Among the types of (peri)pancreatic fluid collections, an important distinction is made between collections composed of fluid alone (acute peripancreatic fluid collection and pancreatic pseudocyst) and those that arise from necrosis and contain a solid component (acute necrotic collection and walled‐off necrosis). There is good interobserver agreement for the types of (peri)pancreatic fluid collections as defined by the RAC, particularly among experienced radiologists [22].
Table 3.2 Modified Marshall scoring system.
Source: Banks et al. [12]. © 2013 BMJ. Reproduced with permission of BMJ Publishing Group.
|
Score |
| Organ system |
0 |
1 |
2 |
3 |
4 |
| Respiratory ( P aO 2/ F iO 2) |
>400 |
301–400 |
201–300 |
101–200 |
<101 |
| Renal (serum creatinine, mg/dl) |
<1.4 |
1.4–1.8 |
1.9–3.6 |
3.6–4.9 |
>4.9 |
| Renal (serum creatinine, μmol/l) |
<134 |
134–169 |
170–310 |
311–439 |
>439 |
| Cardiovascular (systolic blood pressure, mmHg) |
>90 |
<90, fluid responsive |
<90, not fluid responsive |
<90, pH <7.3 |
<90, pH <7.2 |
A score ≥ 2 in any organ system defines the presence of organ failure in AP.
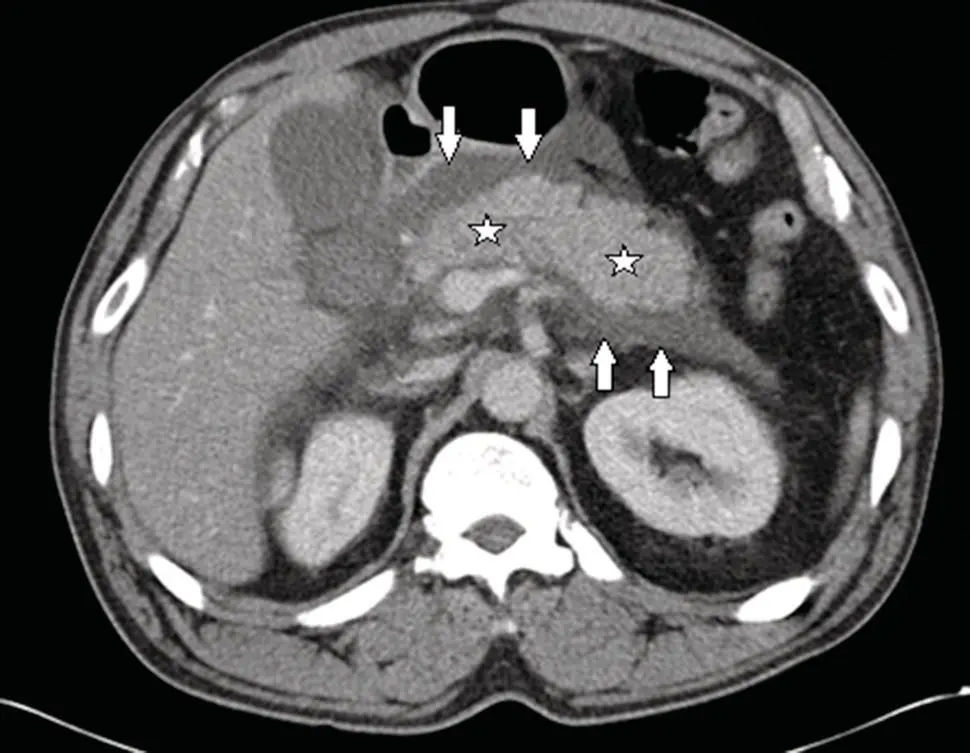
Acute Peripancreatic Fluid Collection
