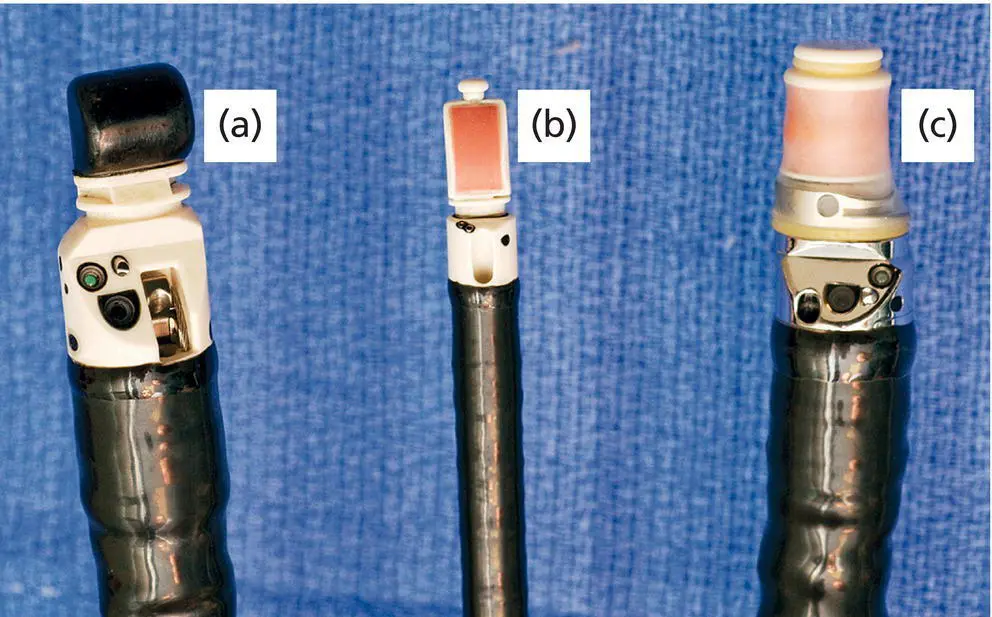
Figure 3.2 Types of echoendoscopes: (a) linear probe; (b) endobronchial probe; (c) radial probe.
Inferior posterior mediastinum
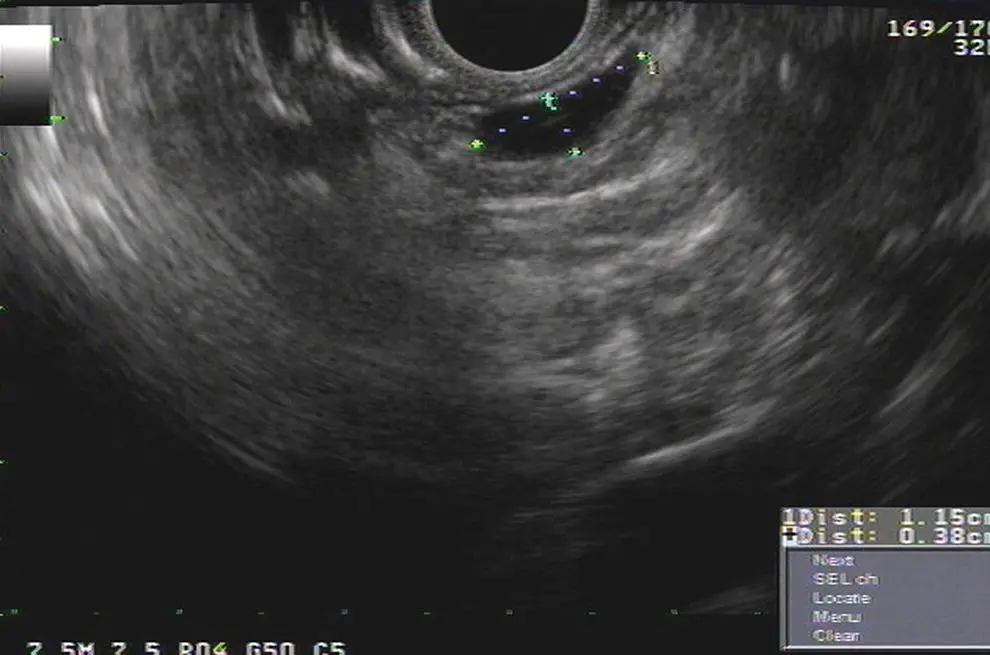
The descending aorta is a large echo‐poor longitudinal structure on linear array with a bright deep wall due to the air interface with the left lung. Clockwise rotation will sequentially image left lung, left pleura, left atrium, right lung, right pleura, azygos vein, and spine. The azygos vein can be localized by rotating approximately 30 degrees counterclockwise from the descending aorta. It is a thin echo‐poor structure that can be followed proximally to its union with the superior vena cava. This is the area of LN stations 8 and 9 ( Figure 3.3).
