Clinical Signs and Signalment
Historically, the most common presenting signs for dogs with PCE have been weakness, collapse, and labored breathing (Stafford Johnson et al. 2004; MacDonald et al. 2009; Lisciandro 2016a); however, more recently a study documented that approximately 50% of dogs had a history of vomiting within 48 hours of presentation (Fahey et al. 2017). This finding, from the author's experience, argues for performing a Global FAST prior to a complete detailed abdominal ultrasound not only for ordering the indicated ultrasound study but also for the safety of the patient. Placing a patient with PCE into dorsal recumbency risks acute decompensation. Golden retrievers are the most common breed reported and in one study comprised 33% of the case study population, followed by German shepherds and other large breeds (Stafford Johnson et al. 2004; Fahey et al. 2017). In another study, gastrointestinal signs were reported in 16% of canine cases of PCE (Stafford Johnson et al. 2004).
Changes in the Paradigm – Recognizing Acute Pericardial Effusion
We are recognizing a new patient subset, the acute PCE case, with an unremarkable cardiac silhouette and respiratory distress, and a likely cardiac chamber rupture as the contributing factor. Traditional signs of muffled heart sounds, pulsus paradoxicus, electrical alternans on electrocardiogram, and a globoid heart on thoracic radiography are insensitive even in the chronic PCE case, let alone the acutely collapsed respiratory distressed case (Stafford Johnson et al. 2004; MacDonald et al. 2009; Guglielmini et al. 2012; Côté et al. 2013). Moreover, treatment strategies differ, as does the success of pericardiocentesis and definitive treatment. For example, if a cardiac chamber has acutely ruptured because of a right atrial mass, then the PCE may return in minutes to hours with repeated cardiac tamponade and obstructive shock. The case of a right atrial mass from hemangiosarcoma is a strong argument for the Global FAST approach, and rapidly staging the patient within minutes of presentation. Metastatic rate is high, 50–66% in one study (MacDonald et al. 2009).
Global FAST screens for hemoabdomen and lung metastasis, because if the patient is staged as isolated disease, then surgical removal of the cardiac tumor may be effective. The insertion of an indwelling pericardial catheter and autotransfusion(s) may be your only effective option (much different from traditional teaching paradigms). Moreover, performing a rough pericardiocentesis and opening the pericardial sac as a temporary pericardial window, used as a cheap, quick option in the past, will backfire with the patient then exsanguinating into an even larger space, the pleural cavity.
Pericardiocentesis Becomes a Core Skill
Veterinarians need to acquire pericardiocentesis as part of their skill set to save these patients (both canine and feline). Pericardiocentesis is not a difficult procedure and is discussed in detail in Chapters 21and 43. You have nothing to lose and everything to gain if a patient is dying from its PCE and complications are acceptable (Humm et al. 2009).
Use of TFAST for Accurate Diagnosis of Pericardial Effusion
See Chapters 17and 18.
Use of the DH View and TFAST for Accurate Diagnosis of Pleural Effusion
See Chapters 17and 18.
Use of the DH View and Vet BLUE for Deep Lung Lesions
See Chapters 22and 23for more detail. However, it is important to appreciate that the DH view serves as a deep window into lung pathology along its diaphragmatic interface (see Figures 6.14and 23.21).
