Table 1-1 Correlation between HbA1c and mean plasma glucose29
Those whose diabetes is poorly controlled will have elevated blood sugar, or hyperglycemia , and could be adversely affected by the stress of a dental appointment. Hypoglycemia (low blood sugar) can also cause problems. A controlled diabetic (on medication) who has missed a meal or has not eaten for several hours may become sweaty, lightheaded, and disoriented. These patients usually carry some quick source of glucose, such as candy, which should be administered. Four ounces of a regular soft drink or fruit juice or several pieces of hard candy should help them recover quickly. Treatment should be halted for that appointment, and the patient should be monitored at the office until complete recovery can be confirmed. It would be wise to have a family member drive the patient home. Dental treatment for the diabetic patient should interfere as little as possible with the patient’s dietary routine, and the patient’s stress level should be reduced. Any questions about the patient’s ability to cope with dental treatment and whether he or she is properly controlled should be referred to the patient’s physician before proceeding.
The prolonged presence of xerostomia , or dry mouth, is conducive to greater carious activity and is therefore extremely hostile to the margins of cast metal or ceramic restorations. Xerostomia can be caused by large doses of radiation in the oral region, 31lupus erythematosus, 22,32or Sjogren syndrome, an autoimmune disease. 33Sjogren syndrome frequently is first noticed and diagnosed by a dentist because of the xerostomia. 34It is frequently seen in conjunction with other autoimmune diseases, such as rheumatoid arthritis, lupus erythematosus, and scleroderma. 33
There are approximately 400 drugs capable of producing mild to severe xerostomia. 3,35Anticholinergics, anorectics, and antihypertensives may produce this effect. Antihistamines comprise the largest group of such drugs, and chronic allergy sufferers who use them over a prolonged time may suffer from dry mouth.
A relatively new problem that has arisen in relation to drug side effects and dental treatment is bisphosphonate-related osteonecrosis of the jaws (BRONJ). There is some controversy regarding the etiology and pervasiveness of this condition. Over the past 7 years, more than 4,000 cases have been reported to the Food and Drug Administration. 36This family of drugs is administered intravenously (IV) to treat metastatic bone cancer, and the greatest risk of osteonecrosis occurs in these patients. Bisphosphonates are used more widely, but at lower dosage levels, as an oral preventive treatment for osteoporosis. The ratio of patients on oral bisphosphonate therapy who have developed osteonecrosis compared with those on the IV drug has varied from 10% 37to as high as 83%. 38
Osteonecrosis was initially associated with oral surgery, but there have been reports of spontaneous occurrences without surgery at rates as high as 25%. 39,40Scully et al 41have stated that bisphosphonate therapy is a contraindication for dental endosseous implants, and at the present time, Marx et al 39strongly discourage implant placement in patients taking bisphosphonates.
Current complaint and patient expectations
As part of the health history, the patient should be given an opportunity to describe the exact nature of the complaint that has brought him or her to the dental office for treatment. Attitudes about previous treatment and the dentists who have rendered it offer insight into the patient’s level of dental awareness and the quality of care expected. This will help the dentist to determine how much education the patient will require and how amenable the patient will be to cooperating with a good home-care program. Moreover, an effort should be made to get an accurate description of the patient’s expectations for the treatment results. Particular attention should be paid to the esthetic effect anticipated. A judgment must be made as to whether the patient’s desires are compatible with sound restorative procedures. Possible conflicts in this area, as well as in the realm of personality, should be noted. The option of not providing care may need to be exercised with some patients.
TMJ and occlusal evaluation
Prior to the start of fixed prosthodontics procedures, the patient’s occlusion and TMJs must be evaluated to determine if they are healthy enough to allow the fabrication of restorations. If the occlusion and TMJs are within normal limits, then treatment should be designed to maintain that relationship. However, if the occlusion or one or both TMJs are dysfunctional in some manner, further appraisal is necessary to determine determine whether the dysfunction can be improved prior to the placement of the restorations or if restorations should not be placed.
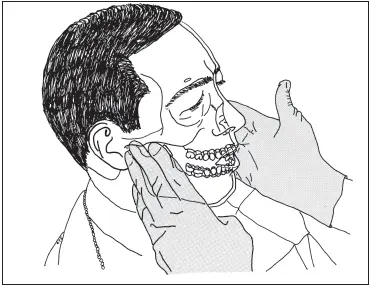
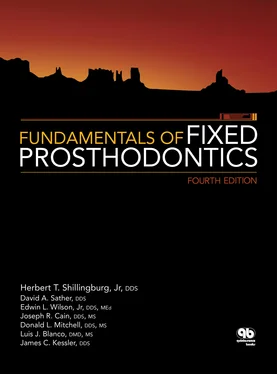
Fig 1-7The joints are palpated as the patient opens and closes to detect signs of dysfunction.
