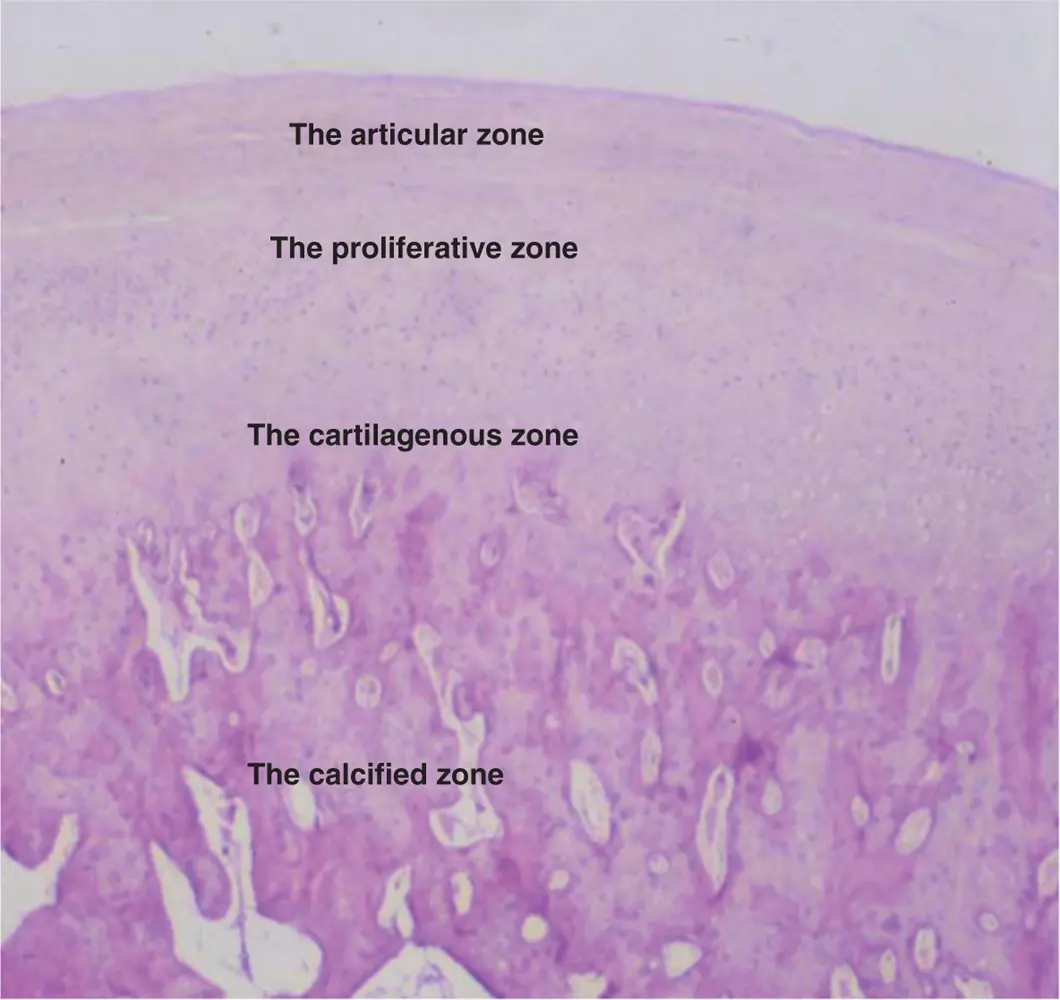
1 The articular zone is dense fibrous connective tissue and forms the outer functional surface of the condyle head. As a result of this fibrous connective tissue layer, it is suggested that it is less susceptible to the effect of ageing and breakdown over time. In addition, despite a poor blood supply, it has a better ability to repair, good adaptation to sliding movement, and the ability to act as a shock absorber when compared with hyaline cartilage.