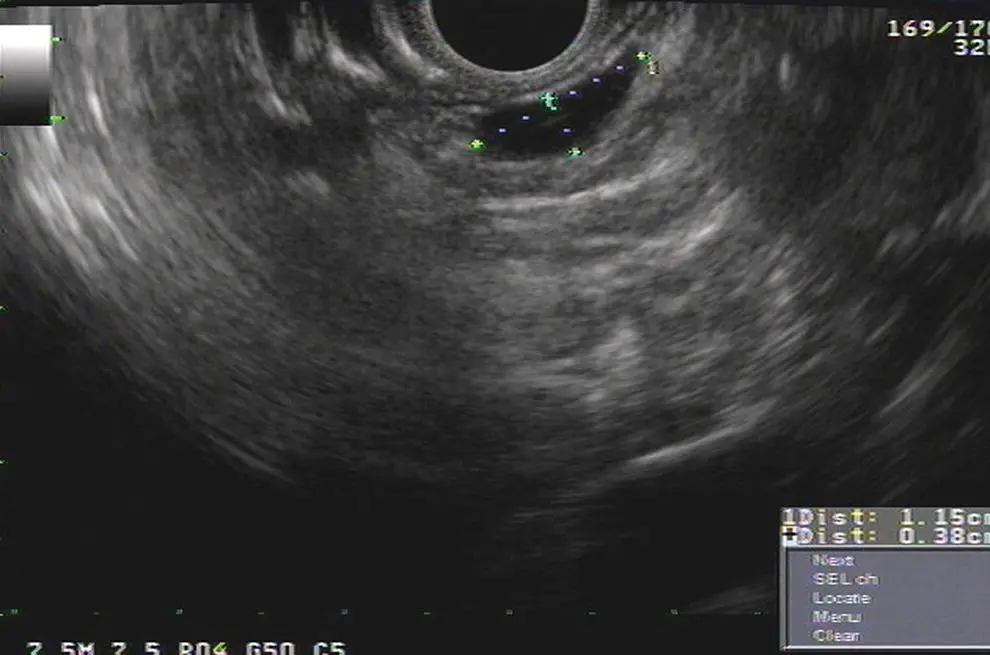
Figure 3.3 Lymph node at station 8 (between calipers).
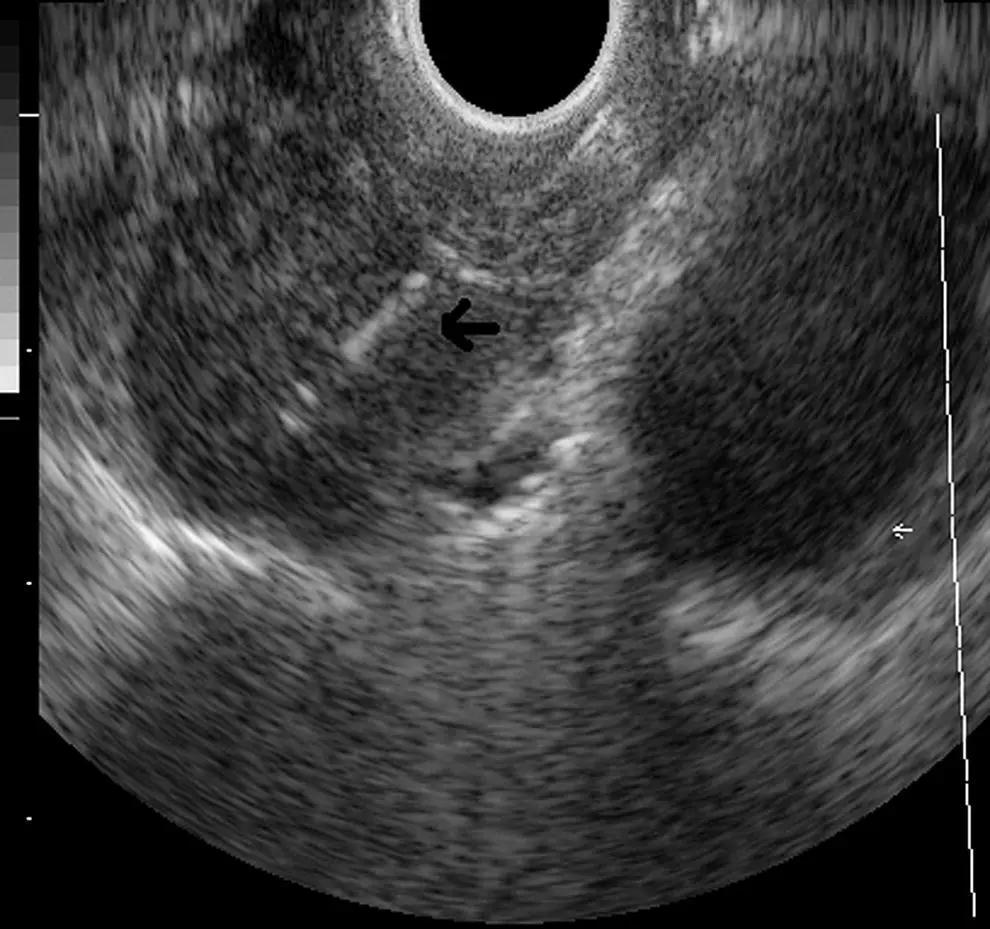
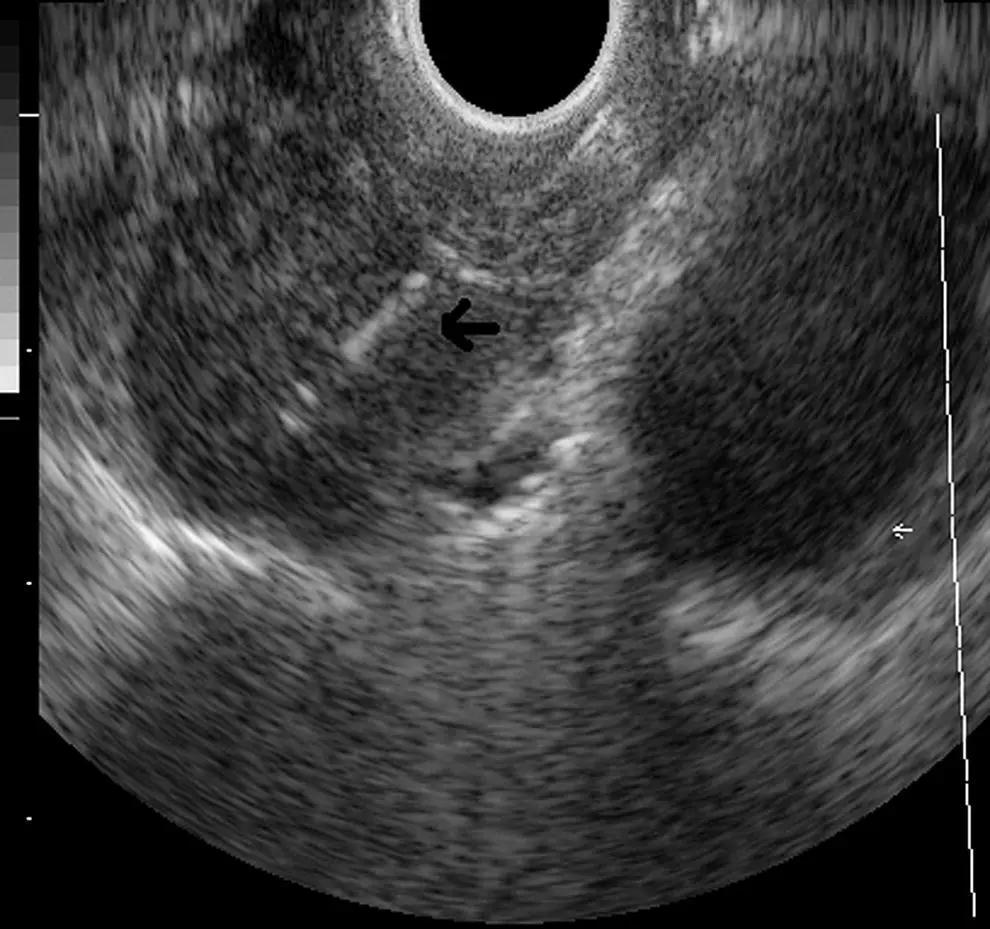
Figure 3.4 Subcarinal station (station 7).
At approximately 30 cm the subcarinal area is easily recognized by finding the left atrium, a large hypoechoic structure with cardiac motion, and pulling back until it disappears on the left edge of the screen. Then one should have the pulmonary artery in the right portion of the screen ( Figure 3.4). Slight movements to the right and left have to be performed to completely interrogate this station. This is the area of LN station 7 ( Videos 3.3and 3.4).
