Nicotinic effectsinclude stimulation of all autonomic ganglia. However, the action of acetylcholine on ganglia is relatively weak compared with its effect on muscarinic receptors, and so parasympathetic effects predominate. The nicotinic actions of acetylcholine on the sympathetic system can be demonstrated, for example, on cat blood pressure, by blocking its muscarinic actions with atropine. High intravenous doses of acetylcholine then cause a rise in blood pressure, because stimulation of the sympathetic ganglia and adrenal medulla now results in vasoconstriction and tachycardia.
8 Autonomic drugs acting at cholinergic synapses
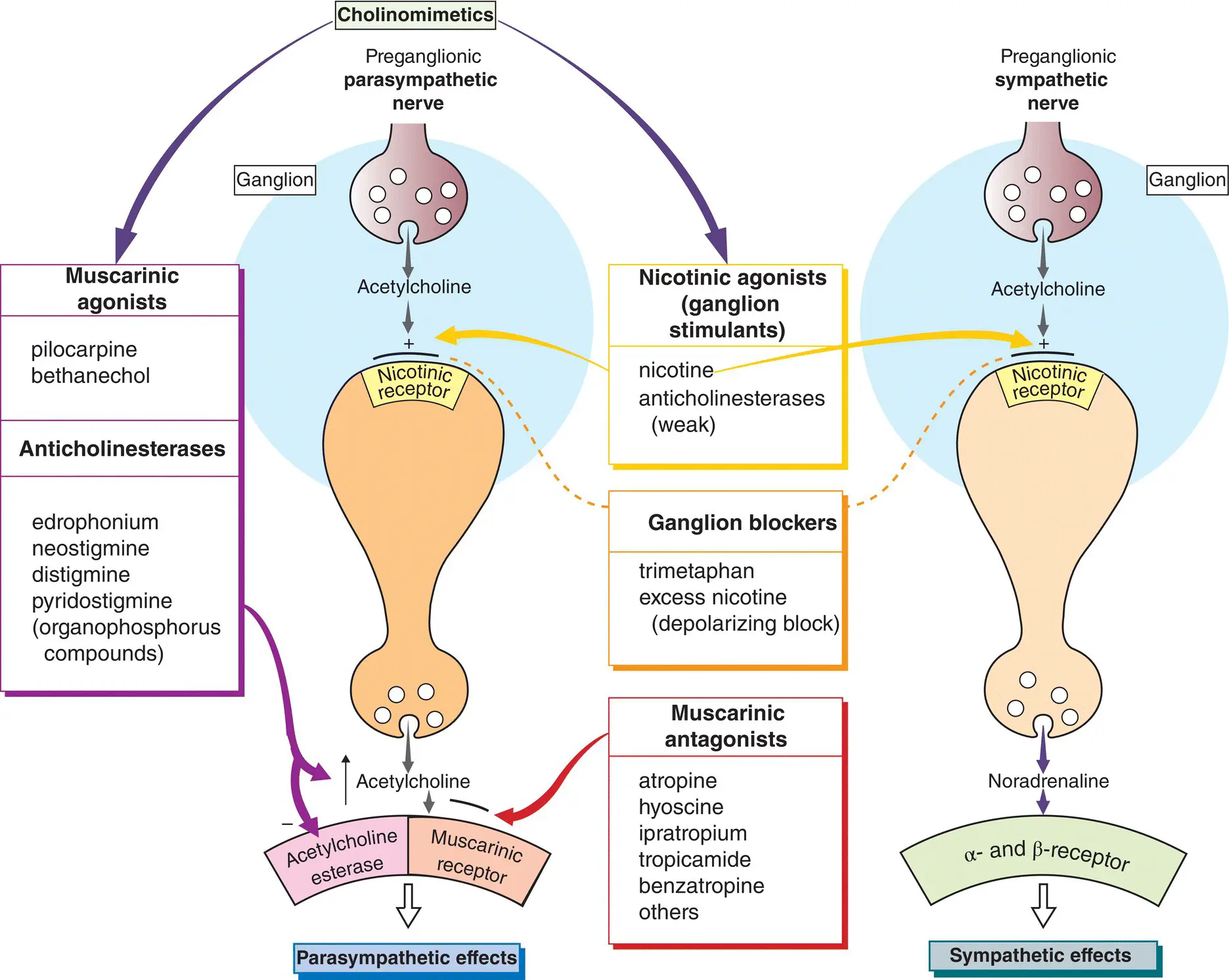
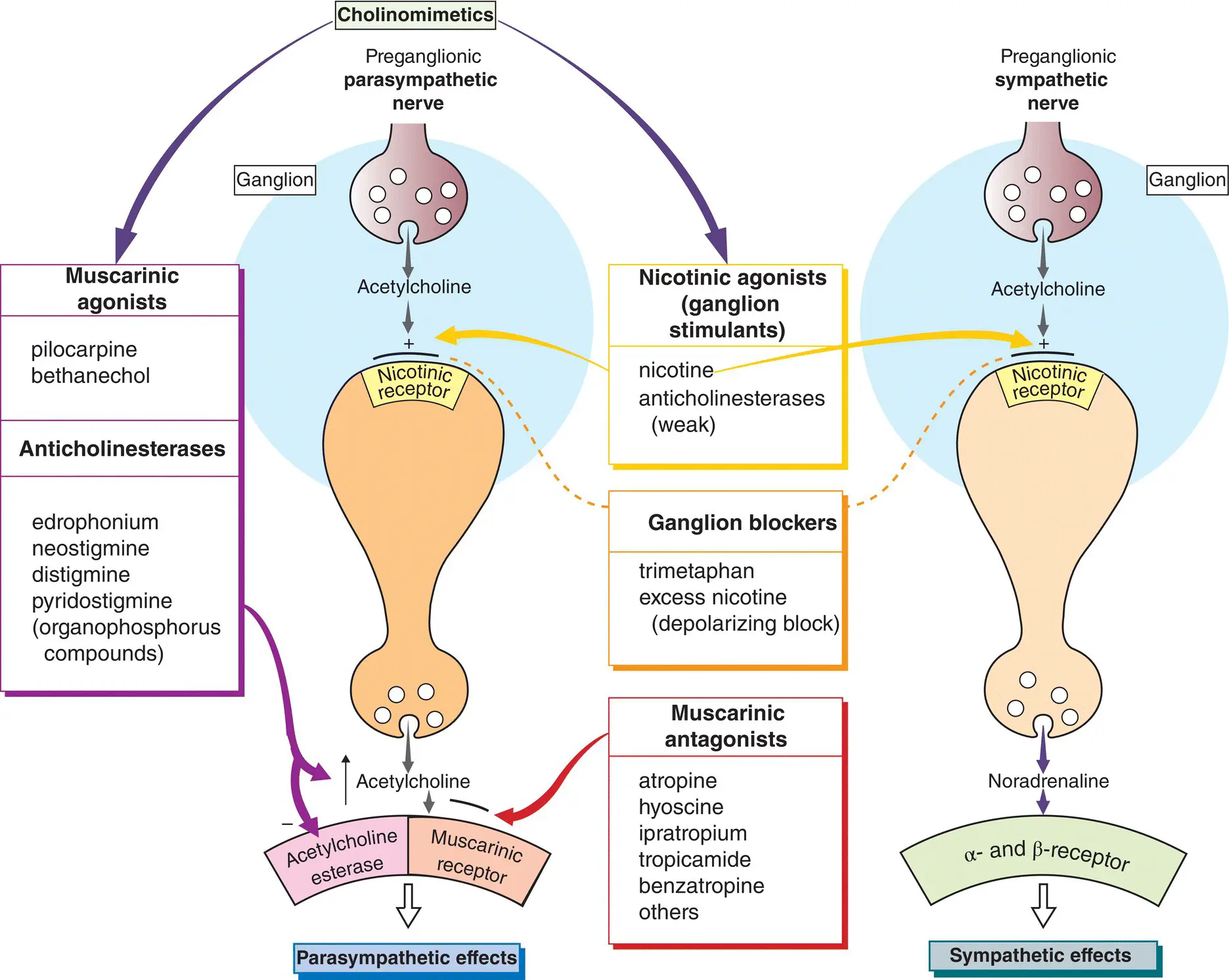
Acetylcholine released from the terminals of postganglionic parasympathetic nerves (left,  ) produces its actions on various effector organs by activating muscarinic receptors(
) produces its actions on various effector organs by activating muscarinic receptors(  ). The effects of acetylcholine are usually excitatory, but an important exception is the heart, which receives inhibitory cholinergic fibres from the vagus ( Chapter 17). Drugs that mimic the effects of acetylcholine are called cholinomimeticsand can be divided into two groups:
). The effects of acetylcholine are usually excitatory, but an important exception is the heart, which receives inhibitory cholinergic fibres from the vagus ( Chapter 17). Drugs that mimic the effects of acetylcholine are called cholinomimeticsand can be divided into two groups:
drugs that act directly on receptors (nicotinic and muscarinic agonists); and
anticholinesterases, which inhibit acetylcholinesterase and so act indirectly by allowing acetylcholine to accumulate in the synapse and produce its effects.
Muscarinic agonists(top left) have few uses, but pilocarpine(as eyedrops) is sometimes used to reduce intraocular pressure in patients with glaucoma ( Chapter 10). Bethanecholwas used to stimulate the bladder in urinary retention, but it has been superseded by catheterization.
Anticholinesterases(bottom left) have relatively little effect at ganglia and are used mainly for their nicotinic effects on the neuromuscular junction. They are used in the treatment of myasthenia gravis and to reverse the effects of competitive muscle relaxants used during surgery ( Chapter 6).
Muscarinic antagonists(bottom middle) block the effects of acetylcholine released from postganglionic parasympathetic nerve terminals. Their effects can, in general, be worked out by examination of the figure in Chapter 7. However, parasympathetic effector organs vary in their sensitivity to the blocking effect of antagonists. Secretions of the salivary, bronchial and sweat glands are most sensitive to blockade. Higher doses of antagonist dilate the pupils, paralyze accommodation and produce tachycardia by blocking vagal tone in the heart. Still higher doses inhibit parasympathetic control of the gastrointestinal tract and bladder. Gastric acid secretion is most resistant to blockade ( Chapter 12).