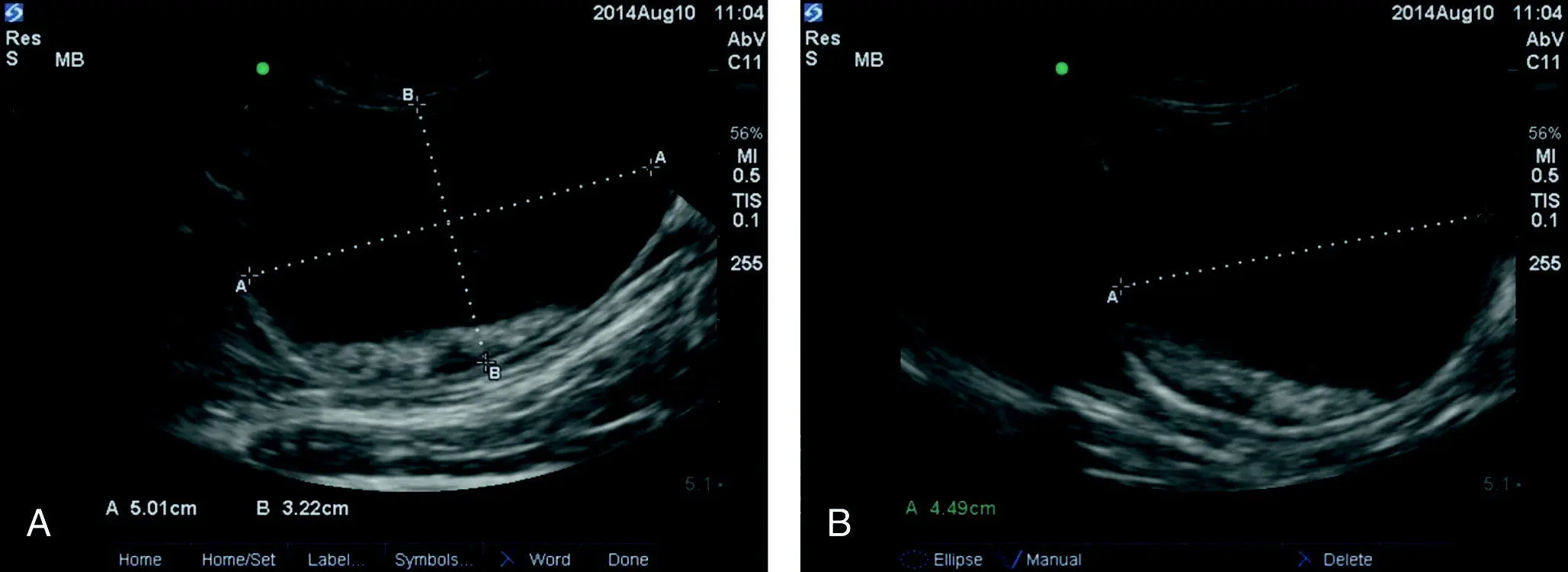
AFAST Cysto‐Colic View Formula for Urinary Bladder Volume Estimation
The use of the CC view formula of length × height × width (cm) × 0.625 = estimation of urinary bladder volume (mL) (Lisciandro and Fosgate 2017) serves as a rapid noninvasive way in which to estimate urinary bladder volume and, with serial measurements over time, provides a noninvasive means to estimate urine production. Moreover, walking dogs and allowing them to void, then confirming an empty urinary bladder with AFAST, is another way to effectively measure urine output in the hospitalized setting.
Make your best oval in longitudinal orientation of the bladder and acquire length and height in centimeters (cm).
Rotate the probe into transverse orientation and make your best largest oval and measure width (cm) ( Figure 7.15).
Calculate urinary bladder volume using length × height × width (cm) × 0.625 = estimation of urinary bladder volume (mL) (see Figure 7.15).
Urine output is estimated using change in urinary bladder volume/time.
AFAST and Its Target Organ Approach
AFAST was never meant to be a “flash exam” of the abdomen. The “flash” mentality is a quick ultrasound sweep answering a single binary question of whether fluid is present or absent, a positive or negative test. It is often used as a desultory sweep for a midabdominal mass, but without standardization of views and knowledge of anatomy at specific acoustic windows as in AFAST. Without direction, it becomes easy for the sonographer to get lost. Easily detected soft tissue conditions are often missed by abdominal radiography ( Table 7.9) and the reader is referred to Chapters 8– 12. The objective is through repetition and standardization to be able to tell normal from abnormal (differentiate expected from unexpected) and capture conditions that would otherwise be missed without any imaging or with radiography. As you read through Table 7.9, think about the conditions listed and how often they are missed on plain radiography. Interestingly, incidental findings during FAST exams have been reported in people (Sgourakis et al. 2012).