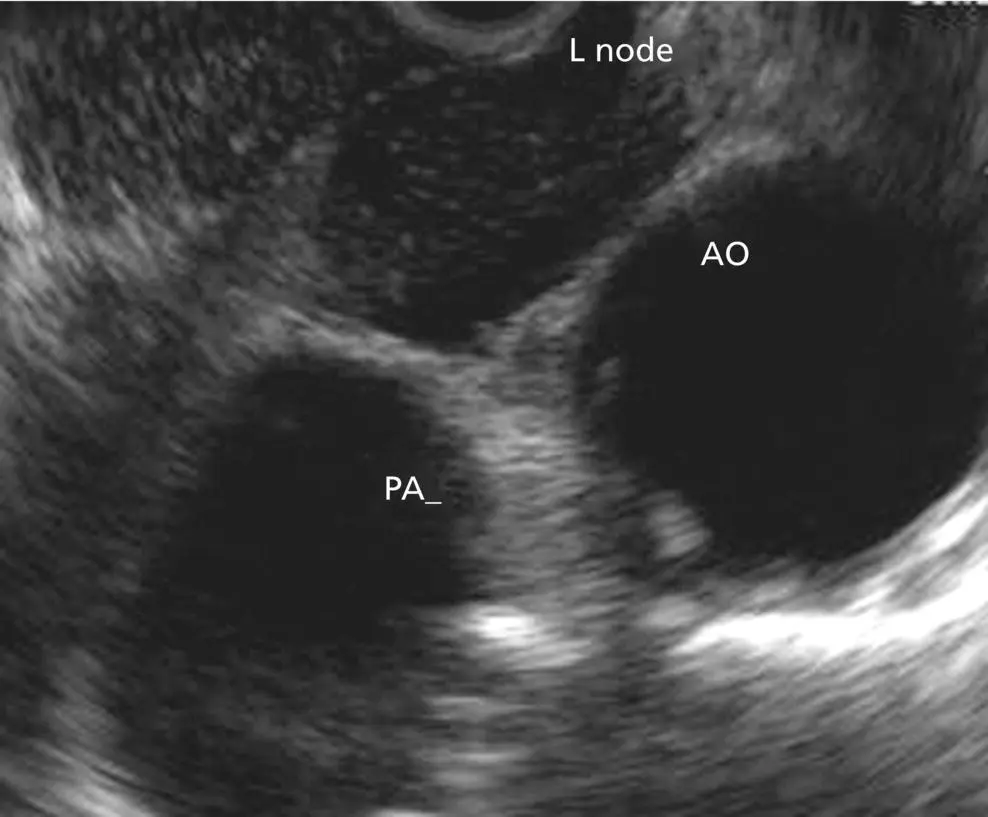
The azygos arch is located at 24–25 cm from the incisors. The aortopulmonary (AP) window (station 5) is situated between the aortic arch and the pulmonary artery. The AP window is found by following the aorta cephalad until its arch, rotating clockwise approximately 90 degrees, then advancing 1–2 cm with slight tip up of the echoendoscope. The aorta will be the echo‐poor structure on the right and the pulmonary artery will be to the left; the AP window is the space between the two just outside the AP ligament (which is not seen by EUS). The 4L region is immediately medial (close to the esophagus and EUS scope) to the AP window ( Figure 3.5). Alternatively, from the subcarinal area, rotating 90 degrees counterclockwise, crossing the left main bronchus and pulling it back 2–3 cm will put you in the same location. Further withdrawal of the echoendoscope with slight rotation will show the origin of the left subclavian artery. Occasionally, the left carotid artery can be seen above the brachiocephalic (innominate) vein.