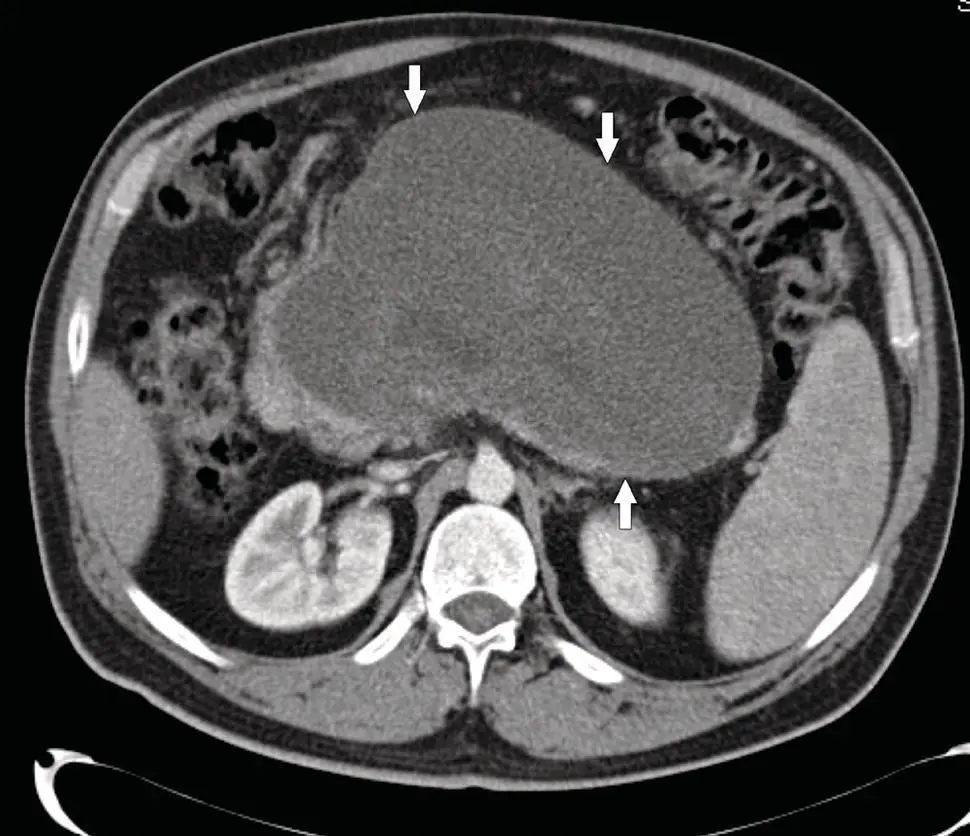
Acute peripancreatic fluid collections (APFCs) are fluid collections that develop in the early phase (less than four weeks) of interstitial edematous pancreatitis. On CECT ( Figure 3.1), APFCs are homogeneous collections that lack a defined wall and are confined by normal fascial planes in the retroperitoneum. Most APFCs resolve spontaneously, although rarely APFCs may evolve into pancreatic pseudocysts if persistent beyond four weeks. The majority of APFCs, which spontaneously resolve and remain asymptomatic, do not require treatment.
APFCs that persist for more than four weeks may organize into homogeneous fluid collections surrounded by a well‐defined wall ( Figure 3.2). These pseudocysts are thought to arise from leakage of amylase‐rich pancreatic juice from the main pancreatic duct or its side branches. Pancreatic pseudocyst formation after an episode of AP is a rare event. Most well‐defined collections are composed not just of pancreatic fluid, but rather a mixture of necrotic solid/liquid tissue and should be termed “walled‐off necrosis” (defined in a subsequent section). Pseudocysts that remain sterile and asymptomatic do not require treatment.
