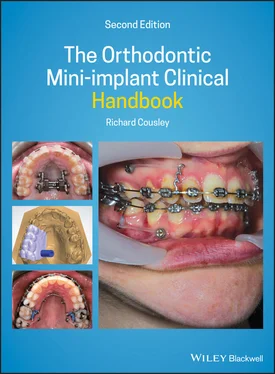
1 Cover
2 Preface to Second Edition
3 1 Orthodontic Mini‐implant Principles and Potential Complications 1.1 The Origins of Orthodontic Bone Anchorage 1.2 The Evolution of Mini‐implant Biomechanics 1.3 3D Anchorage Indications 1.4 Using the Right Terminology 1.5 Principal Design Features 1.6 Clinical Indications for Mini‐implants 1.7 Benefits and Potential Mini‐implant Complications 1.8 Mini‐implant Success and Failure 1.9 Medical Contraindications 1.10 Root/Periodontal Damage 1.11 Perforation of Nasal and Maxillary Sinus Floors 1.12 Damage to Neurovascular Tissues 1.13 Mini‐implant Fracture 1.14 Pain 1.15 Soft Tissue Problems 1.16 Mini‐implant Migration 1.17 Biomechanical Side‐effects 1.18 Factors Affecting Mini‐implant Success References
4 2 Maximising Mini‐implant Success: Patient (Anatomical) Factors 2.1 Cortical Bone Thickness and Density 2.2 Interproximal Space 2.3 Soft Tissue and Oral Hygiene 2.4 Maxillomandibular Planes Angle 2.5 Age 2.6 Cigarette Smoking 2.7 Body Mass Index References
5 3 Maximising Mini‐implant Success: Design Factors3.1 Mini‐implant Design Factors 3.2 The Infinitas™ Mini‐implant System 3.3 Digital Stent Fabrication Processes References
6 4 Maximising Mini‐implant Success: Clinical Factors4.1 Clinical Technique Factors 4.2 Introducing Mini‐implants to your Clinical Practice 4.3 Patient Consent 4.4 Key Points to Consider for Valid Consent 4.5 Staff Training 4.6 Patient Selection References
7 5 Mini‐implant Planning 5.1 Mini‐implant Planning 5.2 Mini‐implant Location 5.3 Hard Tissue Anatomy and Radiographic Imaging 5.4 Soft Tissue Anatomy 5.5 Vertical Location and Inclination 5.6 Insertion Timing 5.7 Guidance Stent 5.8 Mini‐Implant Dimensions References
8 6 Mini‐implant Insertion 6.1 Mini‐implant Kit Sterilisation 6.2 Superficial Anaesthesia 6.3 Antibacterial Mouthwash 6.4 Stent Application (Optional) 6.5 Soft Tissue Removal 6.6 Cortical Perforation 6.7 Mini‐implant Insertion 6.8 Mini‐implant Fracture 6.9 Postoperative Instructions 6.10 Force Application 6.11 Biomechanics 6.12 Explantation 6.13 Summary of Mini‐implant Insertion Steps 6.14 Maximising Mini‐implant Success: Ten Clinical Tips References
9 7 Retraction of Anterior Teeth 7.1 Clinical Objective 7.2 Treatment Options 7.3 Key Treatment Planning Considerations 7.4 Biomechanical Principles 7.5 Midtreatment Problems and Solutions 7.6 Clinical Steps for a Posterior Mini‐implant 7.7 Biomechanical Options for Anterior Teeth Retraction 7.8 Case Examples References
10 8 Molar Distalisation8.1 Alternatives to Mini‐Implant Distalisation 8.2 Clinical Objectives of Molar Distalisation 8.3 Treatment Options 8.4 Key Treatment Planning Considerations 8.5 Biomechanical Principles 8.6 Midtreatment Problems and Solutions 8.7 Mandibular Arch Distalisation 8.8 Maxillary Arch Distalisation 8.9 Midpalatal Distaliser Options References
11 9 Molar Protraction 9.1 Clinical Objective 9.2 Treatment Options 9.3 Key Treatment Planning Considerations 9.4 Biomechanical Principles 9.5 Midtreatment Problems and Solutions 9.6 Clinical Steps for Molar Protraction Using Alveolar Site Anchorage 9.7 Case Examples 9.8 Clinical Steps for Midpalate (Indirect) Anchorage (Figure 9.3) 9.9 Direct Palatal Anchorage Example (Figure 9.15) References
12 10 Intrusion and Anterior Openbite Treatments 10.1 Single‐Tooth and Anterior Segment Intrusion Treatments 10.2 Anterior Openbite Treatment References
13 11 Transverse and Asymmetry Corrections11.1 Asymmetry Problems 11.2 Dental Centreline Correction 11.3 Unilateral Intrusion (Vertical Asymmetry Correction)
14 12 Ectopic Teeth Anchorage 12.1 Clinical Objectives 12.2 Treatment Options 12.3 Relevant Clinical Details 12.4 Biomechanical Principles 12.5 Clinical Tips and Technicalities 12.6 Midtreatment Problems and Solutions 12.7 Clinical Steps for Ectopic Tooth Alignment
15 13 Bone‐anchored Maxillary Expansion13.1 Conventional Rapid Maxillary Expansion 13.2 Expansion Forces and Speed 13.3 Potential Advantages of Mini‐implant Anchored RME 13.4 Clinical Objective 13.5 Treatment Options 13.6 Relevant Clinical Details 13.7 Design Options for Mini‐implant Expanders 13.8 Hybrid RME 13.9 Non‐tooth Borne Mini‐Implant Only RME 13.10 Biomechanical Principles 13.11 Haas‐type (Mucosa) and Mini‐implant RME 13.12 Summary of RME Design Selection References
16 14 Orthognathic Surgical Uses 14.1 Clinical Objectives 14.2 Treatment Options 14.3 Relevant Clinical Details 14.4 Biomechanical Principles 14.5 Clinical Tips and Technicalities 14.6 Clinical Steps 14.7 Case Examples References
