In the immediate context of the treatment of impacted teeth, however, this procedure offers advantages for problems that are difficult to overcome by other means, and nowhere is its efficacy easier to demonstrate than in relation to the resolution of an impacted second mandibular molar. If an attempt is made to elevate an impacted mandibular molar, particular one with a distinct mesial inclination beneath the distal bulbosity of the first molar, a great deal of anchorage potential may be expended in its alignment. To use the remaining teeth as the base from which the extrusive force is to be applied will rapidly cause marked intrusion of these teeth and a strong cant in the occlusal plane. In time, this may then secondarily cause an asymmetrical deterioration in the maxillary occlusal plane.
Had the opposing teeth been used as the anchorage base, rapid extrusion of these teeth and a cant in the upper occlusal plane would be generated. Furthermore, the maxillary second molar may already have over‐erupted a priori , in the absence of the unerupted mandibular second molar, and may even be impinging on the soft tissue overlying this impacted tooth. Clearly, therefore, intra‐arch or inter‐arch tooth‐borne mechanics are completely inappropriate unless backed up by some form of skeletal anchorage.
The over‐eruption of an unopposed maxillary second molar is usually recognized by its vertically prominent mesial marginal ridge in relation to the occlusal plane, as represented by the distal marginal ridge of the first molar. This needs to be corrected concurrently with orthodontic eruption of an impacted mandibular molar, to bring it into occlusion at the level of the occlusal plane. To this end, an elastic chain may be drawn across the occlusal surface of the over‐erupted maxillary molar from a palatal screw TAD to the intra‐oral extremity of the zygomatic plate implant.
At the same time, a vertical intermaxillary elastic may be placed by the patient from the same intra‐oral extremity of the zygomatic plate, to an attachment on the impacted tooth in the mandible. In this manner, it is easy to balance the degree of extrusion of the one with the degree of intrusion of the other, in relation to the occlusal plane. For these movements to be completed, no brackets or other appliances need to be placed on any of the other teeth. Furthermore, no retainer appliances need to be placed at the end of this phase of the treatment.
It will be appreciated that the zygomatic plate is an important device that may be used as a support to move a tooth mesially or distally and to extrude or to intrude a tooth. It may also be employed as an anchor base to safeguard against movement of a block of teeth and to move a large number of teeth at one and the same time. It may be used for intermaxillary up‐and‐down stability in the correction of vertical discrepancies and, antero‐posteriorly, for class II or class III correction.
Ankylotic, infra‐occluded, implanted or otherwise non‐movable teeth as bone anchors
There are several situations where an erupted or partially erupted deciduous or permanent tooth cannot be moved. Ankylosis is usually the term given to these teeth, although infra‐occlusion of deciduous or permanent teeth may not necessarily be due to ankylosis. Successfully replanted teeth that have been avulsed as the result of trauma are usually ankylotic. These teeth may often be included in an orthodontic appliance to act as bone anchors, in much the same way as described above regarding the zygomatic plates and screw TADs. Accordingly, they may be used as the base against which orthodontic forces may be applied to other teeth.
One possible source for the application of suitable forces is the rare earth magnet. These magnets were developed more than 60 years ago, and it has more recently become possible to reduce them in size with the introduction of lanthanide alloys, so that now they may be exploited in the present context. The professional literature has presented successful clinical results of the treatment of impacted teeth in humans [23–26] using magnetic forces. The ‘pull’ of the rare earth magnet is generated along the line of the magnetic plane and in consequence it is possible to prescribe tooth movement in all three planes [27, 28]. However, these magnets corrode significantly in the intra‐oral environment and have to be carefully coated in order to render them safe. A parylene coating has been shown to seal them successfully and, when embedded in acrylic appliances, these magnets can be isolated from the intra‐oral environment and protected from heavy biting forces [28].
There are a number of other significant problems with the use of the rare magnet. The attracting forces that exist between the two magnets are in inverse proportion to the square of the distance between them. This means that when employed in order to move displaced or ectopically positioned teeth, the magnet that is sited on the appliance must be placed close to the magnet that has been bonded to the displaced tooth, otherwise the force between them will be too low. Furthermore, if the magnets are not ideally sited one on top of the other, there will be a dramatic drop in force level [28, 29].
