Cocaine, in addition to being a local anaesthetic ( Chapter 5), is a sympathomimetic because it inhibits the reuptake of norepinephrine by nerve terminals. It has an intense central stimulant effect that has made it a popular drug of abuse ( Chapter 31).
Directly acting sympathomimetics
The effect of sympathomimetic drugs in humans depends on their receptor specificity (α and/or β) and on the compensatory reflexes they evoke.
Epinephrineand norepinephrineare destroyed in the gut and are short lasting when injected because of uptake and metabolism. Epinephrine increases the blood pressure by stimulating the rate and force of the heartbeat (β 1‐effects). Stimulation of vascular α‐receptors causes vasoconstriction (viscera, skin), but β 2‐stimulation causes vasodilatation (skeletal muscle) and the total peripheral resistance may actually decrease.
Norepinephrine has little or no effect on the vascular β 2‐receptors, and so the α‐mediated vasoconstriction is unopposed. The resulting rise in blood pressure reflexively slows the heart, usually overcoming the direct β 1‐stimulant action on the heart rate.
Epinephrine by injection has an important use in the treatment of anaphylactic shock ( Chapter 11).
β‐receptor‐selective drugs
Isoprenalinestimulates all β‐receptors, increasing the rate and force of the heartbeat and causing vasodilatation. These effects result in a fall in diastolic and mean arterial pressure with little change in systolic pressure.
β2‐adrenoceptor agonistsare relatively selective drugs that produce bronchodilatation at doses that cause minimal effects on the heart. They are resistant to MAO and are probably not taken up into neurones. Their main use is in the treatment of asthma ( Chapter 11).
Adrenoceptor antagonists
α‐blockers
α‐blockersreduce arteriolar and venous tone, causing a fall in peripheral resistance and blood pressure ( Chapter 15). α‐blockers cause a reflex tachycardia, which is greater with non‐selective drugs that also block α 2‐presynaptic receptors on the heart, because the augmented release of norepinephrine stimulates further the cardiac β‐receptors. Prazosin, a selective α 1‐antagonist, causes relatively little tachycardia. BPHis common in men over 50 years old. As the prostate gland increases in size, pressure on the urethra obstructs urine flow. α 1‐blockers increase urine flow (at least partially) by relaxing smooth muscle in the gland. Tamsulosinis selective for α 1A‐adrenoceptors and is better tolerated than other antagonists.
β‐blockersvary in their lipid solubility and cardioselectivity . However, they all block β 1‐receptors and are equally effective in reducing blood pressure and preventing angina. The more lipid‐soluble drugs are more rapidly absorbed from the gut, undergo more first‐pass hepatic metabolism and are more rapidly eliminated. They are also more likely to enter the brain and cause central effects (e.g. bad dreams). Cardioselectivity is only relative and diminishes with higher doses. Nevertheless, selective β 1‐blockade seems to produce less peripheral vasoconstriction (cold hands and feet) and does not reduce the response to exercise‐induced hypoglycaemia (stimulation of gluconeogenesis in the liver is mediated by β 2‐receptors). Cardioselective drugs may have sufficient β 2‐activity to precipitate severe bronchospasm in patients with asthma and they should avoid β‐blockers. Some β‐blockers possess intrinsic sympathomimetic activity (i.e. are partial agonists, Chapter 2). The clinical importance of this is debatable, see Chapter 16.