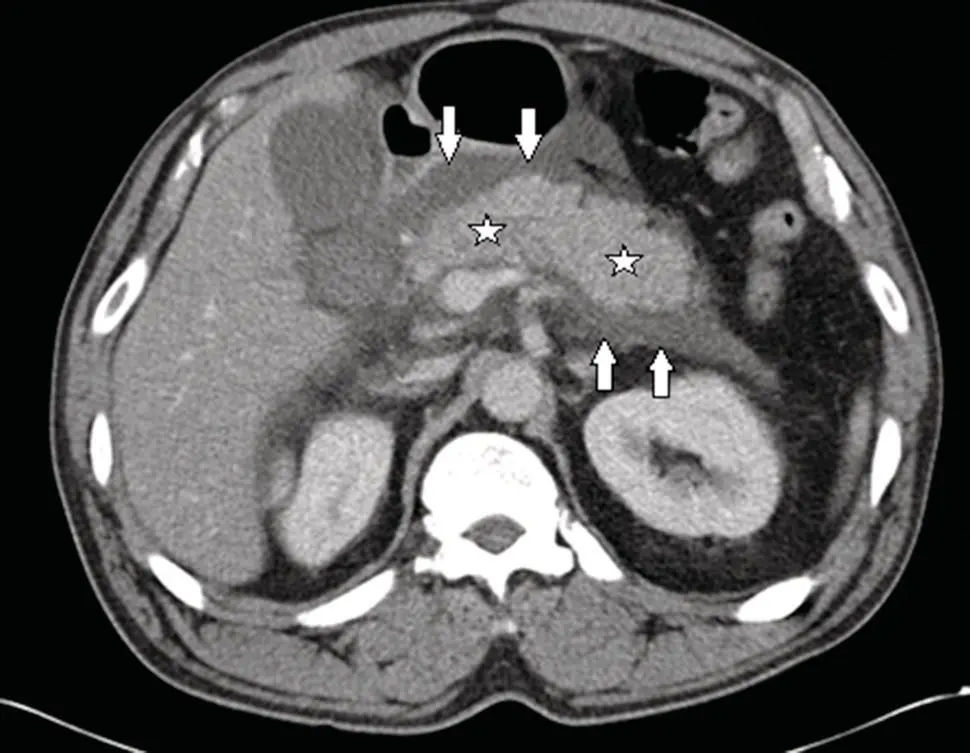
Figure 3.1 CECT showing acute interstitial edematous pancreatitis with acute peripancreatic fluid collection (APFC) in the lesser sac and the left anterior pararenal space (arrows indicate borders of APFC). The pancreatic parenchyma (stars) enhances completely, indicating absence of parenchymal necrosis.
Source: courtesy of Peter A. Banks.
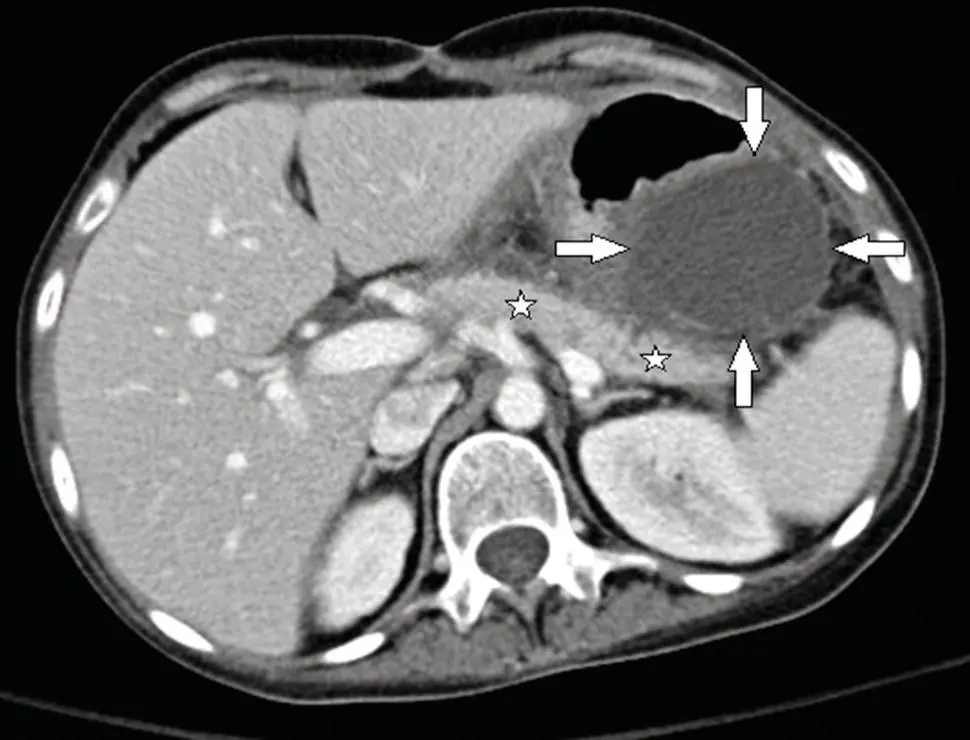
Figure 3.2 CECT showing a pancreatic pseudocyst more than four weeks after an episode of acute interstitial edematous pancreatitis. Note the round homogeneous fluid collection surrounded by a well‐defined wall (arrows indicate border of pseudocyst). The pancreatic parenchyma (stars) enhances completely, indicating absence of parenchymal necrosis.
