Although phagocytic cells are effective killers of bacteria and are essential for clearing the invading bacteria from an infected area, the body can pay a high price for this service. During active killing of a bacterium, lysosomal enzymes are released into the surrounding area as well as into the phagolysosome. Released lysosomal enzymes damage adjacent tissues and can be the main cause of tissue damage that results from a bacterial infection. Also, PMNs, NK cells, and macrophages kill themselves as a result of their killing activities, and lysosomal granules released by dying PMNs contribute further to tissue destruction. Pus, a common sign of infection, is composed mainly of dead PMNs and tissue cells. If pus accumulates in an enclosed tissue area, then an abscess can form. Pus is usually whitish or yellowish in color, but sometimes it can have a greenish color due to the abundant presence of myeloperoxidase. Bacteria that cause pus formation are called suppurative, purulent, or pyogenic.
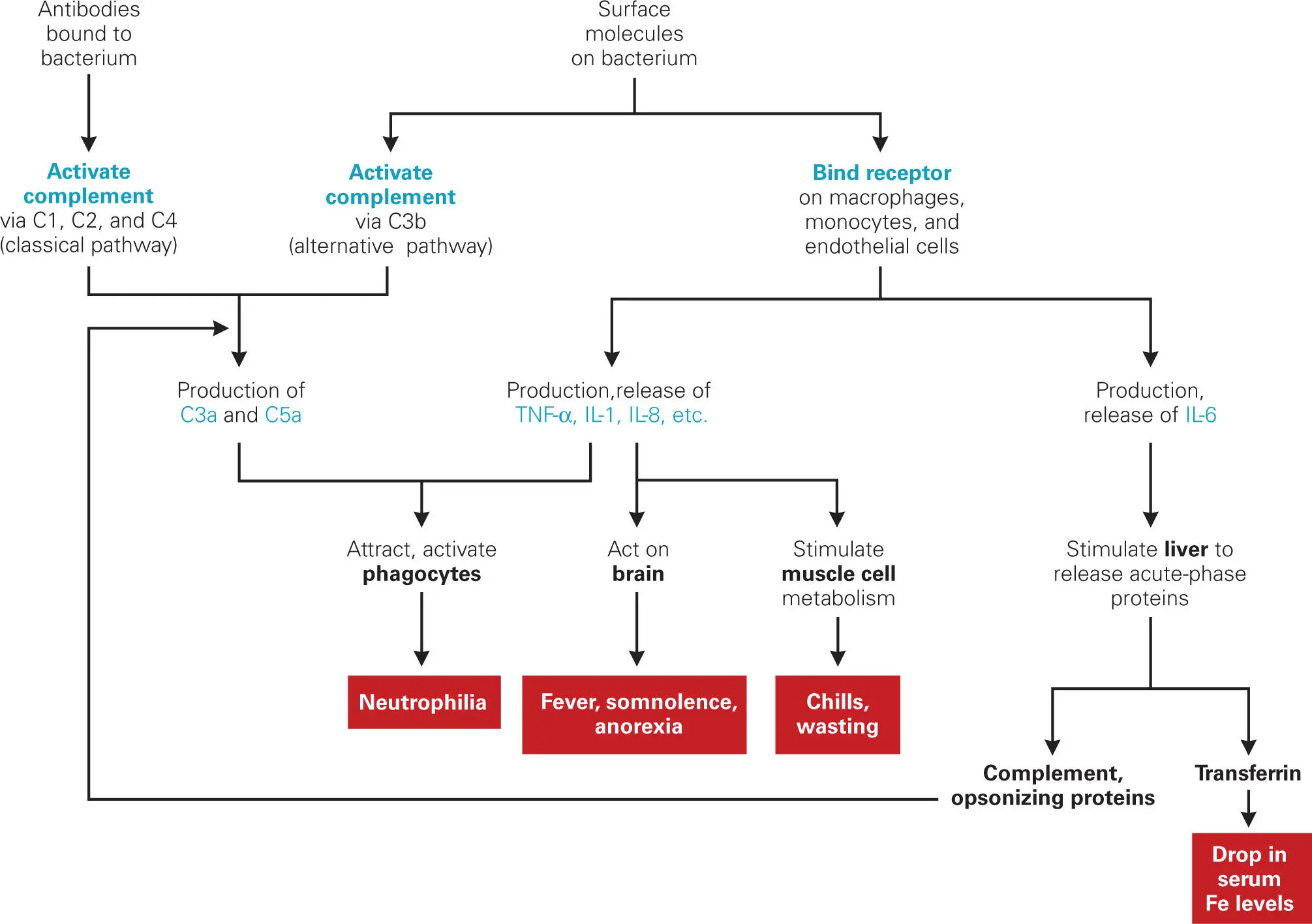