Does the patient suffer from frequent occasions of head, neck, or shoulder pain? If so, an attempt must be made to determine the origin of such pain. It may be referred pain , ie, it may not originate from the area where the pain is experienced. 42Many patients suffer from undiagnosed muscle and/or joint dysfunction of the head and neck region; such a history should be investigated further.
Next, an assessment of the TMJs themselves should be performed. Healthy TMJs function with no evidence of pain. Asymptomatic clicking or crepitation occurs in about one-third of the general population. 43Limitation of movement on opening, closing, or moving laterally should be investigated further to determine the condition of the TMJs. Palpation of the joints as the patient opens and closes should reveal the existence of any signs of dysfunction ( Fig 1-7). Many patients suffer from muscle pain as a result of parafunctional jaw activity related to stress. Habits such as clenching the teeth and manipulating the bite during the course of the daily routine may result in fatigue and muscle pain. The physical appearance and activities of the patient should be observed for signs of such habits. Many times they will have a squarejowled appearance, with masseter muscles that are overdeveloped from hyperactivity. They may even clench their teeth during the patient interview.
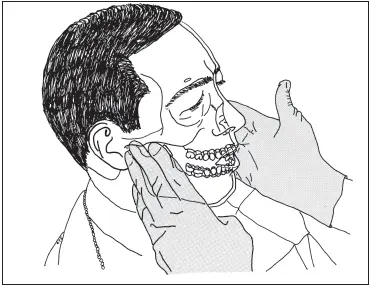
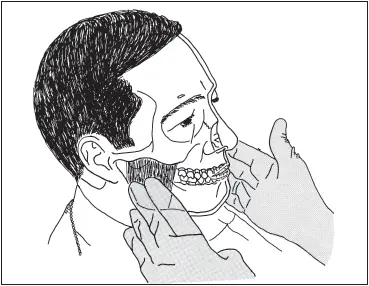
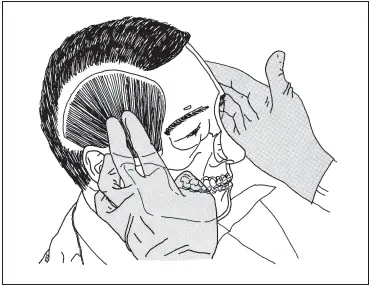
A brief palpation of the masseter ( Fig 1-8), temporalis ( Fig 1-9), medial pterygoid ( Fig 1-10), trapezius ( Fig 1-11), and sternocleidomastoid ( Fig 1-12) muscles may reveal tenderness. The patient may demonstrate limited opening due to tightness of the masseter, temporalis, and/or medial pterygoid muscles. This can be noted by asking the patient to open “all the way” ( Fig 1-13). If it appears that the opening is limited or the movement is slowed, ask the patient to point to the area that hurts ( Fig 1-14). If the patient touches a muscle area, as opposed to the TMJ, there is probably some dysfunction of the neuromuscular system. Patients experiencing a problem with one or both TMJs will most frequency point to the joint itself.
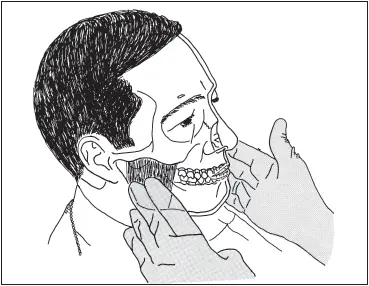
Fig 1-8The masseter muscles are palpated extraorally by placing the fingers over the lateral surfaces of the rami of the mandible.
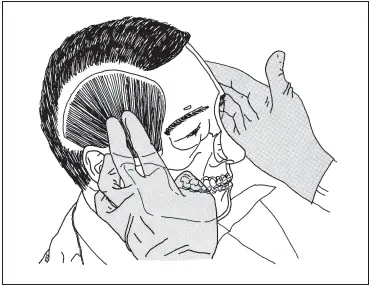
Fig 1-9The fingers are placed over the patient’s temples to feel the temporalis muscles.
Читать дальше