Source: courtesy of Peter A. Banks.
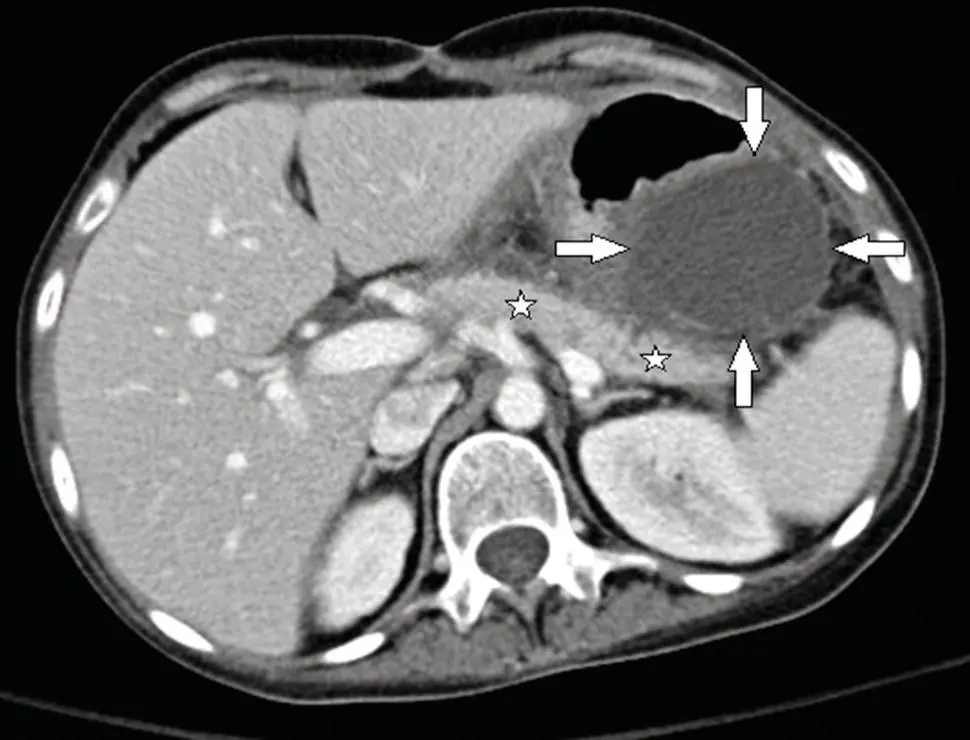
Acute Necrotic Collection
Acute necrotic collections (ANCs) are collections containing a variable amount of liquid and solid tissue that arise during the initial four weeks of necrotizing pancreatitis. Necrosis involves only peripancreatic tissue in up to 50% of cases, which has more favorable outcomes compared to necrosis involving both the pancreatic parenchyma and peripancreatic tissue [23]. ANCs may appear poorly organized or loculated, disrupt fascial planes, and become infected. On CECT ( Figure 3.3), ANCs contain varying amounts of solid necrotic tissue, though this may not be readily apparent until five to seven days after AP onset. The presence of gas is highly suggestive of infected necrosis. When in doubt, magnetic resonance imaging (MRI) may help confirm the presence of solid content. After more than four weeks, ANCs typically mature into walled‐off necrotic collections.