Some of the other roles of the proinflammatory cytokines are listed in Table 3-2and illustrated in Figure 3-16. These proinflammatory cytokines are responsible for common symptoms of infectious diseases other than those localized at the site of infection: fever, somnolence (drowsiness), malaise, anorexia, chills, decrease in blood iron levels, and weight loss. Cytokines IL-1 and TNF-α interact with the hypothalamus and adrenal gland to produce fever and somnolence, which the patient interprets as a feeling of malaise. Indifference to food, which can also characterize this state, contributes to the anorexia. TNF-α and other cytokines stimulate muscle cells to increase their metabolic rate and catabolize proteins to provide fuel for the mobilization of host defenses. Increased metabolism of muscle cells may be the cause of chills seen in some types of systemic infections. If the infection persists, the combination of anorexia and muscle cell breakdown of protein results in weight loss and visible loss of muscle tissue (wasting syndrome).
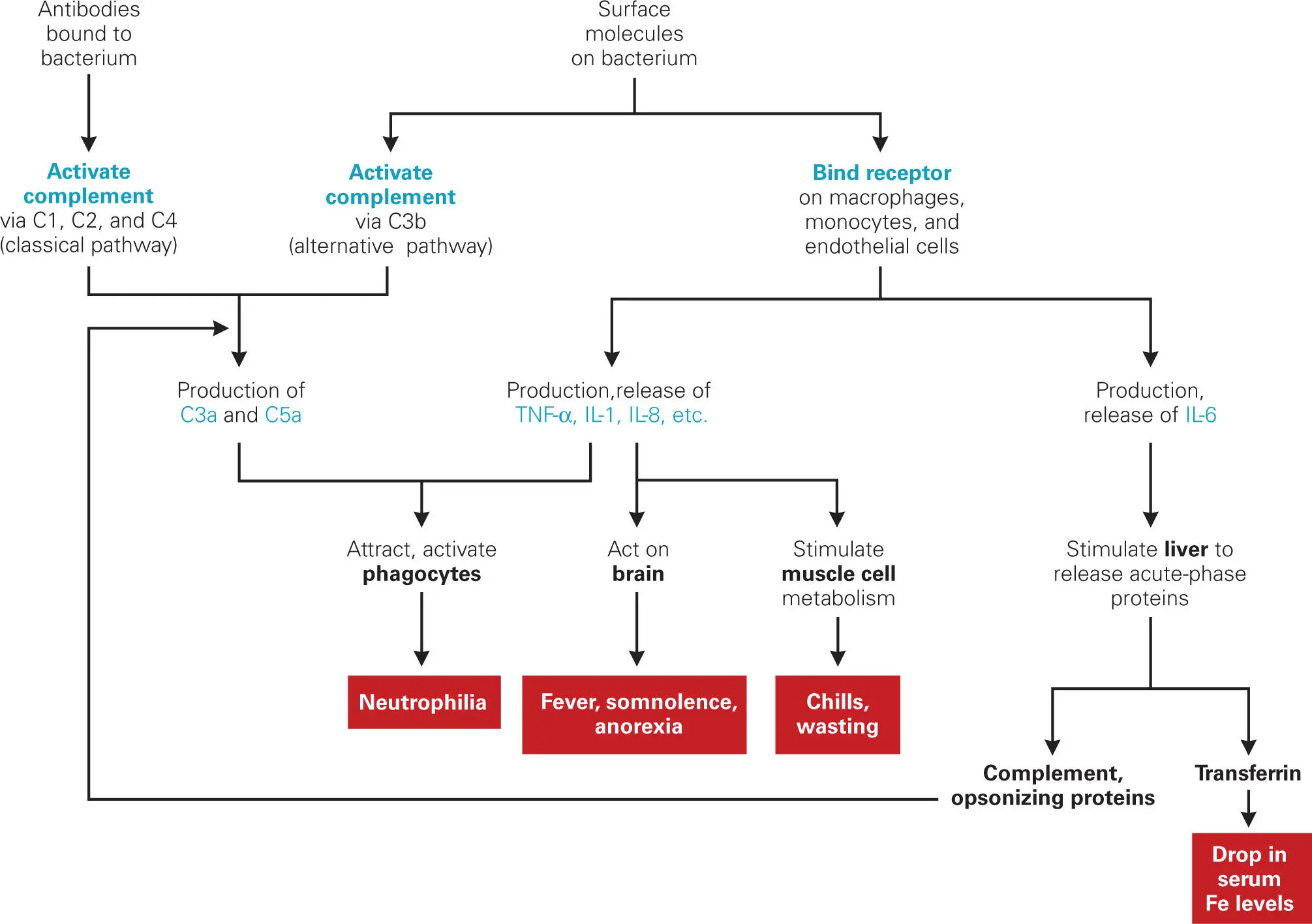
