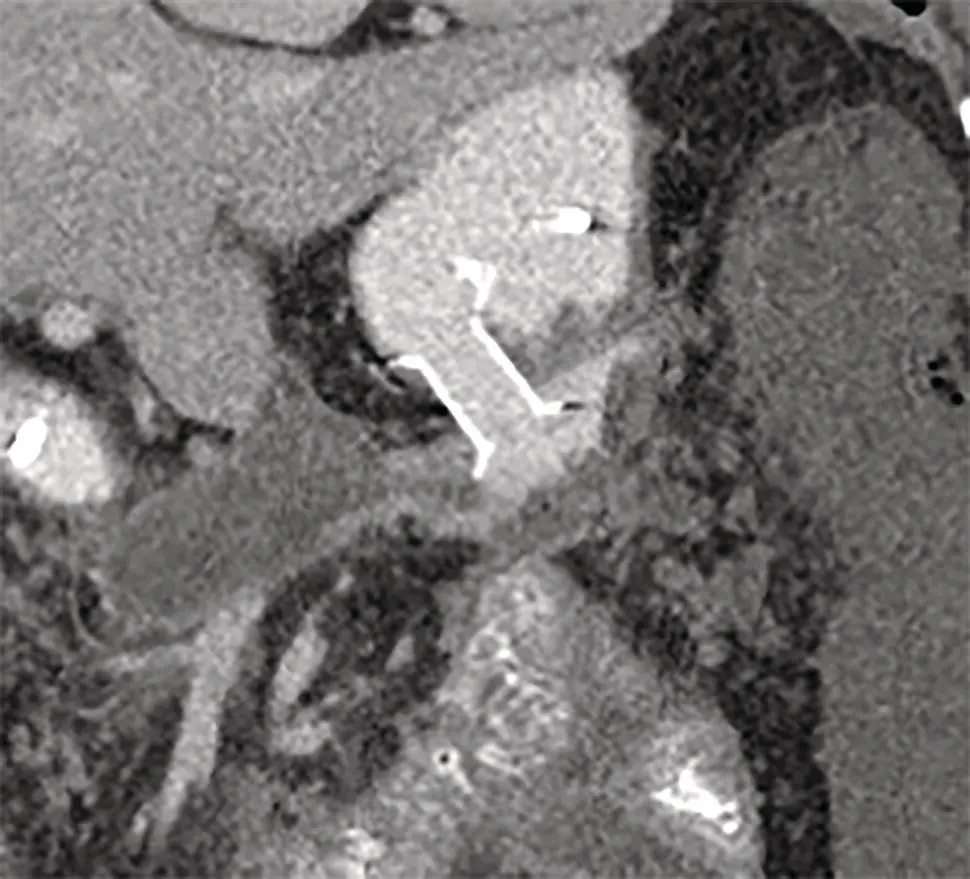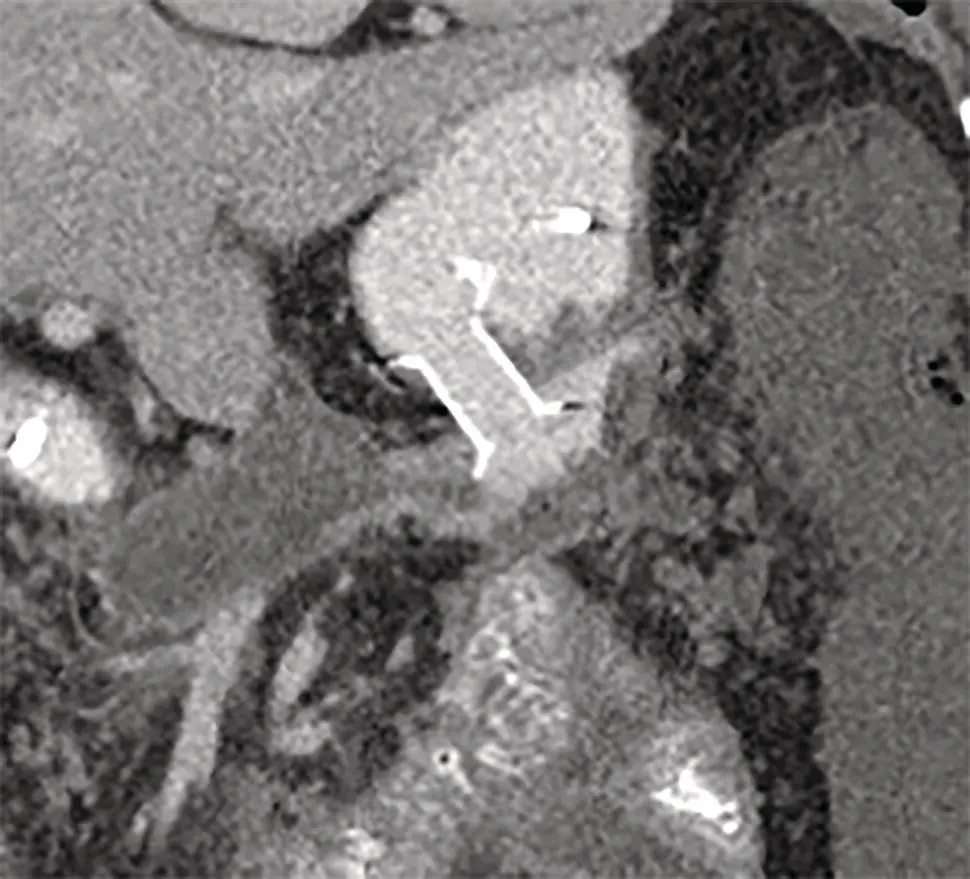
Figure 17.2 CT scan showing LAMS in situ .
Source: courtesy of Muhammad F. Dawwas and Kofi W. Oppong.
Transpapillary drainage of pancreatic pseudocysts by means of stent placement in the pancreatic duct is potentially feasible in the subgroup of patients with small to moderate‐sized pseudocysts that clearly communicate with the main pancreatic duct. In this setting, the pancreatic duct is cannulated via the major or minor papilla in the standard fashion and the disrupted segment of the duct is bridged with one, or preferably two, plastic stents after undertaking a pancreatic sphincterotomy. If this is not feasible, placement of the stent tip medial to the leak or within the pseudocyst may also be effective. In practice, however, transpapillary drainage is not recommended as sole drainage therapy for the majority of pancreatic pseudocysts for several reasons. First, given the fact that at least 50% of pancreatic pseudocysts develop in the absence of evidence of disruption of the main pancreatic duct, transpapillary stent placement in this setting would not be anticipated to facilitate effective drainage. Second, undertaking ERCP in the setting of extrinsic luminal compression of the gastroduodenal lumen and gross inflammation of the duodenal mucosa can be technically challenging, as would attempts to stent a disrupted duct lateral to an obstructing stone or high‐grade stricture. Third, preoperative evaluation of the integrity of the main pancreatic duct may not be feasible as a result of unavailability of a high‐quality secretin‐stimulated MRCP service. Last, the smaller diameter of both pancreatic stent and pancreatic duct, compared with the diameter of transluminal stents and fistula, may result in inadequate drainage, increasing the risk of infection in the setting of contrast contamination of an otherwise sterile pseudocyst.
Combined transluminal and transpapillary drainage is favored by many experts, although the evidence base supporting this practice is less than compelling. If ERCP is performed, the timing of the procedure is also controversial. Undertaking ERCP prior to transluminal pseudocyst drainage may be accompanied by multiple technical challenges as already outlined. On the other hand, delaying ERCP may potentially result in missing a valuable window of opportunity for stenting a potentially bridgeable pancreatic duct disruption that, in the absence of intervention, may evolve into a non‐traversable, high‐grade stricture or even a disconnected duct.