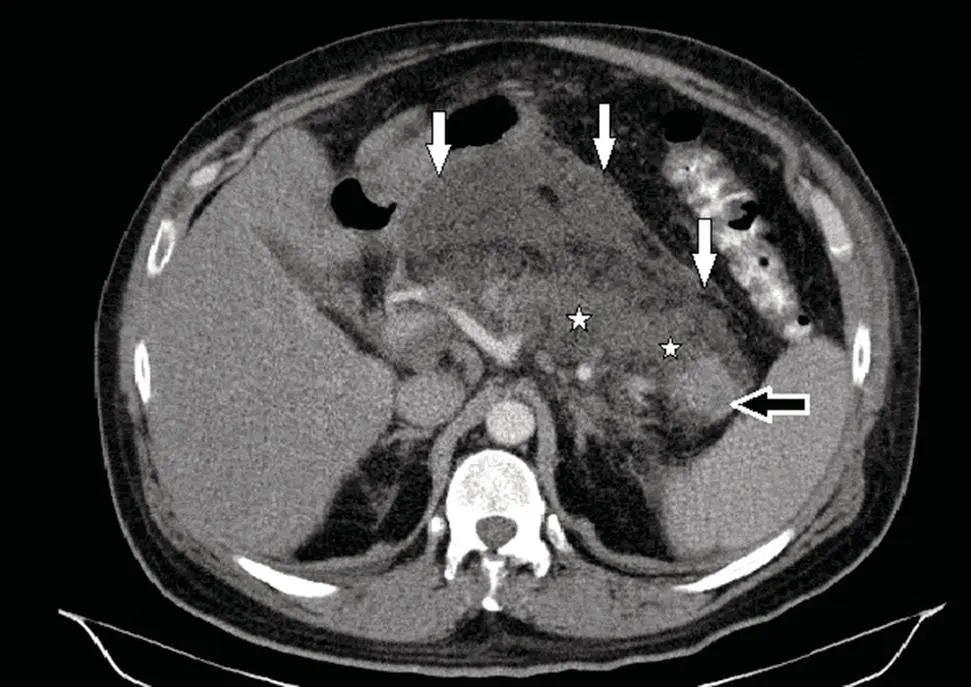
Figure 3.3 CECT showing acute necrotizing pancreatitis with an acute necrotic collection (ANC) involving both the pancreatic parenchyma and peripancreatic tissue (white arrows point to border of ANC). Note the heterogeneous appearance of liquid and solid contents within the ANC. There is extensive pancreatic necrosis (stars) with a small amount of normally enhancing tissue in the pancreatic tail (black arrow).
Source: courtesy of Peter A. Banks.
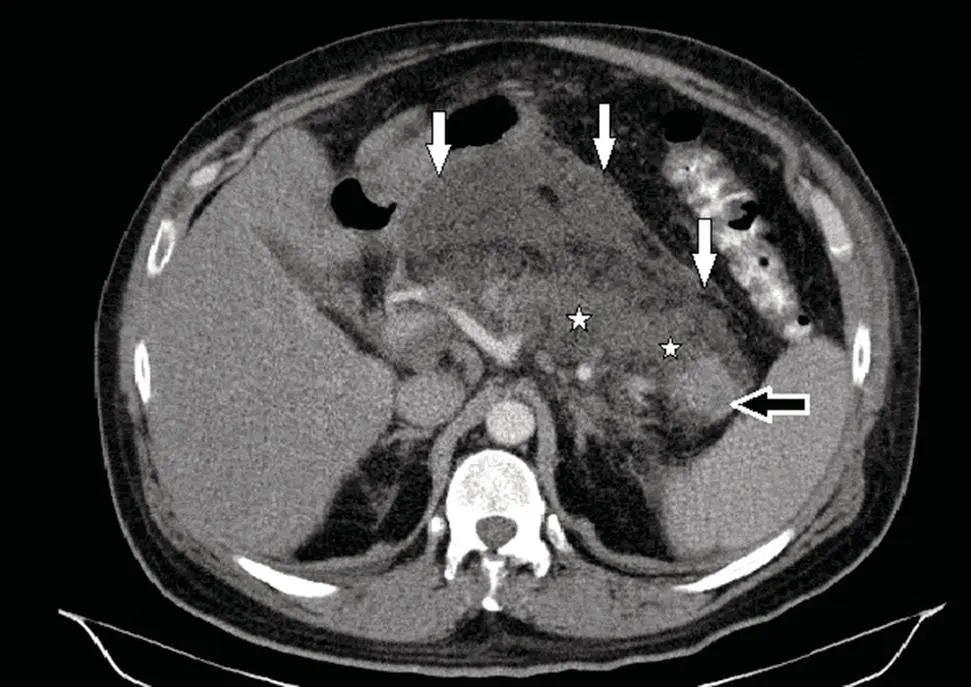
Walled‐off necrosis are mature collections of (peri)pancreatic necrosis encapsulated by an inflammatory wall that forms more than four weeks following onset of necrotizing pancreatitis. On CECT ( Figure 3.4), walled‐off necrosis appears as a heterogeneous collection of liquid and solid necrotic tissue surrounded by a well‐defined rim. Like other local fluid collections, walled‐off necrosis may become infected.
