Congenital Anomalies
Pancreas Divisum
This is the most common congenital anomaly of the pancreas and is seen in 5–14% of the general population. Pancreas divisum has long been associated with pancreatitis but the causality is suspect. In a large series of patients undergoing ERCP, there was no difference in the prevalence of pancreas divisum in the groups with and without pancreatitis [66]. In patients with idiopathic recurrent acute pancreatitis and pancreas divisum, genetic polymorphism/mutation in serine protease inhibitor Kazal type 1 ( SPINK1 ) and cystic fibrosis transmembrane conductance regulator ( CFTR ) genes have been shown as important cofactors [67]. A randomized controlled trial (SHARP) is currently being conducted to evaluate the efficacy of minor papilla sphincterotomy in patients with recurrent AP and pancreas divisum.
Table 2.3 Independent risk factors for post‐ERCP pancreatitis.
Source : adapted from Dumonceau et al. [63].
|
Odds ratio (95% confidence interval) |
| Patient‐related risk factors |
| Prior post‐ERCP pancreatitis |
8.7 (3.2–23.8) |
| Female sex |
3.5 (1.1–10.6) |
| Previous recurrent pancreatitis |
2.5 (1.9–3.1) |
| Suspected sphincter of Oddi dysfunction |
1.9 (1.4–2.6) |
| Younger patient age (<40 years old) |
1.8 (1.3–2.6) |
| Absence of chronic pancreatitis |
1.9 (1–3.48) |
| Normal serum bilirubin |
1.9 (1.2–2.9) |
| Procedure‐related risk factor |
| Difficult cannulation (>10 minutes) |
1.8 (1.1–2.7) |
| Repetitive pancreatic guidewire cannulation |
2.8 (1.8–4.3) |
| Pancreatic duct injection |
2.2 (1.6–3.0) |
| Pancreatic sphincterotomy |
3.1 (1.6–5.7) |
| Endoscopic papillary large balloon dilatation of intact sphincter |
4.5 (1.5–13.5) |
Anomalous Pancreatobiliary Ductal Union
Anomalous pancreatobiliary ductal union (APBDU) is a congenital pancreatic anomaly resulting from an abnormally long (>1.5 cm) common channel between the terminal ends of the bile duct and pancreatic duct. The putative mechanism is bile reflux into the pancreatic duct, which may result in pancreatitis. APBDU can be diagnosed on MRCP or ERCP. The causal association of APBDU with pancreatitis has not been proven.
This is the cystic dilatation of the intraduodenal part of the bile duct and may cause obstruction to pancreatic outflow. Treatment involves deroofing of the choledochocele by endoscopic sphincterotomy.