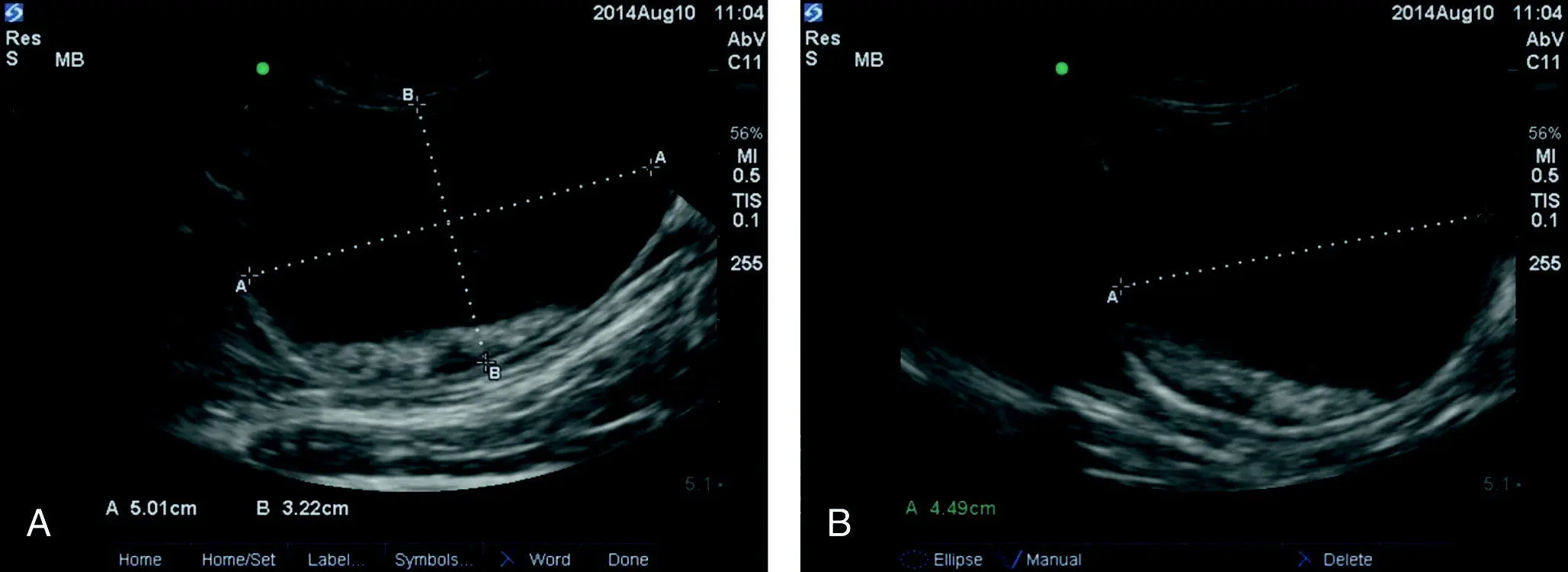
Figure 7.15. Measurements at the AFAST CC view for estimating urinary bladder volume. In (A) the best largest oval in the longitudinal plane is used for length (L, cm) and height (H, cm) measured as 5.01 cm and 3.22 cm, respectively. In (B) the best largest oval in the transverse plane is used for width (W, cm) measured as 4.49 cm. With these measurements the equation would be 5.01 × 3.22 × 4.49 cm × 0.625 = 45.3 mL. The volume can be compared to that aspirated when patients are catheterized immediately thereafter to gain confidence in its use (Lisciandro and Fosgate 2017).
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
Table 7.9. AFAST and its target organ approach as a soft tissue screening test.
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
| View |
Target organ |
Findings |
| DH |
Gallbladder |
SludgeMucoceleCalculiMasses |
|
Liver |
MassesObvious mottled echogenicity |
|
Caudal vena cava |
Caudal caval size abnormalitiesCaval syndromeHepatic venous congestion |
|
Lung |
Alveolar‐interstitial edema (B‐lines)ConsolidationMasses |
|
Heart |
Pericardial effusionLeft atrial enlargement |
|
Thorax |
Pleural effusionMasses |
| SR, HR, SR5th, HR5th |
KidneyLiver |
PyelectasiaHydronephrosisCortical cyst(s)Perinephric cyst(s)Polycystic diseaseMassesSee DH view |
| CC |
Urinary bladder |
SedimentCalculiBladder wall irregularitiesMasses |
| HRU, SRU |
Spleen |
MassesObvious mottled echogenicityMidabdominal masses |
See respective POCUS abdomen‐related chapters for examples.
Читать дальше