The RAC defines systemic complications of AP as an exacerbation of preexisting comorbid conditions, such as coronary artery disease, congestive heart failure, or chronic lung disease.
Definition of Severity in Acute Pancreatitis
The RAC defines three degrees of AP severity: mild, moderately severe, and severe (see Table 3.1). Stratification of AP severity plays an important part in clinical management, as it may aid in the identification of patients who require early aggressive treatment, who need to monitored in an intensive care setting, or who need to be transferred for specialist care.
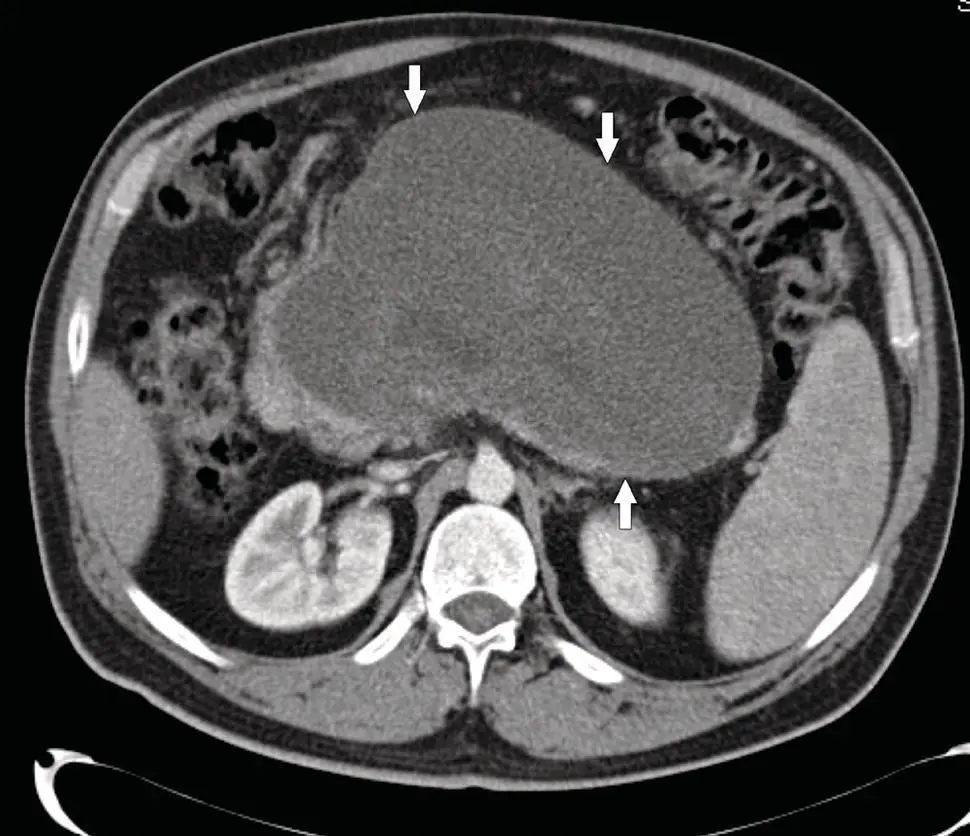
Figure 3.4 CECT showing walled‐off necrosis (WON) more than four weeks after an episode of necrotizing pancreatitis. The heterogeneous collection has replaced most of the pancreatic parenchyma and has a thin, well‐defined, encapsulating wall (white arrows point to border of WON).
Source: courtesy of Peter A. Banks.
Mild AP is characterized by absence of both organ failure and local/systemic complications. Approximately 60–70% of AP patients develop a mild disease course and recover within one week, with minimal morbidity and mortality (<1%).
Moderately Severe Acute Pancreatitis
Moderately severe AP is characterized by the presence of transient (<48 hours) organ failure and/or local and/or systemic complications. Approximately 20–30% of AP patients develop a moderately severe disease course. While those with transient organ failure or an acute fluid collection may experience rapid resolution of symptoms, patients who develop persistent fluid collections or necrotic collections may experience prolonged hospitalizations, difficulty with oral feeding, and long‐term morbidity. Like mild AP, mortality in moderately severe AP is minimal (1–3%).
Читать дальше