Age is an important factor in a patient's response to anesthesia. Sensitivity to anesthetic drugs and alterations in the dosages required to achieve specified levels of sedation are seen with extremes of age. While this may seem self‐evident in the elderly, research shows that the reduction in required anesthetic dose begins as early as age 40–45 [17]. For each decade past the age of 40, there is an observed 10% reduction in the dose of fentanyl required, while for propofol the dose reduction is about 8% [17]. The pediatric population in particular has a markedly idiopathic response to anesthetic drugs, and titration of sedation can be more challenging in this age group. Ironically, patients with very high anxiety levels may be prone to oversedation because they typically require a high initial dose of anesthetic to achieve sedation, but often markedly less medication to maintain a given level of anesthesia. Failure to reduce the dosage of anesthesia adequately after the initial induction bolus in these patients can result in oversedation.
Oversedation may be caused when boluses of a drug are given too quickly or too close together. This typically occurs during an anesthetic procedure when a patient begins to awaken or becomes agitated and additional medications are administered to rapidly deepen the anesthesia. Since all anesthetic drugs take some period of time to exert their effect, failure to wait for the drug to take effect can result in the observation that the dose was insufficient and the administration of an additional bolus. Subsequently, when the additional boluses have had time to take effect, the patient may be in a deeper plane of anesthesia than was intended. This can be partially prevented by the spacing of additional drug boluses and knowing the time to effective onset of the anesthetic drugs utilized. Not all pharmacological agents demonstrate first‐order kinetics, however, and rate of drug onset can be increased or decreased depending on the patient's plasma drug level.
Oversedation can sometimes result when the level of surgical stimulation is rapidly or dramatically decreased. Since surgical stimulation tends to counteract the sedative effects of anesthetic drugs, a higher dose of anesthesia is typically required for more stimulating surgical procedures. A patient who is at an appropriate level of anesthesia may quickly become oversedated if stimulation is decreased or discontinued. In situations where changes in the level of surgical stimulation can be predicted, allowing time for the anesthetic drug to wear off or decreasing the rate of infusion can effectively prevent most oversedation in these cases.
Management of mild oversedation may consist of briefly interrupting the administration of anesthetic drugs and observing the patient for a return to the desired level of anesthesia. If any degree of respiratory obstruction or depression is noted, maneuvers aimed at opening the airway such as a chin lift or jaw thrust should be performed as well. Given the rapid redistribution and short duration of effect of many anesthetic drugs, mild oversedation is self‐correcting with supportive measures within a matter of a few minutes.
Although not a mainstay of treatment, administration of reversal agents may be considered as an adjunctive therapy for oversedation. Few drugs used in ambulatory anesthesia have a reversal agent, but naloxone is able to reverse the effects of opioid agonist drugs and flumazenil is an effective antagonist of the benzodiazepine class of drugs. These reversal agents can be effective in reversing the effects of oversedation due to drug overdosage, but they reverse all actions of a drug including desirable effects such as analgesia, hypnosis, and anxiolysis. They may be considered for the treatment of oversedation and prolonged awakening in the postoperative period and are generally well tolerated. Research has not supported the routine use of reversal agents to speed recovery from ambulatory anesthesia procedures.
Seizure activity, both partial type and tonic–clonic seizures, represents abnormal CNS excitation. Because anesthetic drugs act by causing depression of the CNS, seizure activity during an anesthetic procedure is unlikely to occur. In patients with seizure disorders, however, seizures may occur in the preoperative and postoperative periods. Management of seizures involves positioning the patient to avoid injury and loosening tight or restrictive clothing as much as possible. Most seizures will terminate after a few minutes and require no other treatment, though benzodiazepines such as midazolam, lorazepam, or diazepam may be given intravenously or intramuscularly to terminate seizure activity. Since patients will typically become hypoxic during the clonic phase of a tonic–clonic seizure, supplemental oxygen may be beneficial in the immediate postictal period.
