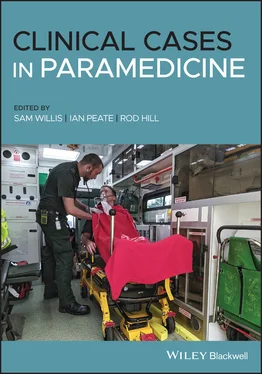
You decide to move your patient to the back of the ambulance to continue the examination in a warm and private environment. On standing, the patient complains of feeling dizzy and faint and is unable to walk even a couple of steps. You instruct your crewmate to fetch the carry chair as you can’t get the stretcher close enough to the patient.
Patient assessment triangle
General appearance
Patient feels better when lying flat.
Normal.
Increased. Patient complains of not being able to ‘catch her breath’.
SYSTEMATIC APPROACH
Danger
None at this time.
Alert.
Clear.
RR: 30.
HR: 128. Weak radial.
Moving all four limbs.
Normal temperature in the ambulance.
RR: 30 bpm
HR: 128 bpm
BP: 88/60 mmHg
SpO 2: unable to obtain
Blood glucose: not repeated
Temperature: not repeated
GCS: 15/15
12 lead ECG: sinus tachycardia with right bundle branch block (RBBB)
1 What is the most common ECG finding in PE? What other ECG changes are associated with PE? The most common ECG finding in PE is sinus tachycardia. PE can cause any of the following ECG changes:T‐wave inversion.New‐onset atrial fibrillation.Right bundle branch block.Right axis deviation.S1Q3T3 (this is a specific pattern that is seen rarely in PE):S waves in lead I.Q waves in lead III.T‐wave inversion in lead III.
2 Explain why females taking the oral contraceptive pill are at greater risk of developing a PE. Virchow’s triad explains the three broad categories that play a part in thrombus formation: Hypercoagulability. Hemodynamicchanges (stasis, turbulence). Endothelialinjury/dysfunction.Taking contraceptive drugs that contain oestrogen can actually change the constitution of the blood, increasing plasma and other clotting factors. This causes the woman to be in a hypercoagulative state, increasing the risk of developing DVT/PE.
LEVEL 2 CASE STUDY
Life‐threatening asthma
| Information type |
Data |
| Time of origin |
07:13 |
| Time of dispatch |
07:15 |
| On‐scene time |
07:26 |
| Day of the week |
Monday |
| Nearest hospital |
20 minutes |
| Nearest backup |
10 minutes |
| Patient details |
Name: Billy Bob DOB: 01/06/1995 |
You have been called to a residential address for a 25‐year‐old male with difficulty in breathing. Caller states he has been breathless all night and has had a cough recently.
The patient is conscious and breathing and is located in a third‐floor flat/unit – there is no lift.
The location appears safe and you are greeted at the communal entrance by the patient’s partner.
The partner appears agitated and hurries you up the stairs, stating that the patient was having his breakfast and his breathlessness got a lot worse.
On arrival with the patient
The patient is sat leaning forward and appears panicked. He does not say hello when you introduce yourself and states repeatedly that he cannot breathe, in short sharp breaths.
Patient assessment triangle
General appearance
Alert, but does not acknowledge your presence. Acutely distressed. Unable to speak in full sentences, leaning forward with clear dyspnoea.
Pale and peripherally cyanosed.
He has increased breathing effort and only giving 1 word answers.
SYSTEMATIC APPROACH
Danger
None at this time.
Alert.
Clear.
RR: 32. Rapid and shallow. No accessory muscle use. Minimal air movement bilaterally on auscultation.
HR: 130. Radial weak and barely palpable, regular. Capillary refill time 3 seconds. Nail beds appear bluish.
Pupils equal and reactive to light (PEARL) – 5 mm.
The chest is exposed to conduct an assessment. The patient is in a private residence and the unit has a warm temperature.
RR: 32 bpm
HR: 130 bpm
BP: 100/54 mmHg
SpO 2: 87%
Blood glucose: 4.3 mmol/L
Temperature: 37.2 °C
Peak expiratory flow reading (PEFR): unable to record
GCS: E4, Verbal – not complying with your questioning, only stating he cannot breathe, M6
4 Lead ECG: sinus tachycardia, regular
Allergies: nil
Look through the information provided in this case study and highlight all of the information that might concern you as a paramedic.
Using the latest guidelines from the Australia and New Zealand Thoracic Society (ANZTS), the British Thoracic Society (BTS) or a source that draws on these resources, compare and contrast the differences between life‐threatening asthma and anaphylaxis, and explain why this is more likely to be asthma than any other differential diagnosis.
Similarities: asthma and anaphylaxis both present with respiratory distress and a wheeze. Both are due to an inflammatory response. And both may appear flushed – from exertion in asthma, and in anaphylaxis the skin’s reaction to the allergen.
Differences: in anaphylaxis the whole airway can be affected, producing particular symptoms not associated with asthma, such as voice changes, stridor, inspiratory wheeze and tongue and lip swelling. Also asthma is predominantly a respiratory problem, whereas anaphylaxis can present with gastrointestinal problems and hypotension, which can lead to distributive shock.
Although this did occur after eating, the patient seems to be presenting with symptoms limited purely to the respiratory system. There are no dermatological, gastrointestinal or cardiovascular changes that would indicate anaphylaxis.
1 Is this patient suffering from moderate, severe or life‐threatening asthma, and why? Life‐threatening asthma. See Table 1.4. Table 1.4 Comparison of asthma severitySource: British Thoracic Society (2019).Near‐fatal asthmaRaised PaCO2 and/or requiring mechanical ventilation with raised inflation pressuresLife‐threatening asthmaIn a patient with severe asthma any one of: PEF <33% best or predicted SpO2 <92% PaO2 <8 Kpa ‘Normal’ PaCO2 (4.6–6.0 Kpa) Altered conscious level Exhaustion Arrhythmia Hypotension Cyanosis Silent chest Poor respiratory effortAcute severe asthmaAny one of: PEF 33–50% best or predicted Respiratory rate ≥25/min Heart rate ≥110/min Inability to complete sentences in one breathModerate acute asthmaIncreasing symptoms PEF >50–75% best or predicted No features of acute severe asthma
1 List your treatment, route and dosages. Adrenaline – 500 μg IM.Salbutamol – 5 mg nebulised.Ipatropium bromide – 500 μg nebulised.Oxygen – 6/8 L.Hydrocortisone – 100 mg IV (IM possible if unable to gain IV access).
Читать дальше