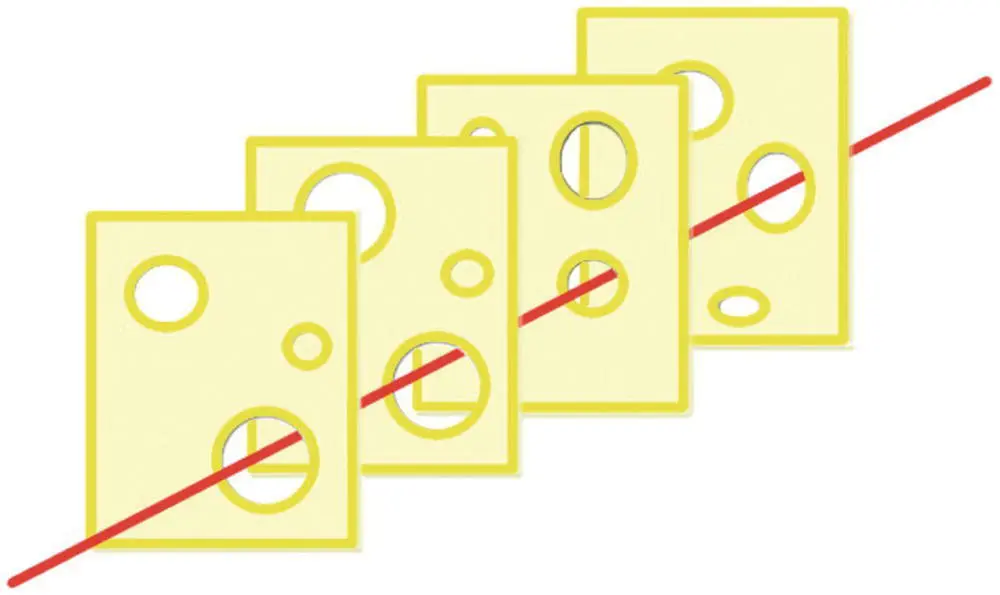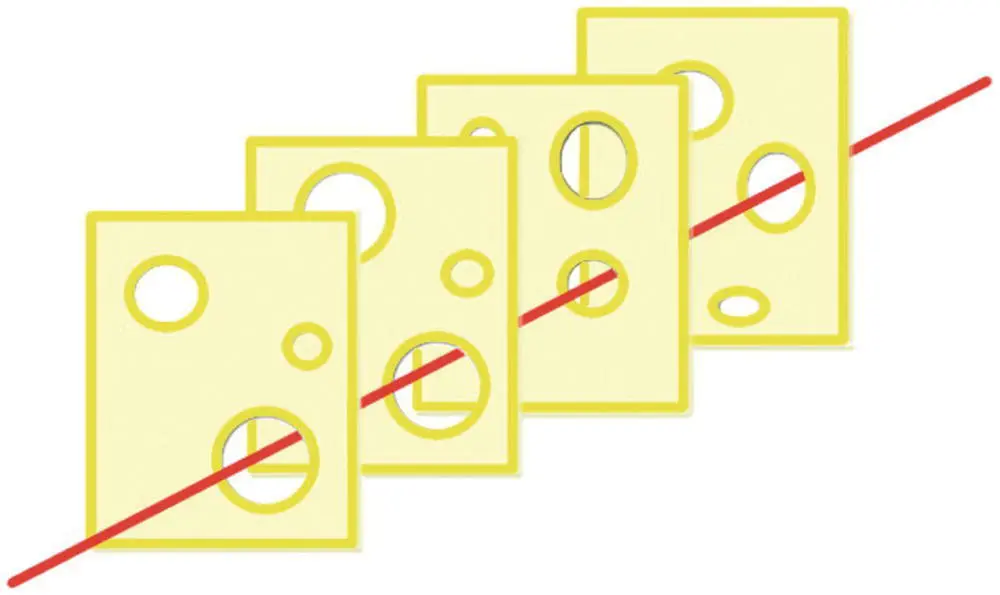
Figure 4.1 The ‘Swiss cheese’ model
Each of the slices of Swiss cheese represents barriers that, under ideal circumstances, would prevent or detect error. The holes represent weaknesses in these barriers; if the holes align the error passes through undetected with the potential to cause poor outcome and patient harm.
Reconsider the example of drug error using the Swiss cheese model. The first slice is the doctor writing the prescription, the second slice is the organisation’s drug policy, the third is the midwife who draws up the drug and the fourth is the midwife who second checks the drug.
Now consider the following: What if the doctor is relatively new to the obstetric unit and unfamiliar with the specific drugs or doses used in this situation? – their ‘slice of cheese’ has larger holes. What if the organisation has failed to develop a robust drug policy that is fit for purpose and guidelines are out of date or not easily accessed? – this second slice is considerably weakened or may even be removed completely. What if the drug is drawn up by a midwife who has just returned from a career break who is not familiar with the particular antihypertensive drug used? – their ‘slice’ has also got larger holes. Labour wards are often chronically short of staff and the midwife who performs the second drug check is distracted as they are looking after two high‐risk women in labour. Inadvertently their check is only cursory – this final slice (or barrier) is completely removed.