2 The proliferative zone is mainly cellular and is the area in which undifferentiated germinative mesenchyme cells are found. This layer is responsible for the proliferation of the articular cartilage and the proliferative zone is capable of regenerative activity and differentiation throughout life.
3 The cartilagenous zone contains collagen fibres arranged in a criss‐cross pattern of bundles. This offers considerable resistance against compressive and lateral forces but becomes thinner with age.
4 The calcified zone is the deepest zone and is made up of chondrocytes, chondroblasts, and osteoblasts. This is an active site for remodelling activity as bone growth proceeds.
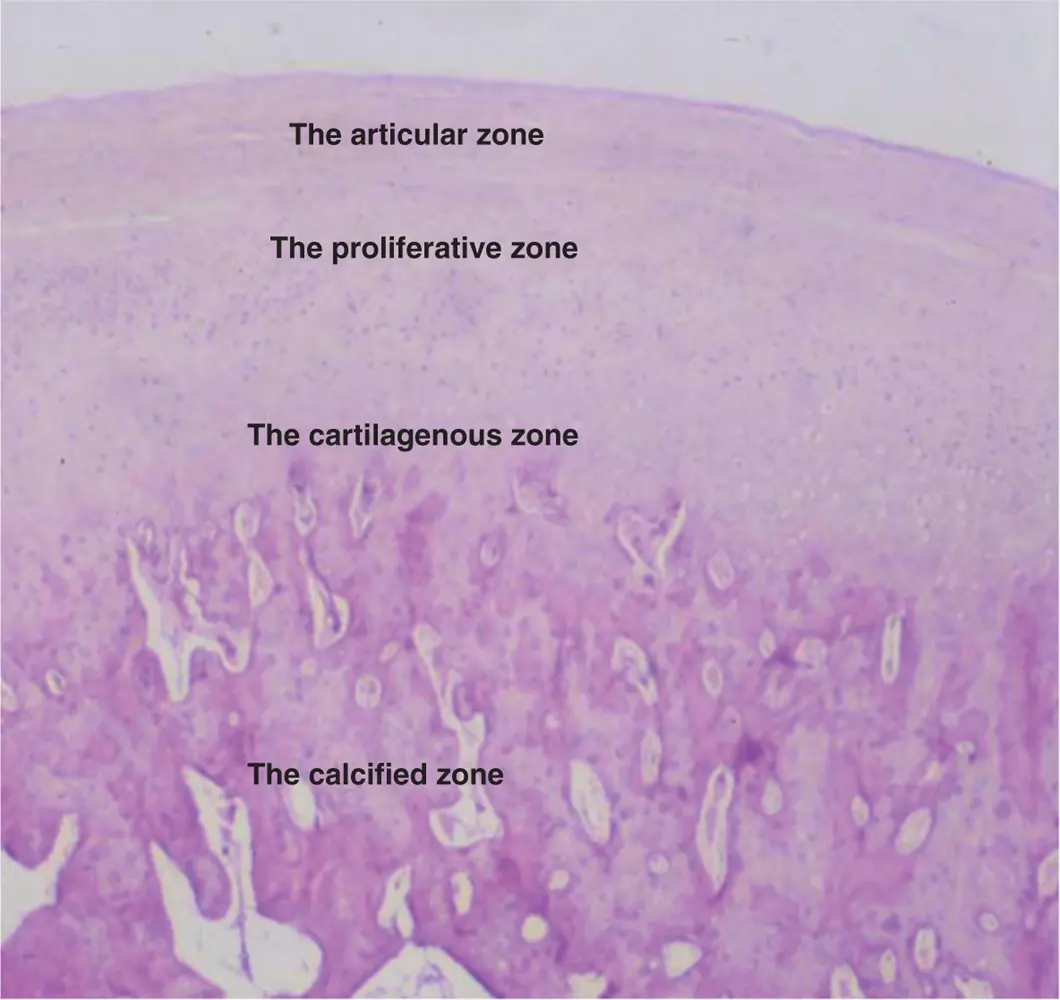
Figure 2.2The four distinct zones described in the articular surface of the condyle and mandibular fossa
(M. Ziad Al‐Ani, Robin J.M. Gray.)