Atropine, hyoscine(scopolamine) or other antagonists are used:
1 in anaesthesia to block vagal slowing of the heart and to inhibit bronchial secretion;
2 to reduce intestinal spasm in, for example, irritable bowel syndrome ( Chapter 13);
3 in Parkinson’s disease (e.g. benzatropine, Chapter 26);
4 to prevent motion sickness (hyoscine, Chapter 30);
5 to dilate the pupil for ophthalmological examination (e.g. tropicamide) or to paralyse the ciliary muscle ( Chapter 10);
6 as a bronchodilator in asthma (ipratropium, Chapter 11) and
7 in urinary incontinence antimuscarinic drugs e.g. solfenacin, darifenacin reduce detrusor muscle overactivity.
Transmission at autonomic ganglia (  ) can be stimulated by nicotinic agonists (top middle) or blocked by drugs that act specifically on the ganglionic neurone nicotinic receptor/ionophore (middle). Nicotinic agonists are of no clinical use and ganglion blocking drugs, e.g. hexamethonium, are only of historical interest.
) can be stimulated by nicotinic agonists (top middle) or blocked by drugs that act specifically on the ganglionic neurone nicotinic receptor/ionophore (middle). Nicotinic agonists are of no clinical use and ganglion blocking drugs, e.g. hexamethonium, are only of historical interest.
Cholinergic nerve terminalsin the autonomic nervous system synthesize, store and release acetylcholine in essentially the same way as at the neuromuscular junction ( Chapter 6). Acetylcholinesterase is bound to both the pre‐ and postsynaptic membranes.