This is a rare congenital anomaly due to failure of rotation of the ventral bud. This results in a band of pancreatic tissue encircling the second part of the duodenum. It may cause AP but the association is weak. Annular pancreas generally remains asymptomatic in adults. In a retrospective series of 198 patients (mean age 55.1 ± 18.3 years) with radiologically and/or surgically confirmed annular pancreas, 60% of patients were asymptomatic. Among symptomatic patients, only 16% had AP (i.e. about 7% of adult patients with annular pancreas presented with AP) [68].
Idiopathic Acute Pancreatitis
A patient is labelled as having idiopathic AP if no etiology is identified after clinical evaluation, biochemical investigations (including serum calcium and triglyceride level), and abdominal imaging by ultrasound and CT [21].
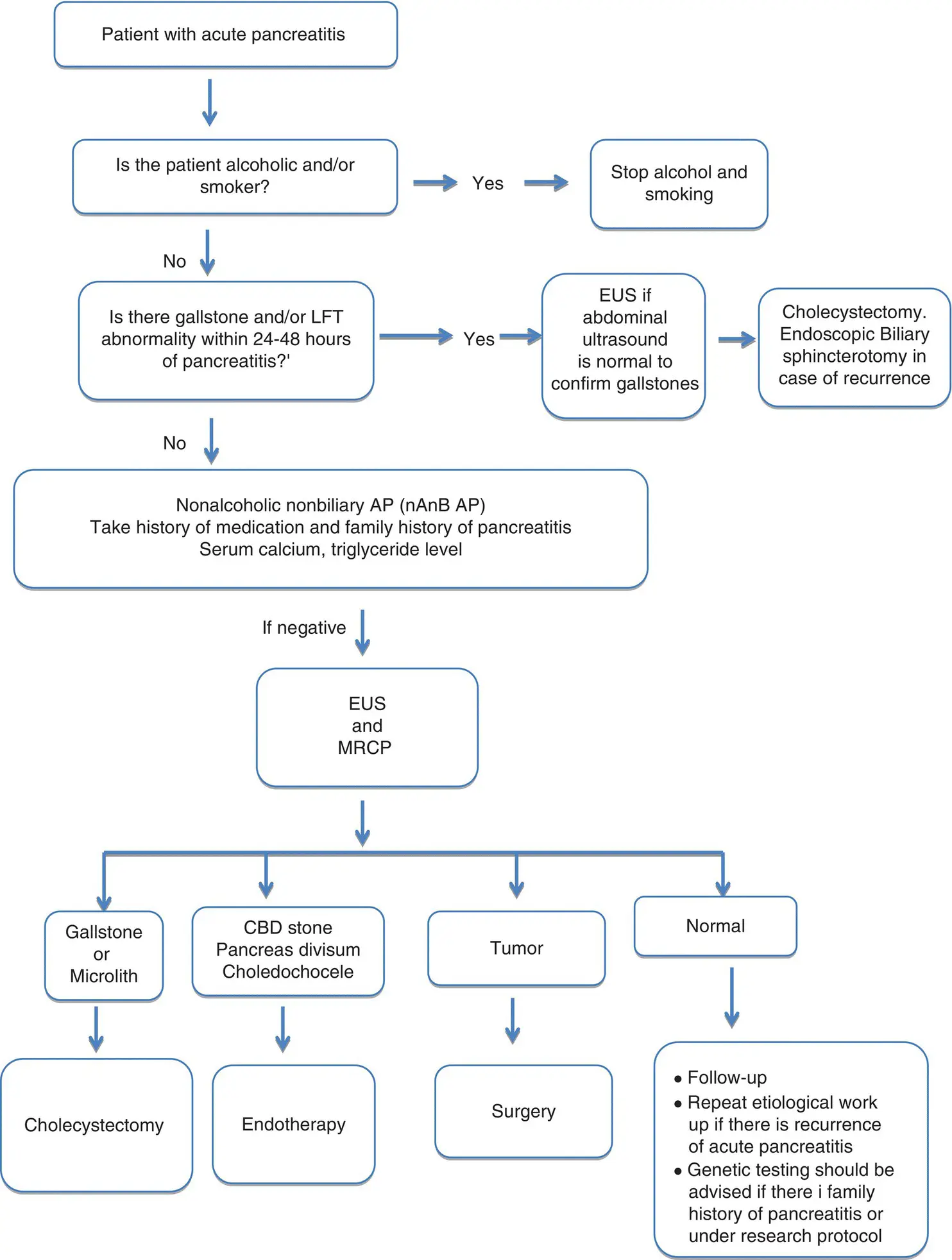
All patients with AP must undergo a diagnostic work‐up to find the cause of the pancreatitis. Figure 2.1shows an algorithmic approach for investigating a patient with AP. Careful history of alcoholism, smoking, medications, family history of pancreatitis, and basic investigations including abdominal USG, and serum calcium and triglyceride levels are essential for initial work‐up. In patients without an identifiable cause, EUS and MRCP should be performed to establish the etiological diagnosis. A repeat evaluation after three to six months of negative work‐up may reveal a cause (e.g. gallstones and occult tumor). A patient with truly idiopathic AP should be advised follow‐up because he or she is at risk of recurrence and may even develop chronic pancreatitis in the long term and thus requires periodic careful assessment.
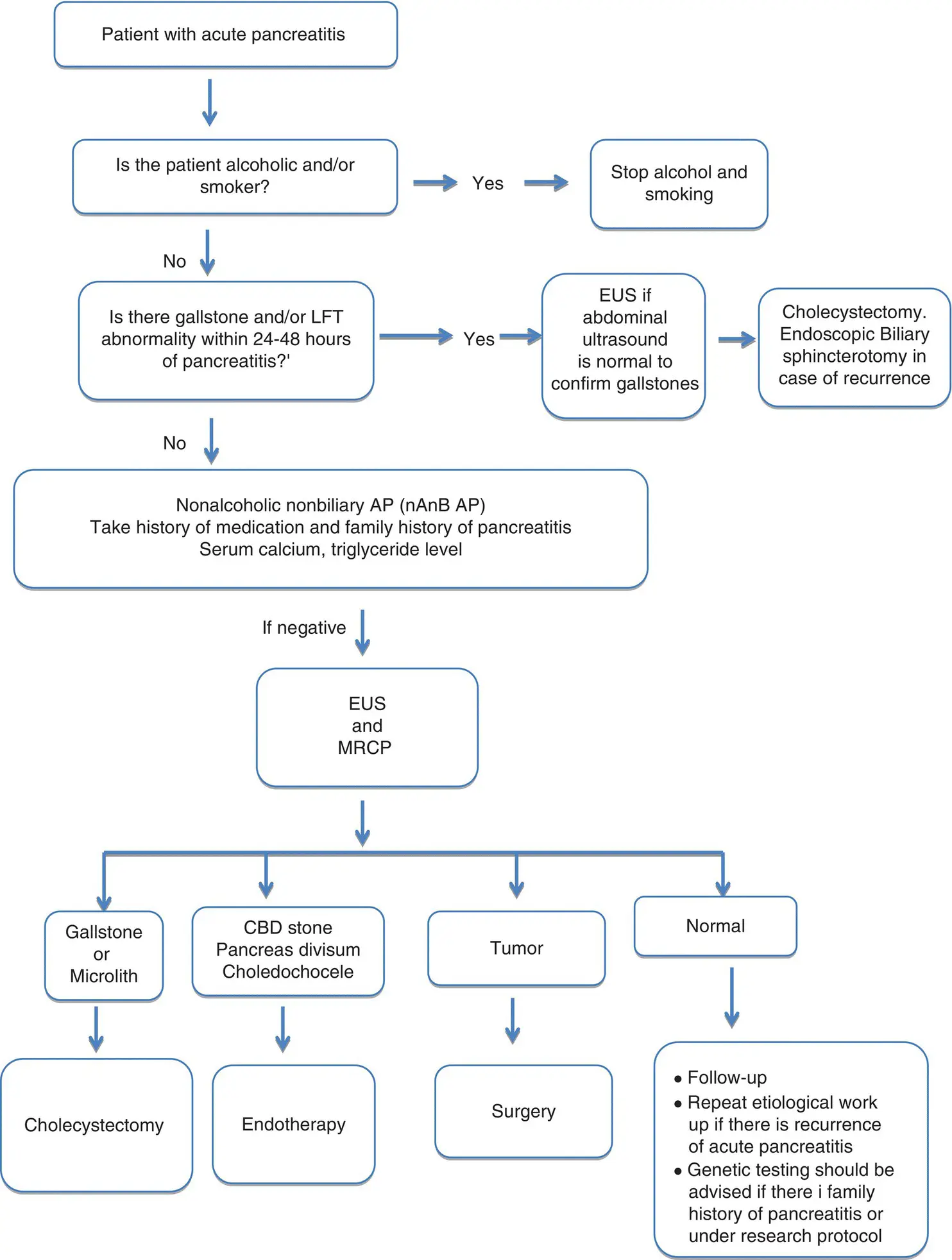
Figure 2.1 Investigative work‐up and treatment for patients with acute pancreatitis to prevent recurrence. CBD, common bile duct; EUS, endoscopic ultrasound; LFT, liver function test; MRCP, magnetic resonance cholangiopancreatography; RAP, recurrent acute pancreatitis.
Source: adapted from Jagannath and Garg [69]. Reproduced with permission of Springer Nature.