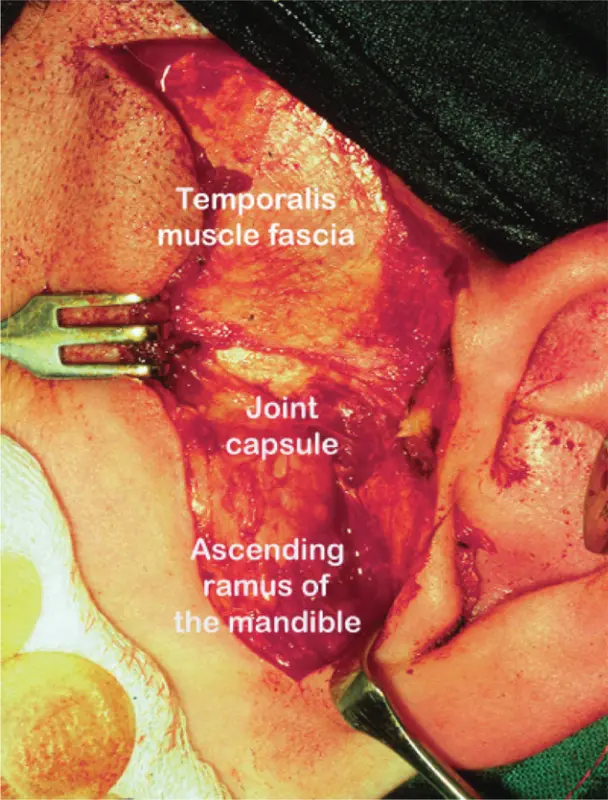
The joint capsule ( Figure 2.3) envelops the articular disc and is attached superiorly to the rim of the glenoid fossa and articular eminence and inferiorly to the neck of the condyle. Posteriorly it is attached to the bilaminar zone and anteriorly becomes continuous with the pterygoid muscle attachment. Although it is thin both anteriorly and posteriorly, it is strengthened laterally by the lateral temporomandibular ligament which is not a discrete ligament but a thickened part of the capsule.
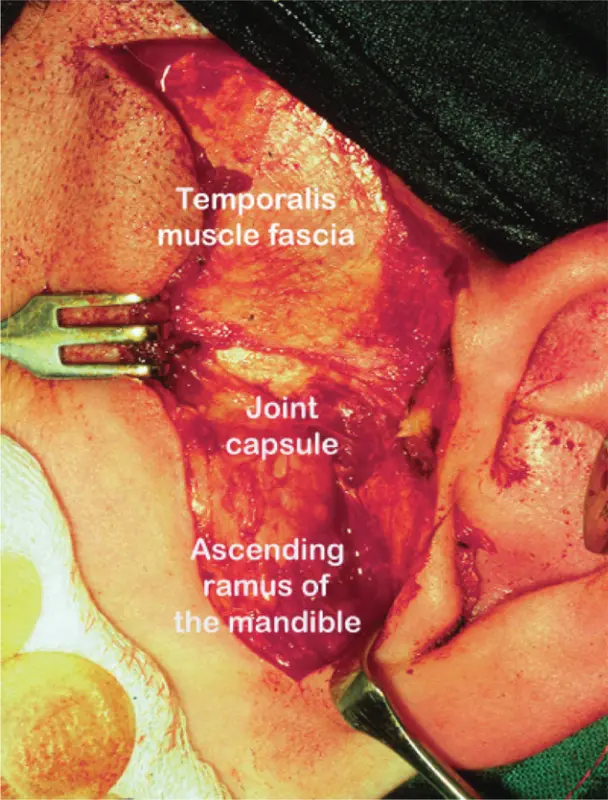
Figure 2.3The joint capsule
(M. Ziad Al‐Ani, Robin J.M. Gray.)
