1 ...7 8 9 11 12 13 ...25 91.Jensen SS, Bornstein MM, Dard M, Bosshardt DD, Buser D. Comparative study of biphasic calcium phosphates with different HA/TCP ratios in mandibular bone defects. A long-term histomorphometric study in minipigs. J Biomed Mater Res B Appl Biomater 2009;90:171–181.
92.Miron RJ, Hedbom E, Saulacic N, et al. Osteogenic potential of autogenous bone grafts harvested with four different surgical techniques. J Dent Res 2011;90:1428–1433.
93.Miron RJ, Gruber R, Hedbom E, et al. Impact of bone harvesting techniques on cell viability and the release of growth factors of autografts. Clin Implant Dent Relat Res 2013;15:481–489.
94.Caballé-Serrano J, Bosshardt DD, Buser D, Gruber R. Proteomic analysis of porcine bone-conditioned medium. Int J Oral Maxillofac Implants 2014;29:1208–1215.
95.Asparuhova M, Caballé-Serrano J, Buser D, Chappuis V. Bone-conditioned medium contributes to initiation and progression of osteogenesis by exhibiting synergistic TGF-β1/BMP-2 activity. Int J Oral Sci 2018;10:20.
96.Caballé-Serrano J, Fujioka-Kobayashi M, Bosshardt DD, Gruber R, Buser D, Miron RJ. Pre-coating deproteinized bovine bone mineral (DBBM) with bone-conditioned medium (BCM) improves osteoblast migration, adhesion, and differentiation in vitro. Clin Oral Investig 2016;20:2507–2513.
97.Caballé-Serrano J, Sawada K, Miron RJ, Bosshardt DD, Buser D, Gruber R. Collagen barrier membranes adsorb growth factors liberated from autogenous bone chips. Clin Oral Implants Res 2017;28:236–241.
98.Allum SR, Tomlinson RA, Joshi R. The impact of loads on standard diameter, small diameter and mini implants: A comparative laboratory study. Clin Oral Implants Res 2008;19:553–559.
99.Kobayashi E, Matsumoto S, Doi H, Yoneyama T, Hamanaka H. Mechanical properties of the binary titanium-zirconium alloys and their potential for biomedical materials. J Biomed Mater Res 1995;29:943–950.
100.Al-Nawas B, Domagala P, Fragola G, et al. A prospective noninterventional study to evaluate survival and success of reduced diameter implants made from titanium-zirconium alloy. J Oral Implantol 2015;41:e118–e125.
101.Quirynen M, Al-Nawas B, Meijer HJA, et al; Roxolid Study Group. Small-diameter titanium grade IV and titanium-zirconium implants in edentulous mandibles: Three-year results from a double-blind, randomized controlled trial. Clin Oral Implants Res 2015;26:831–840.
102.Müller F, Al-Nawas B, Storelli S, et al; Roxolid Study Group. Small-diameter titanium grade IV and titanium-zirconium implants in edentulous mandibles: Five-year results from a double-blind, randomized controlled trial. BMC Oral Health 2015;15:123.
103.Schiegnitz E, Al-Nawas B. Narrow-diameter implants: A systematic review and meta-analysis. Clin Oral Implants Res 2018;29(suppl 16):21–40.
2
Bone Regeneration in Membrane-Protected Defects
Dieter D. Bosshardt, MSc, PhD | Simon S. Jensen, DDS, Dr odont | Daniel Buser, DDS, Dr med dent
A sufficient amount of living bone is required for both the esthetic outcome and the long-term success of dental implant therapy. In about 50% of implant sites, however, there is a need for a procedure that predictably generates enough bone volume for the placement of a dental implant. There are several options for the enhancement of bone formation, including (1) osteoinduction by autogenous bone grafts or the addition of growth factors; (2) osteoconduction provided by autogenous bone grafts or bone substitutes that serve as a scaffold for new bone formation; (3) transfer of stem cells or progenitor cells that differentiate into osteoblasts; (4) distraction osteogenesis; and (5) guided bone regeneration (GBR) using barrier membranes. Regardless of the method used, there is always an underlying basic biologic mechanism of bone healing.