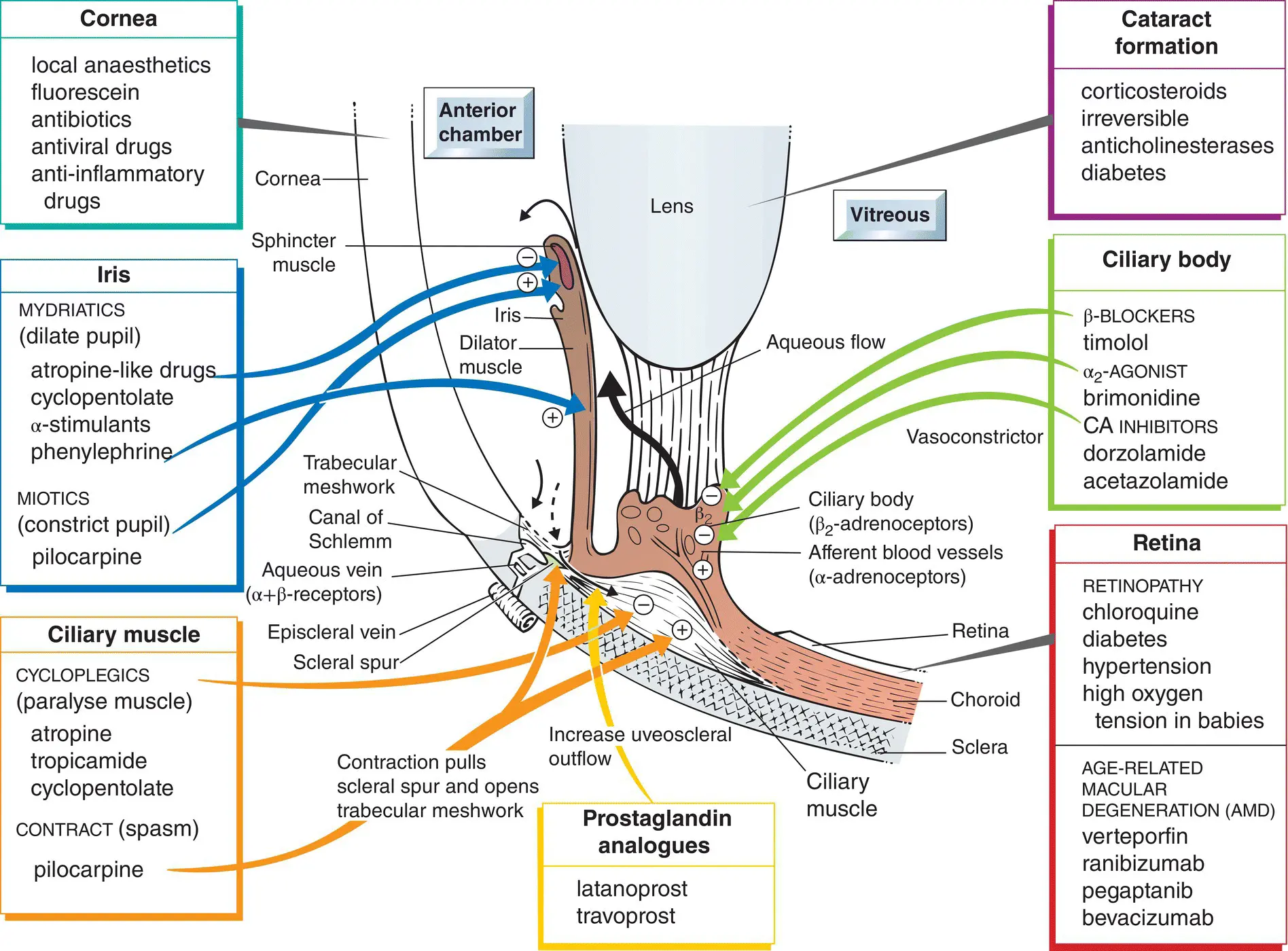
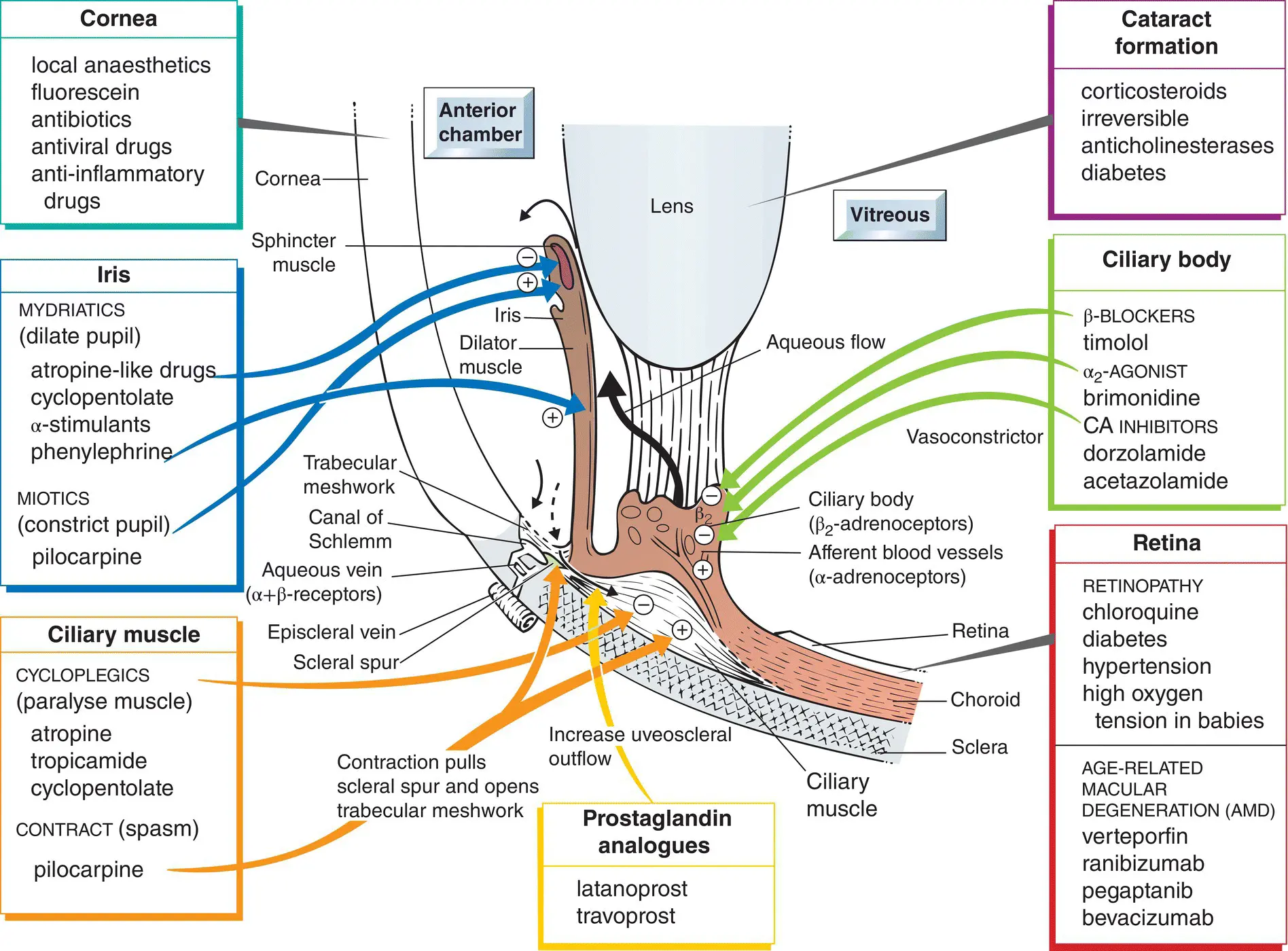
The eye is an inflated spherical shell, its outer layer being the tough, collagen‐rich sclera. The normal intraocular pressure(IOP) is about 15 mmHg. It is maintained by a balance of aqueous humour formation by the ciliary body (  ) and outflow through the trabecular meshwork into the canal of Schlemm (
) and outflow through the trabecular meshwork into the canal of Schlemm (  ) or the uveoscleral pathway (
) or the uveoscleral pathway (  ). In open‐angle glaucoma, pathological changes in the retina progressively cause the death of ganglion cells and loss of vision. This process is often, but not always, associated with elevated IOP. Irrespective of the initial IOP, a reduction of the IOP by 20–40% reduces the average rate of visual loss by 50%. The pressure is reduced, usually with topical drugs. This is usually achieved either by increasing aqueous outflow with a prostaglandin analogue(bottom centre) or by reducing aqueous formation with a β‐blocker(middle right).