The end result is that multiple defences have been weakened or removed and error leading to unintentional harm is more likely. Also be aware of the different types of failure within the system: (i) latent failures include organisational error (e.g. no effective policy, out‐of‐date guidelines and inadequate staffing levels); and (ii) active failures (e.g. failure to escalate, drug errors, failure to monitor or act on deteriorating vital signs).
Historically, those making mistakes have been identified and singled out for punishment and/or retraining, in what is often referred to as a culture of blame. With our example drug error blame would most likely have fallen on the shoulders of the nurse administering and/or the doctor incorrectly prescribing. Does retraining these individuals make it safer for other or future patients? That clearly depends on the underlying reasons. If it was purely a knowledge gap, possibly, but does the same knowledge gap exist elsewhere? Potentially all the other issues remain unresolved. Moreover such punitive reactions make it less likely for individuals to admit mistakes and near misses in the future.
The focus is now on learning from error and, in shifting away from the individual, is much more focused on determining the system/organisational errors. Once robust systems, procedures and policies that work and are effective are in place, then errors can be captured. Of course issues will still need to be addressed where individuals have been reckless or lacked knowledge – but now reasons why the individuals felt the need to violate, or had not been given all the knowledge required, can be looked at.
For this to work health services need to learn from errors, adverse events and near misses. This requires engagement at both the individual level, by reporting errors, and the organisational level, investigating and feeding back the error using a systematic approach. It is also key that information is cascaded through the organisation and across the health service to raise awareness and prevent similar situations.
Violation may be indicative of the failure of systems, procedures or policies or other cultural issues. It is important that policies, procedures, roles and even our buildings and equipment are all designed proactively with human factors in mind so things do not have to be fixed retrospectively when adverse events occur. This means that all members of the organisation must be aware of human factors, not just the front‐line clinical staff.
Improving team and individual performance
Having discussed the magnitude of the problem of healthcare error, the rest of this chapter will focus on how the performance of teams and individuals can be developed.
Raising awareness of the human factors and being able to practise these skills and behaviours within multiprofessional teams allows the development of effective teams in all situations. Simulation activity allows a team to explore these new ideas, practise them and develop them. To do this we need feedback on our performance within a safe environment where no patient is at risk and egos and personal interests can be set aside. Consider how you developed a clinical skill. It was something that needed to be practised again and again until eventually it started to become automatic and routine. The same applies for our human factor behaviours. In addition, recognising our inherent human limitations and the situations when errors are more likely to occur, we can all be hypervigilant when required.
Poor communication is the leading cause of adverse events. This is not surprising; to have an effective team there needs to be good communication. The leader needs to communicate with the followers, and followers communicate with leaders and other followers. Communication is not just saying something – it is ensuring that information is accurately passed on and received. We all want to ensure effective communication at all times. Remember there are multiple components to effective communication ( Table 4.2).
Table 4.2 Elements of communication
| Sender |
Sender |
Transmitted |
Receiver |
Receiver |
| Thinks of what to say |
Communicates message |
Face to face/phone/email |
Hears and confirms message |
Considers and acts |
When communicating face to face a lot of the information is transmitted non‐verbally, which can make telephone or email conversations more challenging. Communication can be more difficult when talking across professional, specialty or hierarchal barriers as we do not always talk the same technical language, have the same levels of understanding, or even have a full awareness of the other person’s role.
There are a variety of tools to aid communication, for example SBAR (situation, background, assessment and recommendation). SBAR is designed for acute clinical communications. It facilitates the sender to plan and organise the message, make it succinct and focused, and provide it in a logical and expected order. It is also an empowerment tool allowing the sender (who may be more junior) to request an action from a more senior individual. Find out what communication tool your organisation uses and practise using it; look out for other staff using it too. While these tools are useful, they tend to be reserved for certain situations, whereas we want to establish effective communication as the routine not the exception. One method to routinely improve communication is to incorporate a feedback loop.
Effective communication with a feedback loop
Errors can occur at any level or multiple levels. Consider a busy clinical situation and the team leader shouts ‘ We need four units of blood’ or ‘ Will someone order four units of blood ’ while managing an ongoing postpartum haemorrhage (PPH) – what happens? The majority of times nothing – nobody goes to bring the blood! So how can this be improved? Avoid using instructions like the two examples above – remember – nobody is called ‘someone’! Most obviously an individual can be identified to perform the task, by name: ‘ Michael can you please order four units of blood? ’ If Michael says ‘ Yes ’ effective communication might be assumed; but not always. What has Michael heard and what will he do? At the moment we do not really know what message has been received. Michael might dash over with a cup of tea as this is what he thought he heard. This may seem a slightly strange thing to happen; but how often in a clinical emergency have you asked for something and been presented with something else? People are less likely to ask questions in emergencies as everyone is busy. This could be the catalyst for an error or precipitate a missed task. So how do we find out what message Michael received? The easiest way is to use specific ‘task allocation’ incorporated within a formal ‘feedback loop’ (also known as ‘closed loop communication’).
Читать дальше