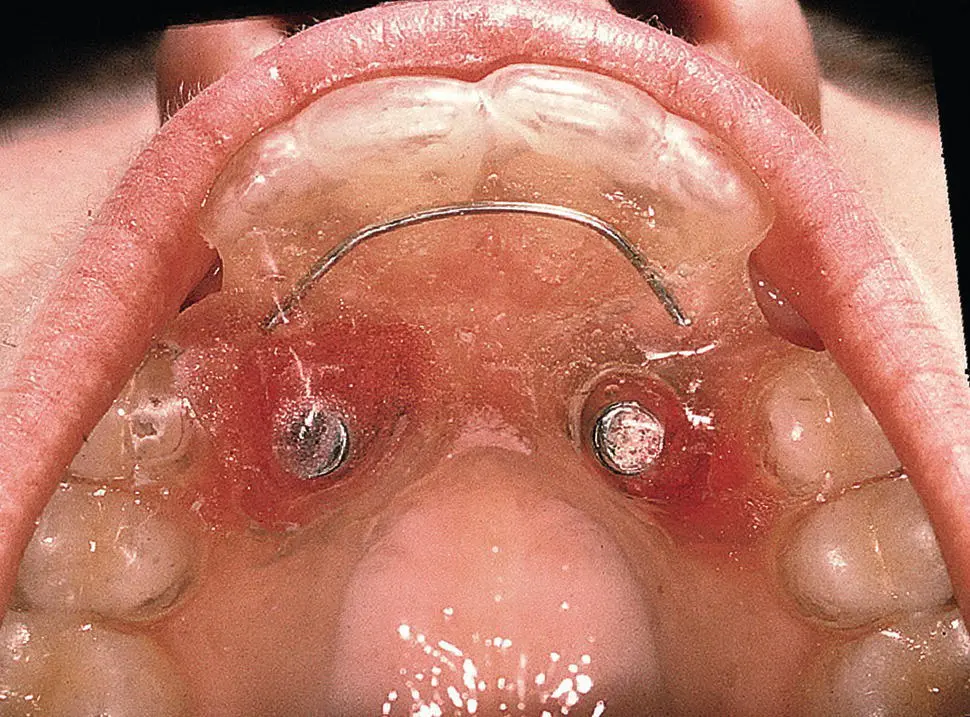
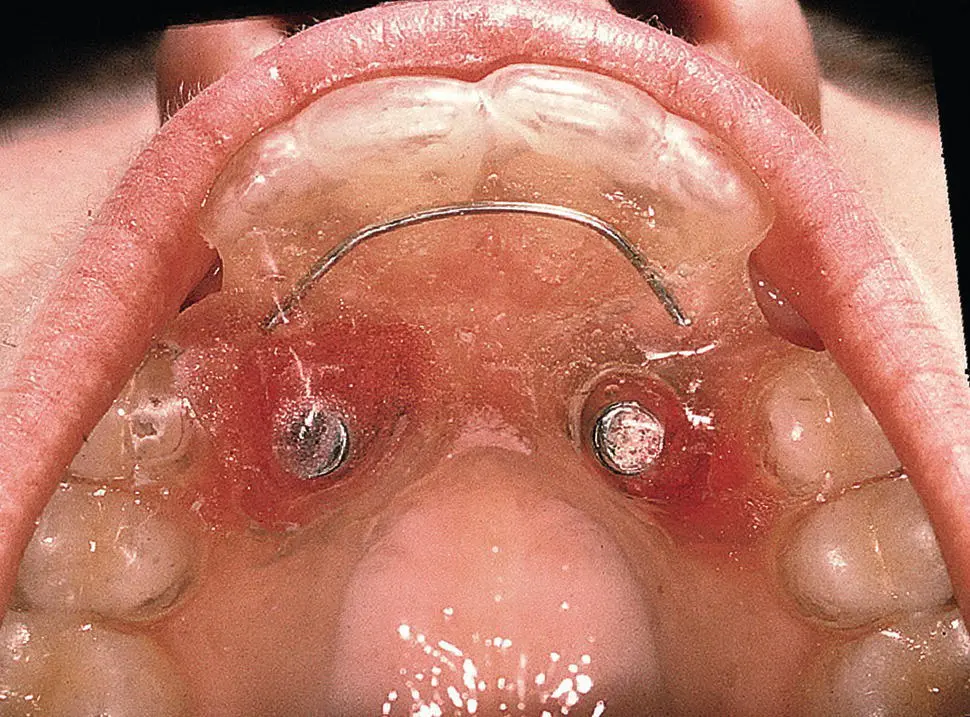
Fig. 2.10 The bonded magnet ‘backpack’.
Courtesy of Professor A. D. Vardimon.
The notion that traction may be applied without the need to trail a wire or a chain through the soft tissues of the palate has a definite appeal to professional authors. They speculate that this will improve the ultimate periodontal condition of the teeth, since ‘eruption simulates a normal eruption process’. However, the following points should be remembered:
The tooth must in any event initially be surgically exposed.
The magnet must be bonded to it.
An open exposure will be indicated for a very superficial and mildly displaced tooth.
For a deeper and markedly displaced tooth, the flap must be partially or fully replaced and healing must occur.
The tooth must then travel through the tissues with this relatively large magnetic ‘backpack’ ( Figure 2.10).
Each of these caveats will present an obstacle that signifies a departure from the similarity to a tooth that has erupted normally. Even if the idea is ‘attractive’ [30], the use of magnets for impacted teeth is still in its early developmental stages and seems to have been largely lying dormant since the mid‐1990s. The methods that have been described still demonstrate a number of technological disadvantages, the size of the magnets and the inverse square rule of their force of attraction being the most pertinent. At the present time, this method cannot yet be seen as an unequivocal substitute for the more traditional and conventional methods described above [31–34] and has largely been sidelined.
1 1. Olive RJ. Factors influencing the non‐surgical eruption of palatally impacted canines. Aust Orthod J 2005; 21: 95–101.
2 2. Höchli D, Hersberger‐Zurfluh M, Papageorgiou SN, Eliades T. Interventions for orthodontically induced white spot lesions: a systematic review and meta‐analysis. Eur J Orthod. 2017; 39: 122–133.
3 3. Iramaneerat S, Cunningham SJ, Horrocks EN. The effect of two alternative methods of canine exposure upon subsequent duration of orthodontic treatment. Int J Paediatr Dent 1998; 8: 123–129.
4 4. Becker A. Alternative methods of canine exposure and subsequent duration of treatment. Int J Paediatr Dent 1998; 8: 298–299 [letter to the editor].
Читать дальше