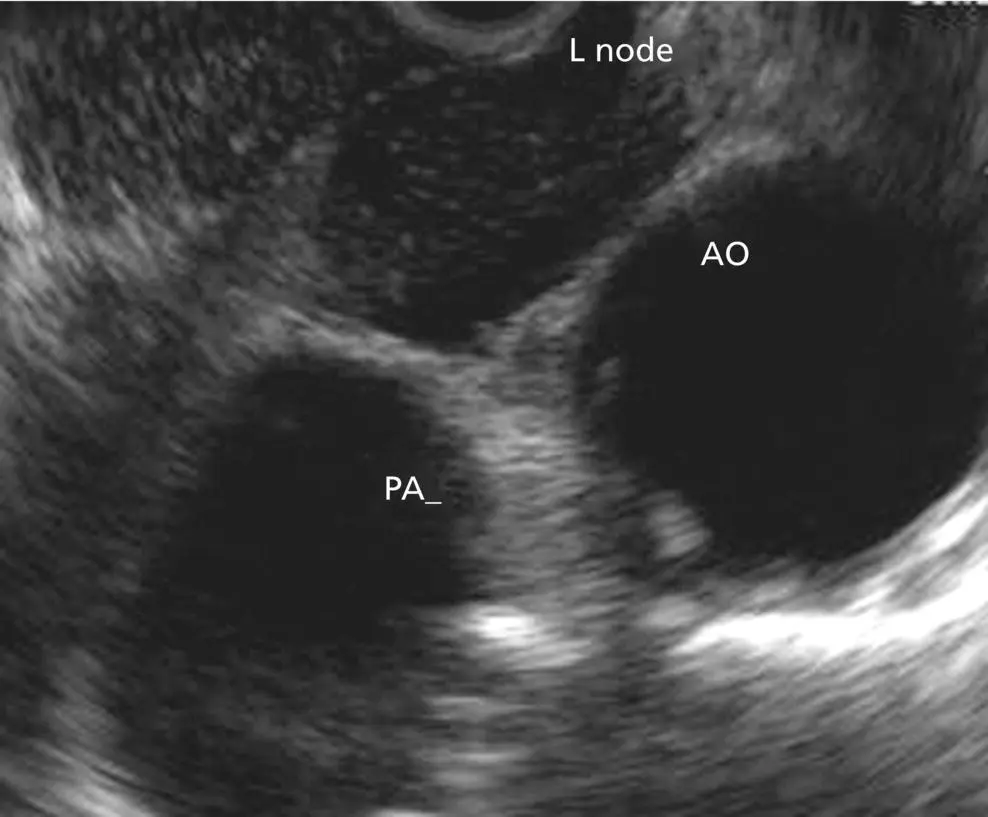
Figure 3.5 Aortopulmonary window station (stations 4L, 5 and 6). AO, aorta; L node; lymph node; PA, pulmonary artery.
Between 22 and 24 cm from the incisors, the superior part of the lungs can be imaged along with the trachea, cricoid bone, jugular veins, and carotid arteries.
At 17–20 cm from the incisors, the inferior thyroid gland can be imaged as well as cervical LNs, which can be targeted for FNA.
For radial scanning, one should enter the stomach, inflate the balloon, and pull back the scope until the GE junction. The aorta with be visualized as a large round echo‐poor structure. The aorta should be rotated to the 5 o’clock position, and the spine will be at 7 o’clock with the azygos vein in the middle. Then the balloon should be deflated and a slow pull‐back is performed observing all the mediastinal areas. It is important to note that, for a complete lung cancer staging with both radial and linear, the celiac axis, the left adrenal, and the left lobe of the liver should be surveyed. This is easily accomplished with a slight tip down on the echoendoscope and and then pushing it into the stomach; the celiac take‐off can be seen and the left adrenal can be seen at the 6 to 4 o’clock position with its usual “seagull” appearance. For the liver, one goes to the gastric antrum, aspirates all the air, inflating the balloon, and then tip up with a slow pull‐back.
Just like EUS, EBUS can be performed with conscious sedation, deep sedation, or general anesthesia. The tip of the scope is placed under direct visual contact in different positions, starting from the segmental bronchi to the trachea usually scanning 90–120 degrees every 0.5–1 cm. The diameter of the EBUS scope (6–7 mm) precludes passage beyond the second or third airway generation. EBUS‐TBNA is performed under the same principles as EUS‐FNA. As mentioned before, this technique is particularly useful for LN stations 2, 4, 7, 10, and 11 ( Figure 3.6). The upper and middle third of the esophagus can be visualized from the upper and lower trachea respectively Currently, we have different sizes of needle available, including 19, 21, 22, and 25 G.
EBUS anatomical landmarks
It is important to note that all right tracheal lymph node stations are found from the left lateral border of the trachea to the right aspect of the trachea.

Figure 3.6 Endobronchial ultrasound (EBUS) images of common mediastinal stations (4L, 7 and 11L). The esophagus and vertebral bodies can be visualized posteriorly from the upper and lower trachea.
Right upper paratracheal nodes (station 2R): the upper border is the apex of the right lung, the lower border is the intersection of the innominate vein with the trachea. This station is usually found facing the scope to the right lateral wall of the trachea, at 3 o’clock, at the level of the fifth tracheal cartilage.
Left upper paratracheal nodes (station 2L): the upper border is the apex of the left lung, the lower border is the superior limit of the aortic arch. This station is usually found facing the scope to the left lateral wall of the trachea, at 9 o’clock, at the level of the fifth tracheal cartilage.
Читать дальше