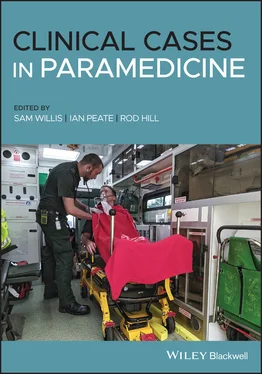
On arrival with the patient
The male patient has been moved to the floor, where the son is performing good‐quality CPR. You note the patient has significant swollen lower peripheries and scratch marks on his lower limbs.
Patient assessment triangle
General appearance
The patient is unresponsive, lying on the floor.
Pale in colour, cool to touch.
The patient does not appear to be breathing.
SYSTEMATIC APPROACH
Danger
Nil.
No response.
Vomit in the airway.
Nil.
No pulse.
Look through the information provided in this case study and highlight all of the information that might concern you as a paramedic.
1 Think about the location you have been dispatched to. Discuss, as you would with your partner, what actions you may take to ensure your safety prior to arriving on scene.Often we attend areas where police assistance is required for our safety. Discussion should include early activation of police (if this has not already been arranged), staging prior to arrival and awaiting police attendance to ensure scene safety, utilising prior history you or comms have on the location, parking your vehicle in a position that would allow for a quick egress if required (this may involve backing into a driveway or ensuring you are not facing a dead‐end street), identifying risks as they arise and using your ‘gut instinct’ to assess the scene. These are just a few to mention. Utilise other paramedics’ experiences to gain knowledge into how others approach these scenes.
Case Progression
History taking
You ask the patient’s partner what has occurred and she does not directly respond to your questions, continually yelling ‘Fix him, fix him, hurry up and do something to fix him’. She is visibly distressed and emotional despite your attempts to calm her.
What must you do in this situation where an accurate/thorough history cannot be gained quickly from the patient’s partner due to her emotive state? Discuss/write down what options you have.
Consider the utilisation of others on scene – the patient’s son may be of benefit and could possibly be a source of information. Other family members or neighbours who are present may assist with information and/or reassurance to the patient’s wife.
Look for other information on scene such as medications, doctor’s letters, medical aids or medical bracelets. You notice leftover boxes of dialysis solution in the hallway as you walk in – what does this tell you?
Case Progression
History taking (cont.)
The son states that the patient has not been well lately. His medical history includes diabetes, hypertension, hypercholesterolemia and end‐stage renal failure. They used to use home dialysis, but for the last two months he has had to go to hospital as his condition has worsened. For the last week he has not been to the hospital as he has been too unwell and hates hospitals. Last night he was not well and had a restless sleep. He said his heart was racing, but didn't tell anyone until this morning. He has been in bed since as he told them his muscles were aching and tingling. When they checked on him they found him unconscious with vomit in the bed.
1 Describe your primary survey for this patient.Danger: No danger.Response: None.Circulation: No pulse, commence CPR and remove any clothing on patient’s thorax area and place the defibrillation pads and analyse rhythm, shock if advised.Airway: vomit is present, requires suctioning that clears airway.Breathing: No breaths.
2 Describe how you would manage your crew and others on scene. What roles would you allocate and would an early sit rep be of benefit?As lead paramedic you should allocate roles and ensure they are maintained. As airway clinician you should assist with removal of clothing and placement of the defibrillation pads onto the patient’s chest to ensure quick automatic analysis of the rhythm. The son is performing quality compressions, so asking him to assist and continue would be appropriate if he is willing. Compressions can then be managed by your partner.The airway then needs to be cleared with suctioning and a correctly sized OPA placed (describe your sizing technique). Then you need to ensure the ratio of 30 compressions to every 2 breaths is maintained and the rate is between 100 and 120 bpm, with appropriate compression depth (1/3 of chest wall). Rhythm checks completed every 2 minutes.An early sit rep is vital in any high‐acuity case. In this case a request for another crew to assist with resuscitation would be appropriate, as would a request for an intensive care paramedic.
You continue your resuscitation to plan and there is no change in the patient’s condition despite defibrillating the patient three times. You are coming up to 6 minutes.
Patient assessment triangle
General appearance
Patient is unresponsive.
Pale in colour.
Nil.
SYSTEMATIC APPROACH
Danger
Nil.
None.
Clear.
Nil intrinsic.
Ventricular tachycardia at a rate of 180 bpm (after three shocks delivered).
Defibrillation pads: Ventricular tachycardia at a rate of 180 bpm
RR: 0
BP: Unrecordable
SpO 2: Unrecordable
Blood glucose: 16.2 mmol/L
GCS: 3/15
Pupils: Size 3, reactive
Colour/appearance: Pale
Respiratory effort/rhythm: No effort
Pulses: Absent
Head to toe: Reveals nil obvious injuries/deformities, nil medical alerts
1 Discuss other interventions that could be considered after 6 minutes.Other interventions include gaining IV or IO access and adrenaline administration (after second unsuccessful shock) every 3–5 minutes. The placement of an advanced airway should not interrupt CPR, with waveform capnography being considered.
2 List the reversible causes of cardiac arrests. Taking into account the history, what is the reversible cause that is most likely to be causing the patient’s condition and what additional treatment could be considered? (Think of a higher scope of practice.)Cardiac arrest caused by hyperkalemia is most likely. Other reversible causes (see Table 2.4) include a build‐up of potassium, which can cause suppression of electrical activity of the heart and can cause the heart to stop beating. This patient has renal failure and has missed his dialysis appointments, indicating that this is the likely cause. To treat a suspected hyperkalemia we need to shift the potassium back into the cell and protect the myocardium. This is achieved by administering calcium gluconate, which will stabilise the myocardium. Sodium bicarbonate 8.4% should be considered as a buffer to treat the metabolic acidosis. These interventions often require the presence of critical care paramedics, so early identification and activation are vital and it helps to think ahead.
Table 2.4 The 4 Hs and 4Ts – reversible causes of cardiac arrest
| Hypoxia |
Tension pneumothorax |
| Hypovolemia |
Cardiac tamponade |
| Hyper/hypokalemia/metabolic causes |
Thrombus |
| Hyper/hypothermia |
Toxins |
Читать дальше