). In open‐angle glaucoma, pathological changes in the retina progressively cause the death of ganglion cells and loss of vision. This process is often, but not always, associated with elevated IOP. Irrespective of the initial IOP, a reduction of the IOP by 20–40% reduces the average rate of visual loss by 50%. The pressure is reduced, usually with topical drugs. This is usually achieved either by increasing aqueous outflow with a prostaglandin analogue(bottom centre) or by reducing aqueous formation with a β‐blocker(middle right).
At the front of the eye, the sclera runs into the cornea(top left), whose transparency is obtained by alignment of the collagen fibres. Many superficial manipulations, such as tonometry (measurement of the IOP) and the removal of corneal foreign bodies, require the instillation of a local anaesthetic . Fluoresceinis commonly instilled into the eye to reveal damaged areas of corneal epithelium, which are stained bright green by the dye. Inflammationof the cornea resulting from allergy or chemical burns is treated with topical anti‐inflammatory drugs ( Chapter 33). Infections are not treated with anti‐inflammatory agents, except together with an effective chemotherapeutic agent, because anti‐inflammatory drugs reduce resistance to invading microorganisms.
The iris(middle left) possesses a sphincter muscle, which receives parasympathetic nerves, and a dilator muscle, which is innervated by sympathetic fibres. Thus, muscarinic antagonists and α‐adrenoceptor agonists dilate the pupil ( mydriasis), while muscarinic agonists and α‐adrenoceptor antagonists constrict the pupil ( miosis).
Contraction of the parasympathetically innervated ciliary muscle(bottom left) allows the lens to become thicker and accommodation for near vision occurs. Thus, muscarinic antagonists paralyse the ciliary muscle ( cycloplegia) and prevent accommodation for near vision, while agonists cause accommodation and a loss of far vision.
The lens(middle top) provides the adjustable part of the eye's refractive power. Opacity of the lens is called a cataract. Some drugs, notably corticosteroids, may cause cataracts.
The retinais a part of the central nervous system, but it seems little affected by drugs, probably because of the effective blood–retinal barrier. Verteporfinand inhibitors of vascular endothelial growth factor (VEGF; bottom, right) are used to treat age‐related macular degeneration (AMD).
The retina may occasionally be damaged by drugs (e.g. bottom right) or by high oxygen tension in newborn babies.
Читать дальше
 ) and outflow through the trabecular meshwork into the canal of Schlemm (
) and outflow through the trabecular meshwork into the canal of Schlemm (  ) or the uveoscleral pathway (
) or the uveoscleral pathway (  ). In open‐angle glaucoma, pathological changes in the retina progressively cause the death of ganglion cells and loss of vision. This process is often, but not always, associated with elevated IOP. Irrespective of the initial IOP, a reduction of the IOP by 20–40% reduces the average rate of visual loss by 50%. The pressure is reduced, usually with topical drugs. This is usually achieved either by increasing aqueous outflow with a prostaglandin analogue(bottom centre) or by reducing aqueous formation with a β‐blocker(middle right).
). In open‐angle glaucoma, pathological changes in the retina progressively cause the death of ganglion cells and loss of vision. This process is often, but not always, associated with elevated IOP. Irrespective of the initial IOP, a reduction of the IOP by 20–40% reduces the average rate of visual loss by 50%. The pressure is reduced, usually with topical drugs. This is usually achieved either by increasing aqueous outflow with a prostaglandin analogue(bottom centre) or by reducing aqueous formation with a β‐blocker(middle right).