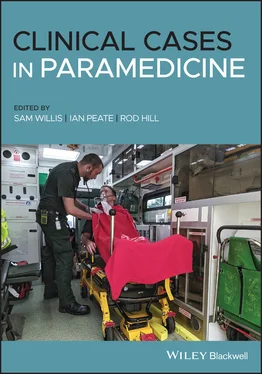
You treat this patient rapidly with 500 μg of intramuscular (IM) adrenaline while your crewmate administers 5 mg of salbutamol and ipratropium bromide via a nebulizer, on 6 L of oxygen. After nebuliser therapy and 1 dose of IM Adrenaline, you rapidly extricate your patient to the ambulance. You deliver a pre‐alert to the nearest emergency department.
Patient assessment triangle
General appearance
Alert and now looking at you and nodding or shaking his head in response to your questions.
Pale.
Increased work of breathing – breathing still rapid, but less shallow.
SYSTEMATIC APPROACH
Danger
None at this time.
Alert.
Clear and peripherally cyanosed.
RR:28. Audible wheeze on auscultation.
HR: 128. Palpable radial. Capillary refill time 2 seconds. Nail beds appear bluish.
Moving all four limbs.
Normal temperature in the ambulance.
RR: 28 bpm
HR: 128 bpm
BP: 110/78 mmHg
SpO 2: 91%
Blood glucose: not repeated
Temperature: not repeated
GCS: 15/15
4 lead ECG: sinus tachycardia
1 This type of incident may lead to high levels of stress during the time you are with the patient. Name at least four short‐term effects of stress. Increased heart rateIncreased blood pressurePupil dilationSweatingIncreased blood sugar levelsInhibitions of digestive secretionsPeripheral vasoconstrictionBronchodilationSource: ANZ (2015).
2 It is important to recognise symptoms of long‐term (chronic) stress in yourself or others. Name at least two long‐term effects of stress. Behaviour changes:Difficulty sleeping.Altered eating habits.Smoking/drinking more.Avoiding friends and family.Sexual problems.Physical responses:Tiredness.Indigestion and nausea.Headaches.Aching muscles.Palpitations.Mental responses:Increased indecision.Difficulty concentrating.Poor memory.Feeling inadequate.Low self‐esteem.Emotional responses:Mood swings, becoming irritable or angry.Increased anxiety.Feeling numb.Hypersensitivity.Feeling drained and listless.Source: Ambulance care practice (2019).
LEVEL 3 CASE STUDY
Respiratory sepsis
| Information type |
Data |
| Time of origin |
09:15 |
| Time of dispatch |
09:30 |
| On‐scene time |
09:43 |
| Day of the week |
Sunday |
| Nearest hospital |
20 minutes |
| Nearest backup |
40 minutes |
| Patient details |
Name: Nicholas Beaumont DOB: 01/01/1947 |
You have been called to a residential address for a 73‐year‐old male complaining of weakness and shortness of breath.
Patient is conscious and breathing. Upstairs in bed.
The scene is safe. You are met at the door by the patient’s wife.
The wife tells you her husband has had a productive cough for 3 days and is now unable to get out of bed.
On arrival with the patient
The patient is lying in bed and appears lethargic.
Patient assessment triangle
General appearance
Alert but lethargic.
Flushed, warm to touch and clammy.
Increased work of breathing.
SYSTEMATIC APPROACH
Danger
None at this time.
Alert on the AVPU scale.
Clear.
RR: 34. Rapid. Mild accessory muscle use. Right basal crackles on auscultation.
HR: 130. Radial palpable but weak – regular. Capillary refill time 3 seconds.
Pupils equal and reactive to light (PEARL).
The patient is in his own bed and the ambient temperature is warm.
RR: 34 bpm
HR: 130 bpm
BP: 108/54 mmHg
SpO 2: 87%
Blood glucose: 8.3 mmol/L
Temperature: 38.4 °C
GCS: 15/15
4 lead ECG: sinus tachycardia
Allergies: nil
Look through the information provided in this case study and highlight all of the information that might concern you as a paramedic.
You administer high‐flow oxygen titrated to maintain an SpO 2of 94–98%. Fluid is not indicated at this time and your local guidelines do not allow for the administration of prehospital antibiotics. You commence rapid transport to the Emergency Department with a sepsis pre‐alert.
Patient assessment triangle
General appearance
Alert.
Flushed.
Increased work of breathing.
SYSTEMATIC APPROACH
Danger
None at this time.
Alert.
Clear.
RR: 30. Right basal crackles.
HR: 126. Weak radial. Capillary refill time 3 seconds.
Moving all four limbs.
Normal temperature in the ambulance. Patient covered with sheet not blanket to assist with ambient cooling.
RR: 30 bpm
HR: 126 bpm
BP: 100/58 mmHg
SpO 2: 90%
Blood glucose: not repeated
Temperature: 38.3 °C
GCS: 15/15
4 lead ECG: sinus tachycardia
1 What is sepsis? ‘Sepsis is characterised by a life‐threatening organ dysfunction due to a dysregulated host response to infection’ (UKST, 2019, p. 14).
2 Outline the pathophysiology of sepsis. Sepsis is when the body’s natural inflammatory immune response to a localised infection becomes systemic, setting off a chain of physiological responses that quickly become life‐threatening. It is an exaggerated response involving both the complement system (immune response) and the coagulation cascades.The body tries to keep up with the increased demand for oxygen by raising the respiratory rate (RR) to increase the level of oxygen in the blood and to oxygenate the extra blood flow through the lungs. The heart rate (HR) and stroke volume (SV) are raised, leading to an increased cardiac output (CO). Vasodilation occurs, allowing the blood vessels to transport a greater blood volume, which eventually leads to reduced preload and reduced SV. The HR increases further to compensate, resulting in tachycardia. Some patients may be on medications that mask tachycardia (e.g. betablockers).Profound vasodilation leads to a ‘relative loss’ in circulating volume and the increased permeability of the blood vessels following the release of histamine results in an ‘absolute loss’ as fluid escapes into the extravascular space. 25% of patients with septic shock present with a normal BP (cryptic shock or occult hypoperfusion) and others may present with relative hypotension (systolic BP >40 mmHg lower than normal systolic BP).In the early stages patients may be warm and flushed as vasodilation leads to an increased blood volume in the peripheries. Heat generated soon becomes lost through the skin, reducing the temperature. In the later stages, the patient begins to peripherally shut down as the body attempts to redirect the blood to its core organs, which results in a further cooling of the skin. Hypothermia/cold sepsis occurs in 10–20% of patients and is more common in elderly patients. The mortality rate for these patients is double that of those with pyrexia.
Читать дальше