Source: courtesy of Muhammad F. Dawwas and Kofi W. Oppong.
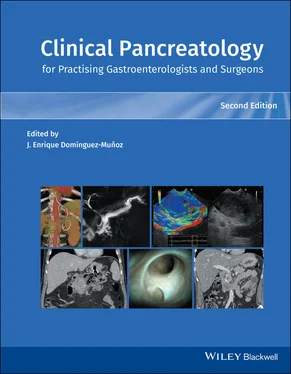
Diagnostic imaging, in the form of contrast‐enhanced computed tomography (CT), magnetic resonance imaging (MRI), or EUS, serves several important goals in the evaluation of pancreatic pseudocysts [2–7]. First, it provides anatomical information on the pseudocyst’s size, wall maturity, solid content, location, and proximity to the wall of the stomach and duodenum. This information is fundamental to decision‐making with regard to the appropriateness and timing of drainage therapy, choice of drainage route, and selection of drainage device. Second, it helps confirm the diagnosis and rule out other cystic lesions with similar radiological appearance such as pancreatic cystic neoplasms and duplication cysts, for which drainage therapy is not only unnecessary but may also potentially render an otherwise resectable tumor unresectable. Third, it can detect pseudoaneurysms arising from the splenic artery or other peripancreatic vessels that would otherwise increase the risk of potentially fatal bleeding in the setting of drainage therapy. Last, it may help evaluate the structural integrity of the pancreatic duct and existence of communication with the pseudocyst, yielding information with important implications for subsequent management.
MRI and endosonography have superior diagnostic accuracy compared with CT for detection of necrotic content and septation, thereby helping to distinguish pseudocysts from both walled‐off necrotic collections and pancreatic cystic neoplasms, respectively. In experienced hands, secretin‐stimulated magnetic resonance cholangiopancreatography (MRCP) and, to a lesser extent, EUS and endoscopic retrograde cholangiopancreatography (ERCP) can be used to evaluate the integrity of the main pancreatic duct and guide endoscopic therapy, such that patients with no evidence of ductal disruption would be candidates for transluminal drainage alone without anticipated benefit from transpapillary stent placement; those with incomplete disruption could potentially benefit from either transluminal or transpapillary drainage (or both); and those with complete rupture (otherwise known as disconnected duct syndrome; see later section) would require long‐term transluminal placement of one or more plastic stents [3,4]. In the setting of suspected peripancreatic pseudoaneurysms, CT and magnetic resonance angiography offer superior diagnostic utility, facilitating preemptive angiographic embolization prior to undertaking an otherwise risky drainage intervention. EUS or image‐guided percutaneous fine‐needle aspiration can potentially determine if a pseudocyst is infected and also exclude a mucinous tumor masquerading as a pseudocyst; however, the procedure is not generally recommended given the high false‐negative and false‐positive rates, and the risk of contaminating an otherwise sterile pseudocyst [2–7].
Conceptually, drainage of pancreatic pseudocysts can be accomplished surgically, percutaneously, or endoscopically.
Open surgical drainage, traditionally the treatment of choice in surgically fit candidates, entails the creation of a cystgastrostomy, cystduodenostomy, or Roux‐en‐Y cystjejunostomy, depending on the location of the pseudocyst and its anatomical relationship to the stomach and duodenum. The procedure has been increasingly performed laparoscopically in recent years and can also be combined with pancreatic resection to address concurrent pancreatic ductal disease. A randomized controlled trial comparing endoscopic and surgical cystgastrostomy for pancreatic pseudocyst drainage reported equivalent efficacy and recurrence rates, with shorter hospital stay, improved quality of life, and lower cost in the endoscopic drainage group [8].
Percutaneous drainage is performed in centers with appropriate interventional radiology expertise and entails ultrasound‐ or CT‐guided placement of a plastic catheter into the pseudocyst, usually utilizing a retroperitoneal approach. Although less invasive than surgical drainage, reliance on this method may present logistic challenges in patients with pseudocysts located in the vicinity of the pancreatic head and neck for whom a transperitoneal (or even transhepatic) drainage approach may be required. Moreover, the procedure carries the risk of creation of a pancreato‐cutaneous fistula, while local complications such as catheter migration and infection are not uncommon.
Endoscopic transluminal drainage has become the mainstay of management for the overwhelming majority of pancreatic pseudocysts in recent years. Transpapillary drainage is another form of endoscopic therapy that is discussed later in this chapter. Hybrid approaches combining the two endoscopic drainage modalities have also been described.