Figure 3-16. Overview of nonspecific responses to infection and the effects of cytokines on these responses. Proinflammatory cytokines include TNF-α, IL-1, IL-6, and IL-8, as well as the complement components C3a, C4a, C2b, and C5a. C3a, C4a, and C5a act as anaphylatoxins that increase histamine and heparin release from mast cells and basophils, smooth muscle contraction, and vascular permeability. C5a and (to a lesser extent) C3a also act as potent chemokines (enhancing chemotaxis of phagocytes to the infection site).
The cytokine IL-6 released from macrophages and T cells stimulates the liver to increase production of transferrin (to sequester iron), complement components (to regenerate complement components used up during complement activation), LPS-binding proteins (to continue stimulation of cytokine production as long as bacteria are detected in the body), and two general opsonins—MBL, discussed above in the context of complement, and C-reactive protein (CRP). CRP is a pentameric protein produced in the liver whose expression and release into blood is greatly up-regulated in response to IL-6 during inflammation. CRP is also another PAMP recognition protein in that it binds to LTA of some bacterial species as well as to phosphocholine found on the surface of dead or dying bacterial cells. Phagocytes have receptors for CRP, which allows it to act as an opsonin by enhancing phagocytosis.
Septic Shock: The Dark Side of the Innate Defenses
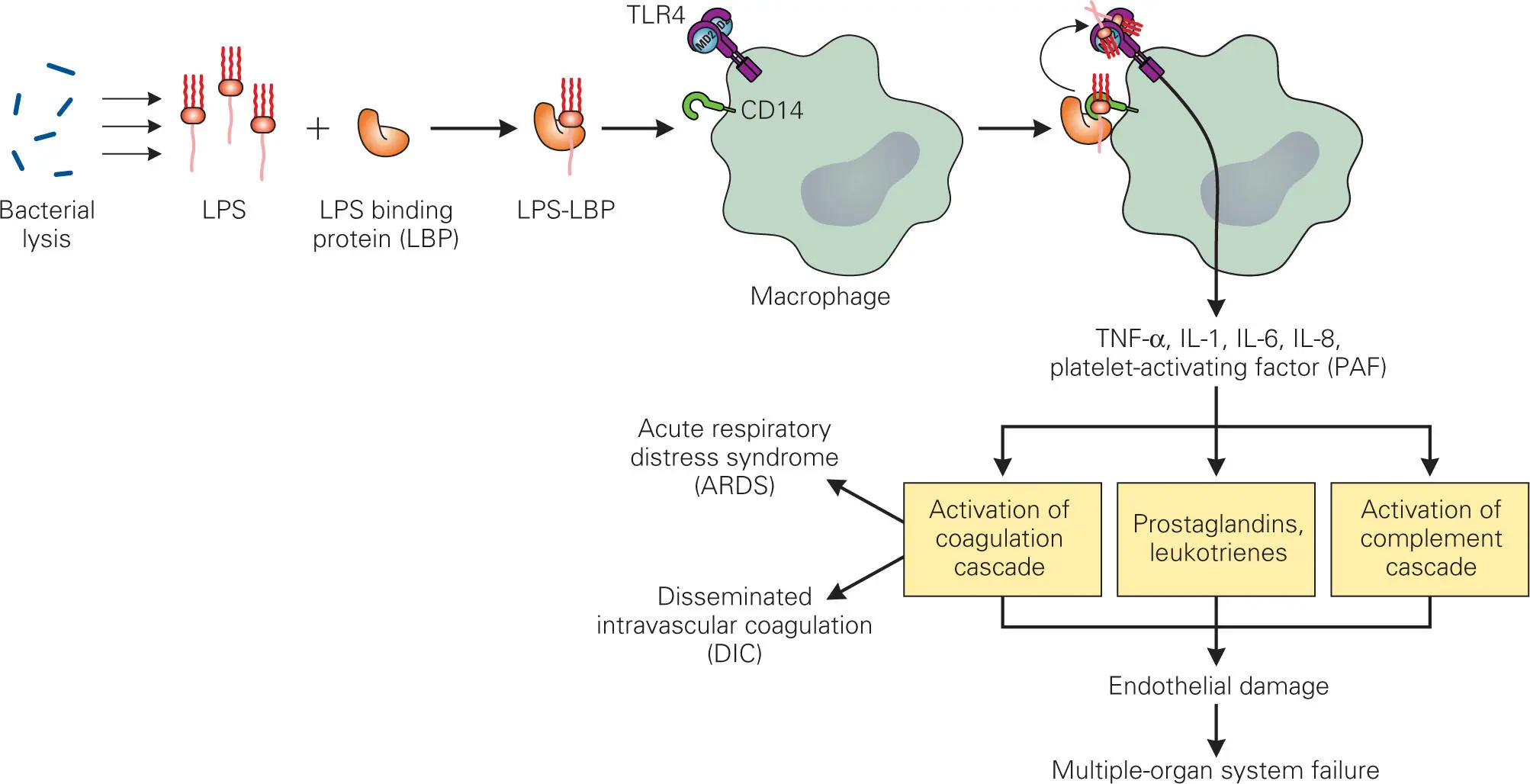
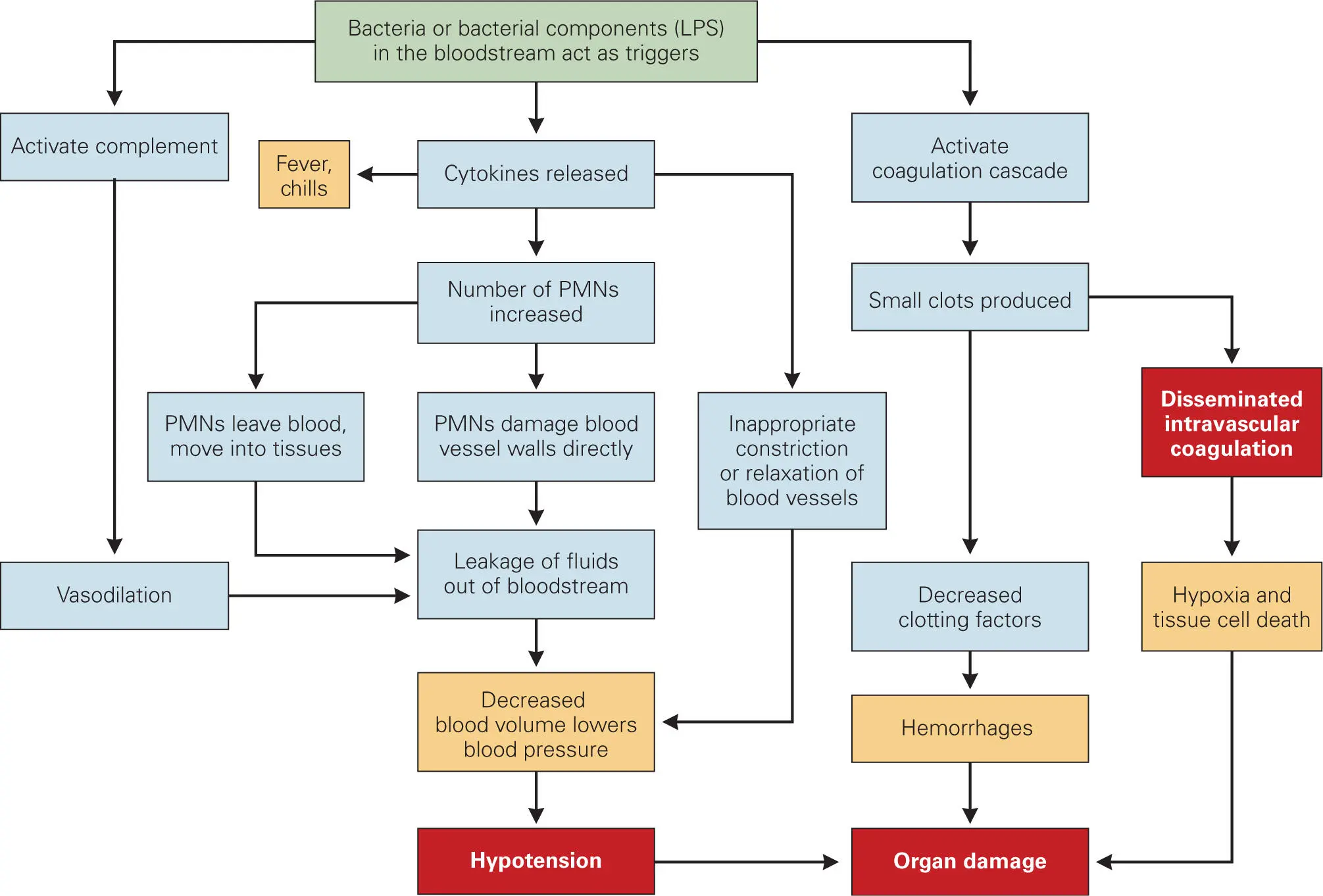
Inappropriately functioning or over-stimulated host defenses can sometimes lead to disastrous consequences such as septic shock. Septic shock is a form of shock caused by bacterial infection ( Figure 3-17), during which a massive release of cytokines (sometimes called a cytokine storm) leads to a subsequent overwhelming inflammatory response. Other causes of shock include massive crush injuries, burns, radiation poisoning, and exposure to toxins (toxic shock). In people with septic shock, vasodilation causes a dramatic drop in vascular resistance and blood pressure (hypotension) despite normal-to-high cardiac output. The heart rate and respiratory rate increase as the body tries to compensate