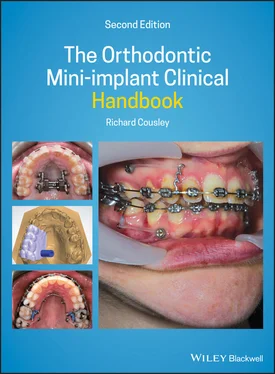
Greater predictability of both the treatment mechanics and clinical outcomes. For example, one can now confidently retract the labial segment without anchorage or torque loss in a controlled manner (as described in Chapter 7).
Reduced treatment time, especially where it's more efficient to move groups of teeth rather than subdivide movements in an attempt to spare anchorage demands. This is exemplified by en masse retraction of the canine and incisor teeth in a single phase, rather than two‐phase retraction of the canines then incisors. A randomised trial showed a four‐month time saving in this respect [15].
3D anchorage control. Traditionally, orthodontists think of anchorage reinforcement in the anteroposterior dimension, with much less emphasis on vertical and transverse anchorage. However, now that it's feasible to control anchorage in all three dimensions, orthodontics can truly aim to correct 3D malocclusion traits.
However, a number of risks and side‐effects have been observed over the years with mini‐implant clinical usage and in the research literature. Fortunately, these are reversible in most clinical situations, but it is important to consider them in an effort to maximise mini‐implant treatment success and to provide informed patient consent. The main risks are described in the following sections.
1.8 Mini‐implant Success and Failure
Failure of a mini‐implant is the ‘risk’ that one ought to focus on most in day‐to‐day clinical terms. Mini‐implant failure means that it cannot be used for its intended clinical loading/anchorage purposes. Conversely, mini‐implant success is generally defined as the fixture remaining stable under continuous orthodontic loading for a minimum period of six months, although many studies have used one year as the minimum observation time. One of the most recent overviews of success rates has been provided by a meta‐analysis of 3250 mini‐implants, which showed a combined rate of 86% [16]. When the effect of insertion site is analysed, there is a consensus in the literature that the success rate varies according to the jaw involved, at approximately 80% and 90% for alveolar sites in the mandible and maxilla respectively, and up to 99% in the midpalate [17–30]. Conversely, success rates for infrazygomatic sites are relatively low, at 78%, as reported in a study of 30 consecutive Caucasian patients [31]. This may seem counterintuitive since the mandible is generally regarded as the stronger jaw bone, but the reasons for this paradox will be explained in Chapter 2.
Interestingly, mini‐implants with minor mobility may still be graded as successful. This is evident clinically by slight rotational or lateral movement of the mini‐implant on manipulation. This is painless and consequently asymptomatic for the patient. It is easily resolved by tightening the mini‐implant, usually by a clockwise turn (insertional rotation), provided that this does not submerge the head, and without the need for anaesthesia. Notably, for Infinitas mini‐implants, one complete turn equates to 0.7 mm further insertion. However, if the mini‐implant displays obvious lateral mobility with light digital pressure then this indicates failure and the mini‐implant should be removed.
Fortunately, most mini‐implant failures become clinically evident within the first few months of insertion [20,24,25], enabling early replacement or a modification to the treatment plan. However, it important to realise that replacement mini‐implants still have much lower success rates than primary insertions [32,33]. For example, a recent study of 471 mini‐implants showed primary and secondary (replacement) success rates of 85% and 58% for maxillary buccal sites and 79% and 77% respectively for midpalate sites [33]. This marked drop in success rates for buccal, but not palatal, insertion sites suggests that the midpalate ought to be considered if a maxillary buccal mini‐implant fails unless there has been an obvious and rectifiable explanation for the failure. Therefore, it is important to determine the likely reason for failure and undertake remedial clinical steps, such as root divergence, to favourably alter the chances of success for a secondary buccal site insertion. On the plus side, when a mini‐implant feels firm after two months in situ then normal orthodontic forces may be applied with confidence.
Mini‐implant failures are staged according to the time taken for this to manifest after insertion.
Primary failure occurs when a mini‐implant is clinically mobile at the time of insertion. This is due to inadequate cortical bone support in terms of its thickness and density, or close mini‐implant proximity to an adjacent tooth root or incorrect insertion technique. These factors will be fully discussed in the relevant sections.
Secondary failure refers to a situation where the mini‐implant is initially stable but then exhibits mobility, usually after 1–2 months. This delayed instability is due to bone necrosis around the mini‐implant threads, which may result from thermal bone damage (during pilot drilling), excessive insertion torque, excessively close proximity to a tooth root, traction overload, or a combination of these.
Most mini‐implant failures become clinically evident within the first few months of insertion, enabling early replacement.
1.9 Medical Contraindications
There are no absolute medical contraindications which specifically apply to orthodontic mini‐implants. Conditions, such as diabetes mellitus and immunosuppression, which are relative contraindications to orthodontic treatment in general must be considered in terms of soft tissue hyperplasia and infection risks. However, if the patient has good oral hygiene then comprehensive treatment may proceed as normal. Older, especially female, patients with osteoporosis may present problems in terms of reduced bone support and hence mini‐implant stability, but this can be accounted for in terms of insertion site and force application considerations. The increasing number of older patients on bisphosphonate drug treatment are a specific group which may limit orthodontic treatment, especially against tooth extractions (because of osteonecrosis risks). Whilst I have successfully treated patients taking oral bisphosphonates with routine orthodontic treatment (e.g. alignment), I have no experience of using mini‐implants in this group of patients and am unaware of any literature published on this.
1.10 Root/Periodontal Damage
Multiple clinical and animal studies have been conducted with the aim of intentionally inflicting damage on tooth roots, using both pilot drills and self‐drilling mini‐implants [34–42]. Fortunately, these studies have consistently shown that traumatised root surfaces are repaired within 12 weeks by cellular cementum and periodontal regeneration, provided that there is no infection portal present (which is usually the case). The cementum repair even occurred when root dentine was fully exposed [34]. Orthodontists can also be reassured that there are no known reports of tooth ankylosis or loss arising from mini‐implant use. This may be because, in normal clinical usage, if a self‐drilling mini‐implant contacts a root then the insertion stalls and its tip will become blunt, preventing extensive penetration of the root tissues. Furthermore, the patient is likely to complain of pain (from periodontal pain receptors) even before root contact occurs. If the root is actually contacted then the orthodontist is also likely to feel a sharp increase in insertion torque [43].
So if a mini‐implant doesn't actually contact a root surface, is there still scope for indirect damage? A recent finite element analysis study indicated that less than 1 mm of separation of the mini‐implant and the adjacent root surface may still risk root resorption because a transfer of stress through the thin layer of bone causes an osteoclastic reaction beside the root surface [44]. However, this has not been validated by animal or clinical studies, and the reciprocal effect on bone remodelling around the mini‐implant is more likely to have a negative impact. For example, a histological analysis of mini‐implants inserted in a dog model showed a significant reduction in BIC where the implant body contacted the root or even just the bundle bone (around the periodontal ligament) [45]. Therefore, it is reasonable to conclude that any irreversible effect from close proximity of a mini‐implant and a tooth root will be on the mini‐implant: it will have an increased risk of failure (by becoming mobile) rather than the tooth being irreversibly damaged [43,46–50].
Читать дальше