CARDIOPULMONARY COMPLICATIONS
Respiratory Depression and Respiratory Arrest
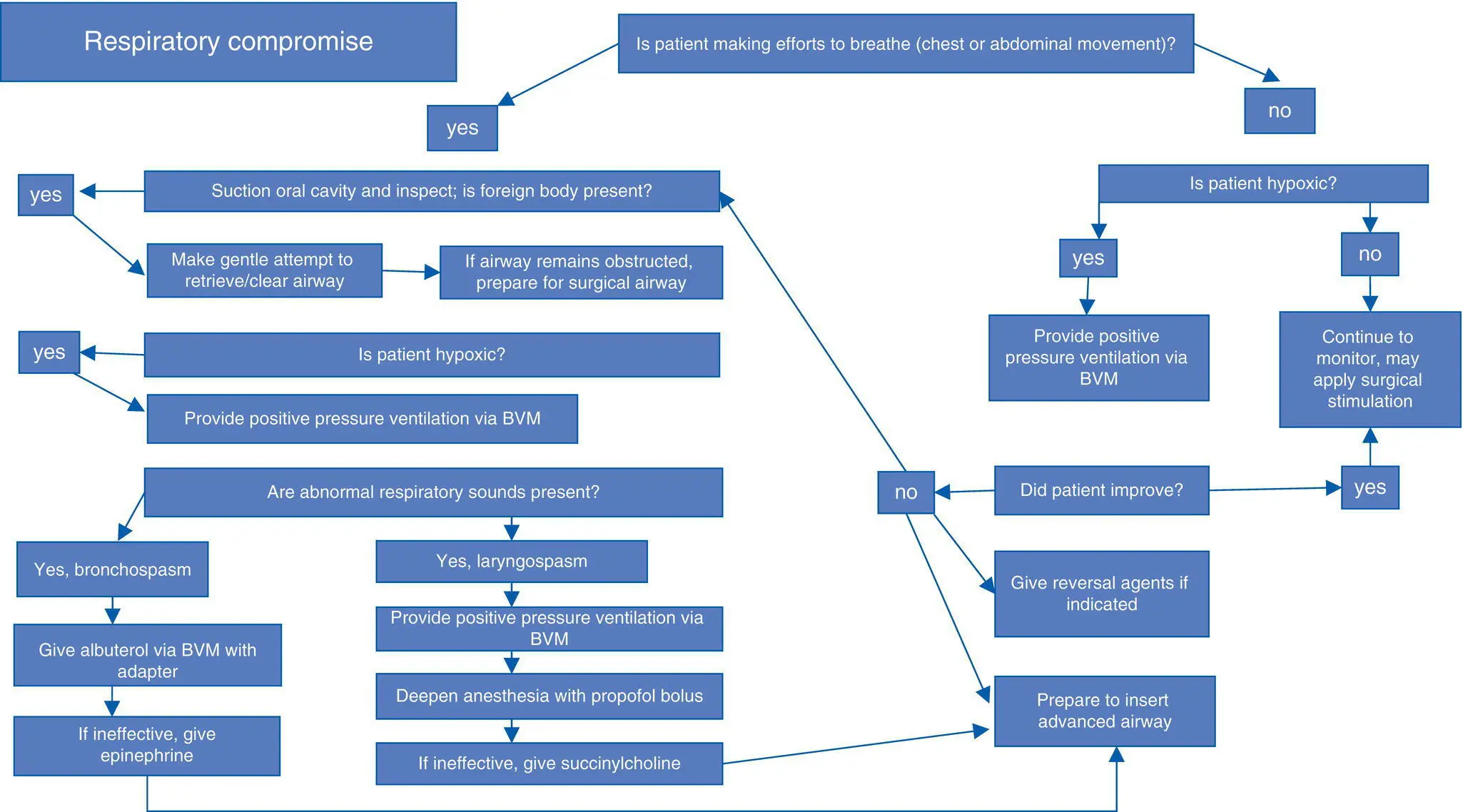
The effects of anesthetic drugs are the most common cause of respiratory depression in ambulatory anesthesia ( Algorithm 1.3). An overdose of anesthesia will produce respiratory depression in virtually all cases, and this may progress to full respiratory arrest if not promptly corrected. Even typical doses of anesthetic drugs will cause some degree of respiratory depression in a proportion of patients.