Bone demonstrates a unique potential for regeneration, which is probably best illustrated by fracture repair. Bone is able to heal fractures or local defects with regenerated tissue of equally high structural organization, without leaving a scar. The mechanism of this healing pattern is often considered as a recapitulation of embryonic osteogenesis and growth. Because bone has a unique spontaneous healing capacity, the trick in reconstructive surgery is to harness this great regenerative potential to enhance bone formation for clinical applications. Thus, adequate bone augmentation or treatment of any bone defect requires a profound understanding of bone development and morphogenesis at the cellular and molecular levels. This chapter summarizes the development, structure, function, and regeneration of bone and discusses the pros and cons of the various biomaterials used for GBR to provide the biologic rationale for selecting appropriate biomaterial combinations for successful bone augmentation around dental implants in the long term.
Development and Structure of Bone
Functions
Bone certainly represents a great achievement in the evolution of supporting tissues. However, it has many additional functions. These include (1) mechanical body support, motion, and locomotion; (2) support of teeth for biting and crushing of food; (3) support and protection of the brain, spinal cord, and internal organs; (4) housing of bone marrow, which is the source of hematopoietic cells; and (5) calcium homeostasis. It is probably because these functions are of vital importance that bone possesses an exceptional capacity for self-healing, repair, and regeneration.
Bone types and structural organization
The mammalian skeleton consists of long bones and flat bones . Based on the orientation of the collagen fibrils, three types of bone tissue can be identified: woven bone, lamellar bone, and an intermediate type—the primary parallel-fibered bone.
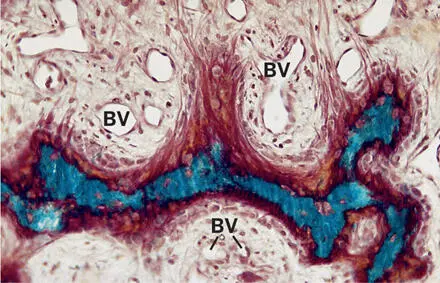
Woven bone is formed predominantly in embryos and growing children and is replaced later by lamellar bone. In adults, woven bone reappears when accelerated bone formation is required, as in the bony callus during fracture repair and in pathologic conditions like Paget disease of bone, renal osteodystrophy, hyperparathyroidism, or fluorosis. In woven bone, the collagen fibrils are oriented in a random manner, and the interfibrillar spaces are comparatively wide. 1 Besides having intertwined collagen fibrils, woven bone is characterized by a high number of large osteocytes and a high mineral density (Fig 2-1).
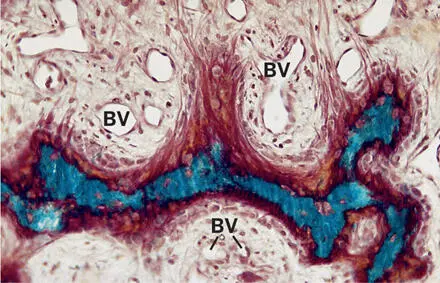
Fig 2-1Light microscopic view of woven bone. This type of bone forms struts and ridges, which are always closely associated with blood vessels (BV) (Goldner trichrome stain).
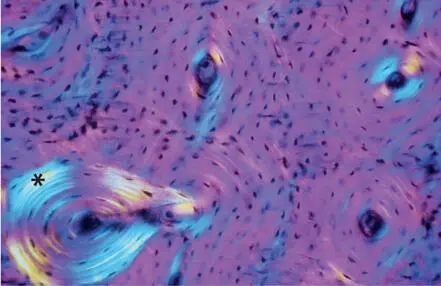
Lamellar bone possesses a much more complex structure, characterized by matrix layers that consist of a parallel collagen fibril arrangement. One lamellar unit is about 3 to 5 µm wide, and the orientation of the fibrils changes from one lamella to another (Fig 2-2). Thus, lamellar bone may be regarded as a complex, plywood-like structure. 2
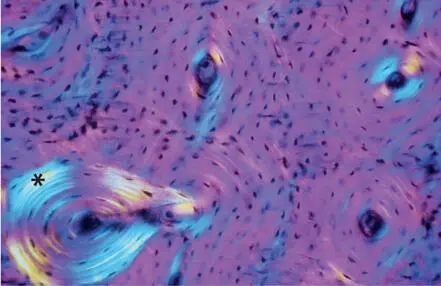
Fig 2-2Primary and secondary osteons in equine cortical bone. In polarized light, secondary osteons (asterisk) reveal a clear lamellar pattern. The wall of primary osteons consists of primary parallel-fibered bone, which is less birefringent.
Primary parallel-fibered bone is deposited in the early stages of bone formation, as well as during periosteal and endosteal bone apposition. Its collagen fibrils run parallel to the bone surface but lack lamellar organization (Fig 2-3). Primary parallel-fibered bone shares most physiologic properties with woven bone.
Читать дальше