for decreasing blood pressure and lack of oxygen. Septic shock is a serious condition because severely reduced levels of blood flow deprive essential organs of oxygen and nutrients (ischemia), causing them to malfunction. The consequent failure of multiple organs, such as the kidneys, heart, brain, and lungs, is the usual cause of death in septic shock patients.
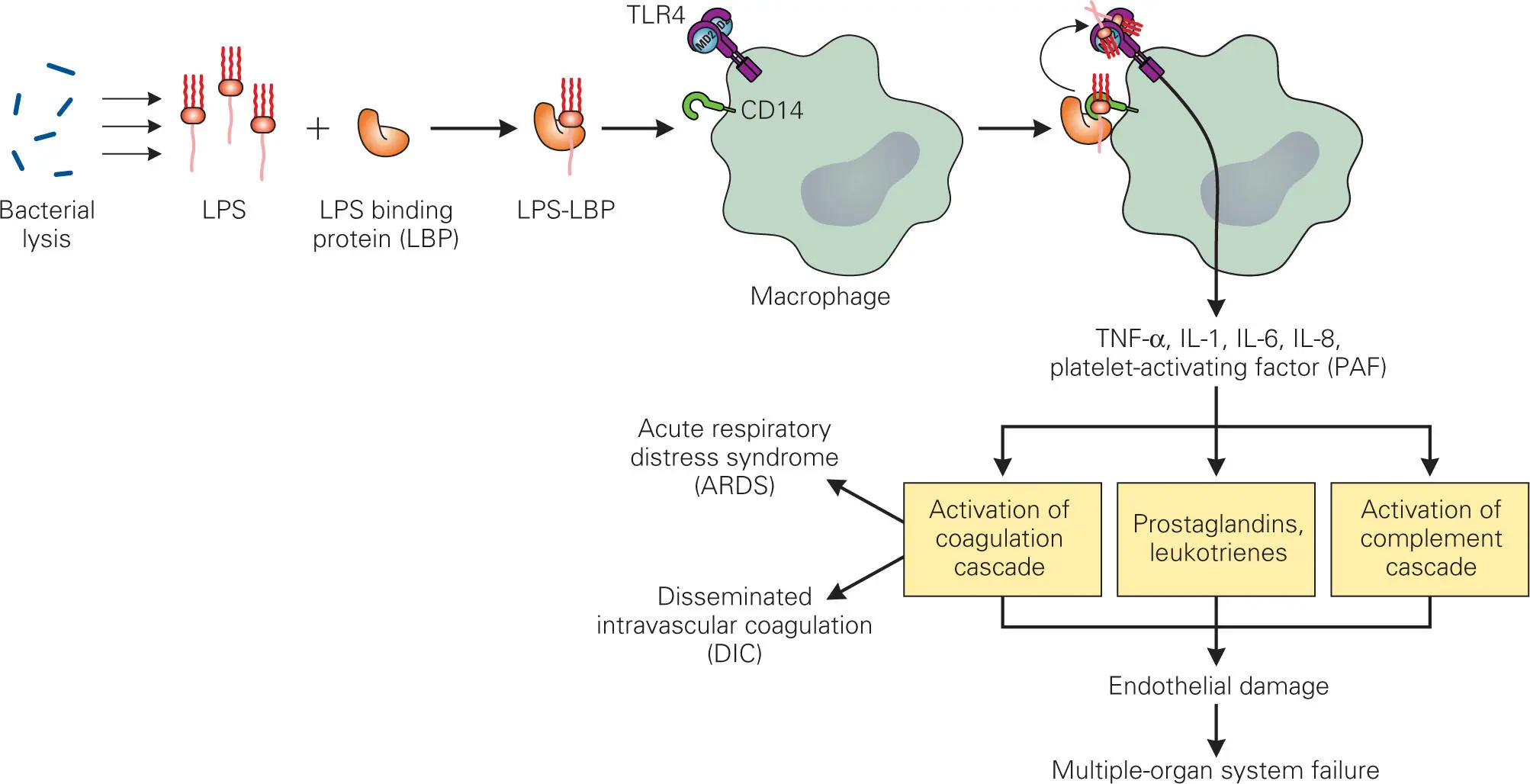
Figure 3-17. Triggering of proinflammatory cytokine release by Gram-negative LPS and its role in septic shock. TNF-α, IL-1, IL-6, and IL-8 are proinflammatory cytokines.
Septicemia (bacteria infecting and growing in the bloodstream) is one of the leading causes of septic shock and occurs in 500,000 to 750,000 patients per year in the United States alone. Up to half of the patients with septicemia end up dying in the hospital. Even those who survive may have long-term aftereffects, such as stroke or permanent damage to lungs, kidneys, liver, or other organs. Indeed, statistics show that those who survive an episode of septic shock have a significantly greater risk of dying during the next five-year period than people with the same underlying conditions but no previous episode of shock. Septic shock is not only serious business for the patient, but it is also a seriously expensive business, as hospital administrators and insurance executives are quick to point out, with annual hospital costs of $5 to 10 billion.
The all-inclusive term sepsis has now been defined more precisely in an effort to aid diagnosis of the various stages of disease. The first stage of shock, called systemic inflammatory response syndrome (SIRS), is characterized by a temperature over 38°C or under 36°C, elevated heart rate, elevated respiratory rate, and an abnormally high or low neutrophil count. The second stage, termed sepsis, is SIRS with a culture-documented infection (i.e., laboratory results showing the presence of bacteria in the bloodstream). The third stage is severe sepsis, characterized by organ dysfunction and very low blood pressure (hypotension). The fourth stage is septic shock, which is characterized by low blood pressure despite intravenous fluid administration.