Algorithm 1.3: Respiratory Compromise
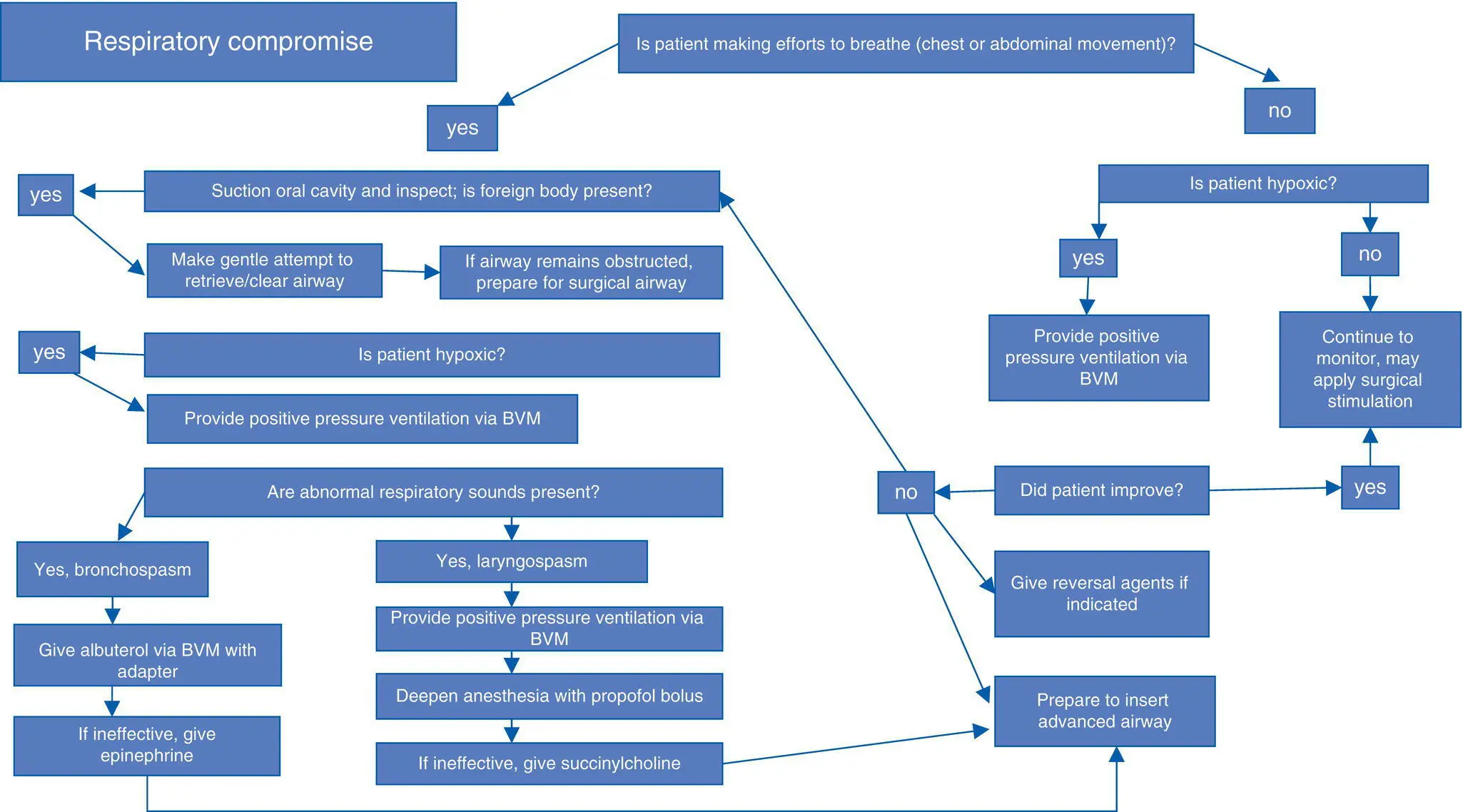
Primary respiratory depression, caused by the provision of anesthesia itself, refers to a deficit in ventilation or oxygenation or both. Respiratory depression may take the form of mechanical obstruction, caused by collapse of the oropharyngeal soft tissues or occlusion of the airway by the tongue or secretions. Central respiratory depression, characterized by hypopnea or apnea, can also occur either separately or concurrently.
Typically, mechanical obstruction occurs more frequently and at lower anesthetic doses than central apnea does, and it occurs to some extent in susceptible persons. Obese patients, those with short thick necks, those with mandibular retrognathia, and patients with OSA are among the most susceptible groups. In severe cases, this may render these patients unsuitable for ambulatory anesthetic procedures. In most other cases, patient positioning can play a role in airway obstruction. Respiratory obstruction due to mechanical airway obstruction can be managed by careful suctioning, repositioning of the tongue in a forward position, and either a chin lift or jaw thrust maneuver. If necessary, the level of anesthesia may be lessened, as increasing levels of sedation contribute to the degree of airway impediment. Rarely, an oral or nasal airway may be needed to overcome the obstruction in the posterior pharynx and stent the airway open. Supplemental oxygen can be helpful to decrease any oxygen desaturation associated with mild to moderate obstruction, although oxygen by itself does not alleviate the mechanics of obstruction.
Respiratory depression may also be “central,” characterized by a decreased respiratory rate or periods of apnea. Narcotic drugs are most often implicated because of their effects on the medullary respiratory center of the brainstem that results in decreased respiratory drive and decreased response to hypercapnia. At moderate levels of narcotic effect, the decreased respiratory rate is accompanied by a compensatory increase in tidal volume that prevents oxygen desaturation. At higher levels of narcotic sedation, respiratory depression can progress to apnea and respiratory arrest. A brief period of respiratory support in the form of supplemental oxygen via a face mask with cessation of anesthetic drug administration may be all that is necessary in terms of management – particularly with short‐acting drugs in a patient with good respiratory reserve. Whenever there is desaturation in a setting of frank apnea, however, the patient's ventilation should be assisted by a positive pressure face mask until spontaneous respiration resumes.
Читать дальше