Transluminal stent‐assisted drainage entails the creation of a fistula between the pseudocyst and the lumen of the stomach and duodenum with or without electrocautery assistance and/or wire‐guided balloon dilation of the fistulous tract, followed by placement of one or more stents across the stoma. In early iterations of the procedure, drainage was accomplished with a duodenoscope or therapeutic gastroscope targeting the bulging portion of the stomach or duodenum for electrocautery‐assisted transluminal fistula creation and stent placement. More recently, EUS‐guided transluminal drainage has become the standard of care for drainage of pancreatic pseudocysts, facilitating drainage of nonbulging pseudocysts through a safe, vessel‐free drainage window. Two randomized controlled trials have reported significantly higher technical success rate for EUS‐guided drainage of pancreatic pseudocysts compared to the conventional “blind” approach [9,10]. Prerequisites for EUS‐guided drainage include apposition of the walls of the pseudocyst and stomach or duodenum with a depth of less than 1 cm from the tip of the echoendoscope, an avascular plane, and a mature pseudocyst wall. Plastic stents have conventionally been used. Two main techniques for creation of a transluminal fistula prior to placing plastic stents have been described, both utilizing continuous EUS guidance. In the first technique, the pseudocyst is first punctured with a 19‐gauge needle. An 0.035 or 0.025 inch (0.889 mm or 0.635 mm) wire is then advanced through the needle and coiled into the pseudocyst, usually under fluoroscopic guidance although the procedure can be performed entirely under EUS control. The tract is then dilated using a balloon dilator up to 10 mm, depending on the thickness of the pseudocyst wall. Dilatation with a graduated (4‐5‐7 Fr) biliary dilator may be required prior to balloon dilatation. The other commonly used approach utilises a 10‐Fr cystotome instead of a 19‐gauge needle. The cystotome device (Cook Medical, Bloomington, IN) comprises a needle knife tip, a distal 5‐Fr inner catheter, and a 10‐Fr outer catheter equipped with a diathermy ring at its distal tip. The pseudocyst is punctured using the needle knife tip and the 5‐Fr inner catheter advanced into the cavity. The 10‐Fr catheter is then advanced over the 5‐Fr inner catheter using the ring diathermy to gain access to the pseudocyst. The inner 5‐Fr catheter is then removed and at this stage two 0.035 inch wires can be introduced, with balloon dilatation performed over one of the wires. Placing two wires facilitates rapid second stent placement (if required) following balloon dilatation as the endoscopic view is often suboptimal due to the rapid egress of fluid following dilatation of the tract. Whichever approach is used, one or more plastic pigtail stents are then placed across the stoma. Whilst many experts favor the placement of two plastic double‐pigtail stents, there is no randomized study showing benefit of multiple stents over one stent. In a retrospective study, there was no treatment benefit of multiple stents over one stent or association with stent size (7 Fr vs. 10 Fr). Large and infected collections may benefit from placement of a nasocystic drain and regular irrigation. Given the significant risk of aspiration, endotracheal intubation for the procedure is recommended, particularly for larger collections that are more likely to decompress rapidly. Additionally, CO 2insufflation is preferred to air to minimize the risk of air embolism. The utility of multiple stents is to facilitate flow of fluid around and between stents. The stents are generally removed after a minimum of six weeks. There is some evidence that recurrence rate is inversely related to indwelling time. If a disconnected pancreatic duct is identified on secretin‐stimulated MRCP or ERCP, the stents can be left in place indefinitely. Fully covered self‐expanding metal stents can be used. Initially, biliary metal stents were repurposed. More recently, the advent of lumen‐apposing metal stents (LAMS) delivered through an electrocautery‐tipped delivery platform specifically designed for EUS‐guided deployment has greatly simplified the process of endoscopic drainage of pancreatic fluid collections. The placement of LAMS has significantly shortened procedure time, reduced the requirement for skilled assistants, and obviated the need for fluoroscopy. Moreover, at least theoretically, the large‐diameter, lumen‐apposing, wide flange stent design has enhanced not only the drainage efficacy of the device but also overall safety of the procedure, potentially minimizing the risk of perforation and pseudocyst wall dehiscence in the setting of indeterminate adherence to the gastroduodenal wall. However, LAMS have several disadvantages compared to plastic stents, including substantially higher cost, greater risk of delayed bleeding (particularly when left in situ for more than three weeks), and requirement for subsequent exchange for long‐term plastic stents in the subgroup of patients with disconnected pancreatic duct syndrome who would otherwise be at risk of pseudocyst recurrence. There are as yet no randomized controlled trials comparing LAMS and plastic stents in the management of pseudocysts. Available data is conflicting in terms of overall clinical success and adverse event rates [11–13]. However, plastic stents do appear to be more cost‐effective whilst LAMS have been associated with a higher risk of bleeding [12] ( Figure 17.2).
Читать дальше