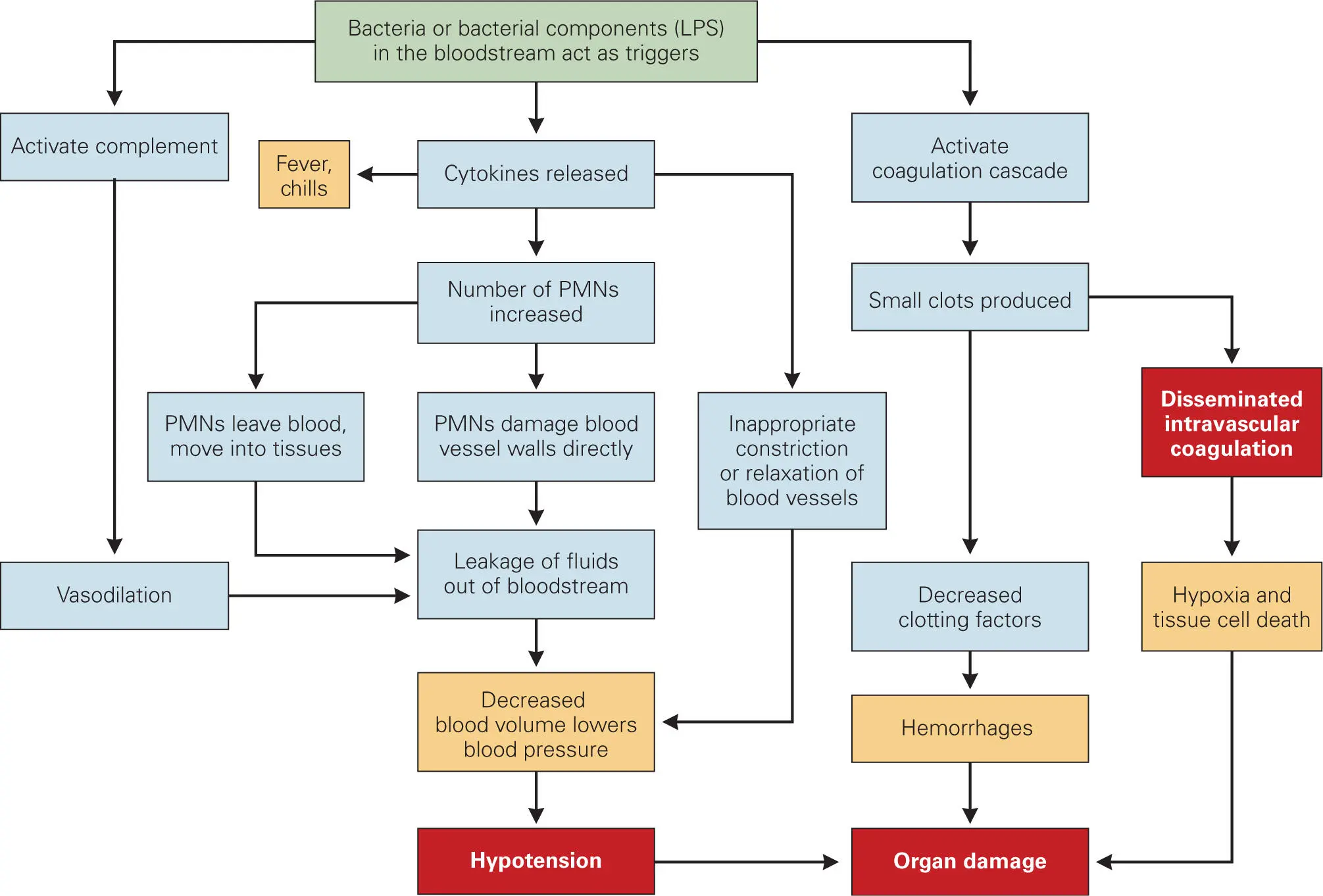
How does a bacterial infection of the bloodstream produce such a serious condition? Steps involved in septic shock are illustrated in more detail in Figure 3-18. From previous sections of this chapter, it should be evident that the body goes to great lengths to confine the inflammatory response to specific areas of the body. Septic shock is an example of what happens when an inflammatory response is triggered throughout the body. Shock occurs when bacteria or their products reach high enough levels in the bloodstream to trigger complement activation, cytokine release, and the coagulation cascade in many parts of the body. High levels of cytokines, especially TNF-α, IL-1, IL-6, IL-8, and IFN-γ, cause increased levels of PMNs in the blood and encourage these PMNs to leave the blood vessels throughout the body. This leads to massive leakage of fluids into surrounding tissue. PMNs and macrophages activated by IFN-γ also damage blood vessels directly, resulting in loss of fluid from these vessels.
Читать дальше