Cholinomimetics
Muscarinic agonists
These directly activate muscarinic receptors, usually producing excitatory effects. An important exception is the heart, where activation of the predominantly M 2‐receptors has inhibitory effects on the rate and force of (atrial) contraction. The M 2‐receptors are negatively coupled by a G‐protein (G 1) to adenylyl cyclase, which explains the negative inotropic effect of acetylcholine. Subunits (βγ)) of G 1directly increase K +conductances in the heart causing hyperpolarization and bradycardia ( Chapter 17). Acetylcholine stimulates glandular secretion and causes contraction of smooth muscle by activating M 3‐receptors, which are coupled to the formation of inositol‐1,4,5‐trisphosphate (InsP 3) and diacylglycerol ( Chapter 1). InsP 3increases cytosolic Ca 2+, thus triggering muscle contraction or glandular secretion. An intravenous injection of acetylcholine causes vasodilatation indirectly by releasing nitric oxide (NO) from vascular endothelial cells ( Chapter 16). However, most blood vessels have no parasympathetic innervation and so the physiological function of vascular muscarinic receptors is uncertain.
Bethanecholis a quaternary compound that does not penetrate the blood–brain barrier. Its actions are much more prolonged than those of acetylcholine, because it is not hydrolyzed by cholinesterase.
Pilocarpinepossesses a tertiary N atom, which confers increased lipid solubility. This enables the drug to penetrate the cornea readily when applied locally, and enter the brain when given systemically.
These are indirectly acting cholinomimetics. The commonly used anticholinesterase drugs are quaternary compounds that do not pass the blood–brain barrier and have negligible central effects. They are poorly absorbed orally. Physostigmine(eserine) is much more lipid soluble. It is well absorbed after oral or local administration (e.g. as eyedrops) and passes into the brain.
Initially, acetylcholine binds to the active site of the esterase and is hydrolyzed, producing free choline and acetylated enzyme. In a second step, the covalent acetyl–enzyme bond is split with the addition of water. Edrophoniumis the main example of a reversible anticholinesterase. It binds by electrostatic forces to the active site of the enzyme. It does not form covalent bonds with the enzyme and so is very short acting (2–10 min). The carbamate esters (e.g. neostigmine, pyridostigmine) undergo the same two‐step process as acetylcholine, except that the breakdown of the carbamylated enzyme is much slower (30 min to 6 h). Organophosphorus agents result in a phosphorylated enzyme active site. The covalent phosphorus–enzyme bond is very stable and the enzyme is inactivated for hundreds of hours. For this reason, the organophosphorus compounds are referred to as irreversible anticholinesterases. They are extremely toxic and are used as insecticides (parathion, malathion) and chemical warfare agents (e.g. sarin). Malathion is used topically in the treatment of scabies and head lice.
Читать дальше
 ) produces its actions on various effector organs by activating muscarinic receptors(
) produces its actions on various effector organs by activating muscarinic receptors(  ). The effects of acetylcholine are usually excitatory, but an important exception is the heart, which receives inhibitory cholinergic fibres from the vagus ( Chapter 17). Drugs that mimic the effects of acetylcholine are called cholinomimeticsand can be divided into two groups:
). The effects of acetylcholine are usually excitatory, but an important exception is the heart, which receives inhibitory cholinergic fibres from the vagus ( Chapter 17). Drugs that mimic the effects of acetylcholine are called cholinomimeticsand can be divided into two groups: ) can be stimulated by nicotinic agonists (top middle) or blocked by drugs that act specifically on the ganglionic neurone nicotinic receptor/ionophore (middle). Nicotinic agonists are of no clinical use and ganglion blocking drugs, e.g. hexamethonium, are only of historical interest.
) can be stimulated by nicotinic agonists (top middle) or blocked by drugs that act specifically on the ganglionic neurone nicotinic receptor/ionophore (middle). Nicotinic agonists are of no clinical use and ganglion blocking drugs, e.g. hexamethonium, are only of historical interest.