Establishing an etiological diagnosis is extremely important in patients with AP to identify the cause and prevent recurrence. Alcohol and gallstones are the most common causes of AP. Biliary pancreatitis is diagnosed if there is elevation of hepatic transaminases on the first day of AP which normalizes in a few days in a patient with gallstones and/or a dilated bile duct. In patients with suspicion of biliary etiology but without demonstrable gallstones, subsequent transabdominal/endoscopic ultrasound after recovery may demonstrate gallstones. Heavy alcohol consumption (>60 g/day) for at least five years may cause alcoholic pancreatitis. Hypercalcemia and HTG are important metabolic causes of AP. Smoking is a risk factor for AP. Patients with idiopathic pancreatitis aged over 50 years should be evaluated for occult pancreatobiliary malignancy if there is no other obvious cause of AP. Patients with AP should undergo an algorithmic investigative work‐up.
1 1 Xiao AY, Tan MLY, Wu LM, et al. Global incidence and mortality of pancreatic diseases: a systematic review, meta‐analysis, and meta‐regression of population‐based cohort studies. Lancet Gastroenterol Hepatol 2016; 1:45–55.
2 2 Schepers NJ, Bakker OJ, Besselink MG, et al. Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis. Gut 2019; 68:1044–1051.
3 3 Padhan RK, Jain S, Agarwal S, et al. Primary and secondary organ failures cause mortality differentially in acute pancreatitis and should be distinguished. Pancreas 2018; 47:302–307.
4 4 Sankaran SJ, Xiao AY, Wu LM, et al. Frequency of progression from acute to chronic pancreatitis and risk factors: a meta‐analysis. Gastroenterology 2015; 149:1490–1500.e1.
5 5 Lankisch PG, Breuer N, Bruns A, et al. Natural history of acute pancreatitis: a long‐term population‐based study. Am J Gastroenterol 2009; 104:2797–2805; quiz 2806.
6 6 Gullo L, Migliori M, Pezzilli R, et al. An update on recurrent acute pancreatitis: data from five European countries. Am J Gastroenterol 2002; 97:1959–1962.
7 7 Garg PK, Madan K, Pande GK, et al. Association of extent and infection of pancreatic necrosis with organ failure and death in acute necrotizing pancreatitis. Clin Gastroenterol Hepatol 2005; 3:159–166.
8 8 Nitsche C, Maertin S, Scheiber J, et al. Drug‐induced pancreatitis. Curr Gastroenterol Rep 2012; 14:131–138.
9 9 Lerch MM, Aghdassi A. Gallstone‐related pathogenesis of acute pancreatitis. Pancreapedia: The Exocrine Pancreas Knowledge Base. https://www.pancreapedia.org/reviews/gallstone‐related‐pathogenesis‐of‐acute‐pancreatitis
Читать дальше