You have been called to a public address for a 38‐year‐old male who was witnessed to be running along a footpath when he suddenly collapsed.
The patient is now conscious and breathing, complaining of palpitations and shortness of breath (SOB).
On arrival on scene, the patient is found to be lying supine on the footpath with three bystanders standing around him. The scene appears safe to approach and the patient seems to be alert.
On arrival with the patient
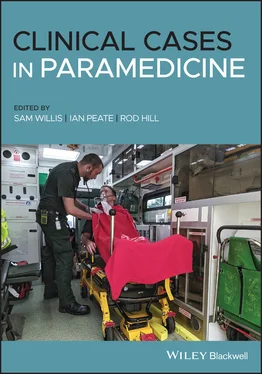
You remove yourself from the ambulance, acquire the oxygen and airway kit, primary response kit (drug kit) and defibrillation monitor, and undertake an observational assessment. After identifying the patient has no physical injuries, you place him on the ambulance stretcher and remove him to the ambulance to maintain confidentiality. You are greeted by a female who states she is an off‐duty Registered Nurse and advises how the patient was witnessed to be jogging along the footpath and suddenly ‘collapsed’ or ‘fell’. The patient was unresponsive for 1 minute before regaining consciousness and was placed in the recovery position.
Patient assessment triangle
General appearance
The patient is alert and he looks at you as you approach. The patient was lying in the right lateral position prior to placing him on the ambulance stretcher. The patient is pale and clammy, but is able to speak in full sentences.
Slightly pale and clammy.
Nil increased work of breathing, air entry = L/R clear, nil adventitious sounds.
SYSTEMATIC APPROACH
Danger
You are in a public place, you observe bystanders, but the scene appears safe to proceed.
The patient is alert on the AVPU scale. He looks at you and acknowledges you as you approach. Patient says hello after you introduce yourself and partner.
The airway is clear. The patient is able to speak in full sentences. Nil blood or secretions coming from airway.
There is breathing with spontaneous effort, equal rise and fall of chest with asymmetry, nil DIB, respiratory rate 22 respirations per minute – adequate ventilation.
The circulation is weak with regular palpable radial pulses, nil obvious signs of haemorrhage and nil C‐spine pain on palpation, with nil report of focal neurological deficits (nil paraesthesia reported).
Nil evidence of trauma on head‐to‐toe assessment, patient able to move all limbs freely, nil evidence of head strike. Nil obvious bleeding. Patient states 0/10 pain, but says he has palpitations/fluttery feeling in his chest.
RR: 22 bpm
HR: 180 bpm
BP: 90/68 mmHg
SpO 2: 97%
Blood glucose: 5.0 mmol/L
Temperature: 36.3 °C
12 lead ECG: Narrow complex tachycardia with nil discernible P wave and nil apparent ST/T wave abnormalities
Look through the information provided in this case study and highlight all of the information that might concern you as a paramedic.
1 What are some differential diagnoses for this patient? (Consider both regular and irregular rhythms.)Regular: Physiological sinus tachycardia, inappropriate sinus tachycardia, sinus nodal re‐entrant tachycardia, focal atrial tachycardia, atrial flutter with fixed AV conduction, AV‐nodal reentrant tachycardia (AVNRT), orthodromic AVRT, idiopathic VT, Wolff–Parkinson–White syndrome.Irregular: Atrial fibrillation, focal atrial tachycardia or atrial flutter with varying AV block, multifocal atrial tachycardia (MATT).
1 What are your treatment priorities for this patient?The 12 lead ECG has become one of the most important prehospital diagnostic tools. In cases such as this where a patient has suddenly collapsed, an early 12 lead ECG is required. If the patient is haemodynamically stable, conduct modified Valsalva manoeuvres (vagal manoeuvres).
2 What is your plan if the patient begins to deteriorate?Request intensive care paramedic backup, prepare for synchronised cardioversion, position patient appropriately, oxygen if hypoperfused/hypoxemic, place defibrillation pads on patient, IV access, crystalloid fluids.
You manage to complete primary and secondary surveys, including early 12 lead ECG acquisition, which identifies a regular narrow complex tachycardia. The patient continues to complain of shortness of breath, palpitations and dizziness, but is haemodynamically stable and maintaining a perfusing blood pressure.
Patient assessment triangle
General appearance
Patient is alert and orientated, sitting upright and speaking in full sentences.
Well perfused, skin is pink, warm and dry.
Increased work of breathing noted, with increased respiratory effort. Nil intercostal recession or supraclavicular retractions seen, patient airway is patent and he is able to speak in full sentences.
SYSTEMATIC APPROACH
Danger
The scene is still safe.
Patient is alert and orientated.
The airway is clear. The patient is able to speak in full sentences. Nil blood or secretions coming from airway.
There is breathing with spontaneous effort, equal rise and fall of chest, nil DIB, respiratory rate 28 respirations per minute – adequate ventilation.
The circulation is weak with regular palpable radial pulses, nil obvious signs of haemorrhage.
Increased respiratory effort, but talking in full sentences – mild shortness of breath (dyspnoea).
1 What is your treatment goal for this patient now? What hospital would you ideally like to transport the patient to?To successfully revert patient into normal sinus rhythm, improving cardiac output and subsequent perfusion. This can be achieved by attempting vagal manoeuvres. Should this fail, transport to hospital for further medical care is required. It would be expected that the patient be transported to a hospital with a cardiac unit/cardiology capabilities.
2 What types of questions would you ask this patient as part of your history‐taking process?See Table 2.3.
Table 2.3 History‐taking questions
| Signs and symptoms: Rapid pulse, pale, clammy, increased work of breathing, complains of mild nausea, palpitations (fluttering feeling in chest) Allergies: NSAIDs Medications: Nil reported Previous medical history: Nil reported Last meal: Breakfast at 07:00 – oats Events leading up to today: Witnessed collapse while running, normal water intake |
| Additional questioningDoes the patient remember falling? If so, what caused the fall? Can the patient retain new information? Is there retrograde amnesia? Does the patient have a cardiac history (Hx)? What is your full name and DOB? Is there any family or emergency contact you’d like us to call? |
Despite two attempts at a modified Valsalva, the patient is now feeling short of breath, dizzy, nauseated, has chest pains and palpitations, and states he feels like he is going to pass out. You are unable to palpate a radial pulse and blood pressure is unrecordable.
Читать дальше