17 Index
18 End User License Agreement
1 Chapter 1 Table 1.1 The clinical evolution of orthodontic mini‐implant anchorage is sub...
2 Chapter 3 Table 3.1 The Infinitas mini‐implant range and typical insertion sites
3 Chapter 4Table 4.1 A clinical database for mini‐implant audit purposes
4 Chapter 5Table 5.1 Clinical scenarios where additional details dictate that a wide dia...
5 Chapter 10Table 10.1 Ten tips for clinical success in molar intrusion
6 Chapter 13Table 13.1 Mini‐implant (OMI) anchored expander design options with practical...
7 Chapter 14Table 14.1 Different time points (stages) of the orthognathic treatment pathw...
1 Chapter 1 Figure 1.1 The three principal sections of a mini‐implant: the head superfic... Figure 1.2 (a) Direct anchorage where this grey elastomeric attachment provi... Figure 1.3 Coronal slice views of a CBCT scan of the maxilla (a) before and ... Figure 1.4 Intraoral radiographs taken after (a) insertion of a cylindricall... Figure 1.5 Overgrowth of the labial sulcular tissues caused by these mandibu... Figure 1.6 (a) Photograph of lower anterior mini‐implants immediately after ... Figure 1.7 (a) Hyperplasia of the palatal mucosa covering an overinserted mi... Figure 1.8 Labial ulceration caused by this mandibular mini‐implant's insert... Figure 1.9 (a) Elastomeric traction auxiliary in contact with the alveolar m... Figure 1.10 Diagrams showing the vertical side‐effects of an oblique vector ...
2 Chapter 2 Figure 2.1 An axial cone beam CT where the cortical bone is seen as the peri... Figure 2.2 A panoramic radiograph which illustrates the typical variations i... Figure 2.3 Photographs showing typical peri‐implant soft tissue inflammation... Figure 2.4 Lateral cephalograms of mini‐implant anchorage patients exhibitin...
3 Chapter 3 Figure 3.1 Diagram of the Infinitas mini‐implant head showing its four brack... Figure 3.2 Diagram of an obliquely inserted Infinitas mini‐implant with a co... Figure 3.3 Diagram of an obliquely inserted mini‐implant where the body trav... Figure 3.4 Packaging of presterilised Infinitas mini‐implants. The mini‐impl... Figure 3.5 Diagram showing how the body's coronal section tapers out from a ... Figure 3.6 Diagram of the Infinitas cortical bone punch traversing the mucos... Figure 3.7 Handpiece insertion of an Infinitas mini‐implant on the palatal a... Figure 3.8 Drilling of the palatal aspect of a plaster model, with the drill... Figure 3.9 (a) Infinitas analogues have been inserted into predrilled holes ... Figure 3.10 A finished insertion stent where the insertion hole in the plast... Figure 3.11 Diagram of a ( green ) computer‐generated guidance stent, with twi... Figure 3.12 (a,b) Illustrations of a unilateral palatal stent designed using... Figure 3.13 (a–c) Diagrams of a CBCT software package being used to plan pla...
4 Chapter 4Figure 4.1 Periapical radiographs taken (a,b) before and (c,d) after inserti...Figure 4.2 The two sides of a mini‐implant patient information leaflet, whic...
5 Chapter 5Figure 5.1 Flowchart highlighting the most common insertion site planning co...Figure 5.2 (a) Panoramic and (b) intraoral pretreatment radiographs of the d...Figure 5.3 (a) A reformatted CBCT image of the right maxilla taken to assess...Figure 5.4 A reformatted CBCT image of the maxilla in a 19‐year‐old female, ...Figure 5.5 Reformatted CBCT image of the maxilla in (a) adolescent and (b) a...Figure 5.6 The upper and lower mucogingival junctions are highlighted as bla...Figure 5.7 Two different versions of powerarms being used in the upper arch ...Figure 5.8 (a) Pretreatment panoramic and (b) intraoral postinsertion radiog...Figure 5.9 (a) Intraoral radiograph of an adult where early loss of a first ...Figure 5.10 The clear elastomeric attachment provides horizontally orientate...Figure 5.11 Diagrams of (a) oblique and (b) horizontal vectors of traction t...Figure 5.12 (a) Pretreatment panoramic, (b) preinsertion and (c) postinserti...Figure 5.13 Diagrams of the premolar and first molar teeth where (a) the sec...Figure 5.14 Algorithms (flowcharts) highlighting the most common considerati...Figure 5.15 Lateral cephalogram showing the midline palatal bone thickness a...
Читать дальше