Disconnected Pancreatic Duct Syndrome
Disconnected pancreatic duct syndrome is a clinical entity characterized by recurrent pancreatitis and persistent extraductal leakage of pancreatic secretions from a disconnected pancreatic tail as a result of complete transection of the pancreatic duct, usually occurring in the setting of a severe episode of acute pancreatitis [14]. The syndrome complicates nearly two‐thirds of pancreatic necrotic collections and one‐third of other pancreatic fluid collections. The diagnosis can be made with varying degrees of accuracy by secretin‐stimulated MRCP, ERCP, EUS, and contrast‐enhanced CT. Successful management requires effective drainage of the disconnected pancreatic segment. If transluminal stent‐assisted drainage of the pseudocyst was undertaken, the most common approach is to maintain the cystenterostomy patent by keeping the transluminal stents in place indefinitely. This is one of the most compelling arguments for recommending the use of plastic over metal stents for transluminal drainage of pancreatic pseudocysts. Transpapillary stent placement into the disconnected duct segment is technically challenging but is not impossible and certainly worth trying. EUS‐guided transluminal placement of a plastic stent into the disconnected duct segment has also been described. Ultimately, if all endoscopic endeavors prove unsuccessful, surgical resection of the disconnected pancreatic segment or even total pancreatectomy with islet cell autotransplantation may be the only therapeutic option.
Complications related to endoscopic drainage occur in 5–25% of patients. Transluminal drainage is associated with bleeding, infection, and perforation. Cyst infection occurs independent of the size of the stent used and can even occur when the cavity appears to have completely drained at the time of stent insertion. Periprocedural antibiotics and for a few days after the procedure are therefore advocated, although there is no randomized controlled trial evidence to support their use [3–7]. Repeat imaging is indicated if infection persists or occurs some time after stenting to assess for stent dysfunction which may require further endoscopic intervention.
Significant bleeding at the time of stent placement is uncommon as the use of EUS guidance should prevent injury to significant vessels. Bleeding at the time of stent placement is usually short‐lived, venous, and from the transluminal tract. Massive bleeding at the time of stent placement is rare and may be due to a preexisting pseudoaneurysm, intra‐abdominal varices, or splenic or portal vein injury. Such massive bleeding is typically not amenable to endoscopic therapy and, when it occurs, resuscitation and the urgent assistance of an interventional radiologist or experienced surgeon is required. Late bleeding appears more common with LAMS [12]. LAMS can induce both neovascularization and overgrowth of adjacent retroperitoneal tissues leading to bleeding at the time of removal, hence the need for earlier retrieval than plastic stents. Additionally, collapse of the cyst cavity can bring vessels into contact with the metal flange leading to abrasion and late bleeding.
Perforation due to stent misplacement is uncommon with EUS guidance in expert hands. However, rapid decompression of a large collection (particularly if the wall is not fully mature and adherent) may lead to dehiscence of the cyst wall from the stomach or duodenum and a clinically significant leak. This is less likely when a LAMS is used. ERCP and transpapillary drainage is associated with the additional risk of pancreatitis.
Endoscopy is well established as an important tool in the armamentarium of the multidisciplinary team managing pancreatic fluid collections. Despite improvements in technique and devices reflecting the complexity of the disease process, endoscopic drainage remains associated with significant morbidity and potential for mortality and careful patient selection and assesment is mandatory.
1 1 Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis – 2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013; 62(1):102–111.
2 2 Muthusamy VR, Chandrasekhara V, Acosta RD, et al. The role of endoscopy in the diagnosis and treatment of inflammatory pancreatic fluid collections. Gastrointest Endosc 2016; 83(3):481–488.
3 3 Arvanitakis M, Dumonceau J‐M, Albert J, et al. Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence‐based multidisciplinary guidelines. Endoscopy 2018; 50(5):524–546.
4 4 Dumonceau J‐M, Delhaye M, Tringali A, et al. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, updated August 2018. Endoscopy 2019; 51(2):179–193.
5 5 Teoh AYB, Dhir V, Kida M, et al. Consensus guidelines on the optimal management in interventional EUS procedures: results from the Asian EUS group RAND/UCLA expert panel. Gut 2018; 67(7):1209–1228.
Читать дальше