The glistening inner surface of the capsule comprises the synovial membrane. At birth, this membrane covers all internal joint surfaces but is lost from articular surfaces as function commences. The flexibility of the inner surface of the capsule is increased by finger‐like projections (villi) of the synovial membrane which disperse the synovial fluid.
The function of the synovial membrane is considered to be
regulatory because it controls electrolyte balance and nutrients
secretory via the interstitial cells
phagocytic.
Synovial fluid is a clear, pale‐yellow, viscous solution secreted by the synovial tissues and consists mainly of an ultrafiltrate of plasma enriched with a proteoglycan‐containing hyaluronic acid synthesised by synovial cells. The high viscosity of this fluid is a result of the presence of sodium hyaluronate which provides lubrication. The synovial fluid also allows removal of degradation products from the joint space, lubrication of the joint surfaces, and nutrition of the vascular parts of the joint.
Ligaments 
The temporomandibular ligament
The temporomandibular ligament is a strong band of fibrous tissue originating as a thickening of the lateral aspect of the joint capsule. It starts at the root of the zygoma and passes obliquely towards the posterior margin of the neck of the condyle, blending into the joint capsule. In the rest position, this ligament is relaxed, but it is thought that, during retrusive and protrusive movements of the condyle, it limits movement in an anteroposterior direction.
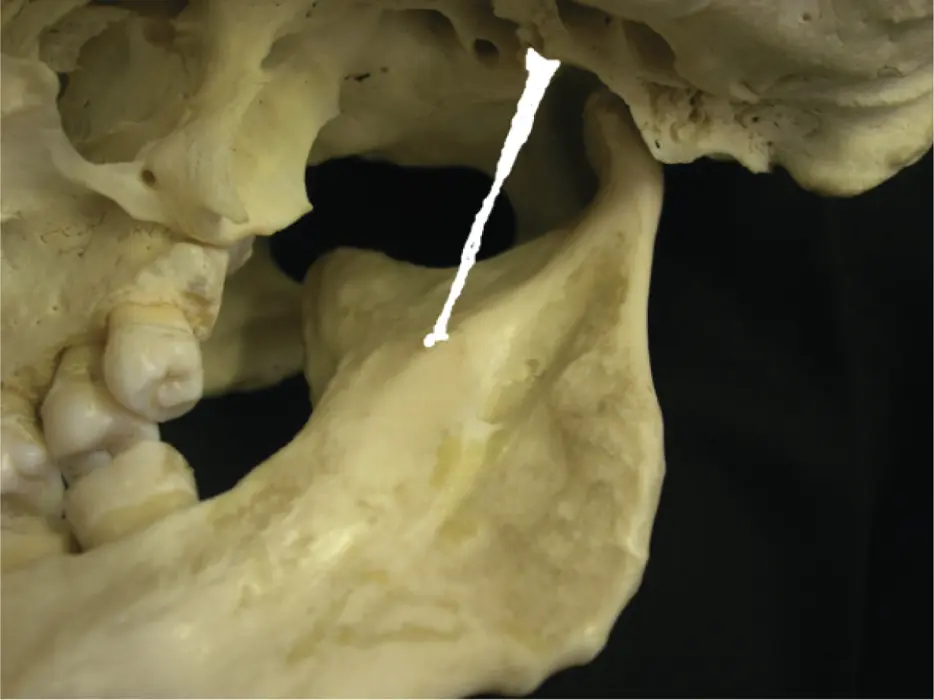
The stylomandibular ligament
This is considered as an accessory ligament. It is a specialised band of cervical fibrous tissue extending from the styloid process to the medial border of the mandible at its angle ( Figure 2.4). The function of this ligament is not clear but it is thought to limit anteroposterior movements of the mandible.
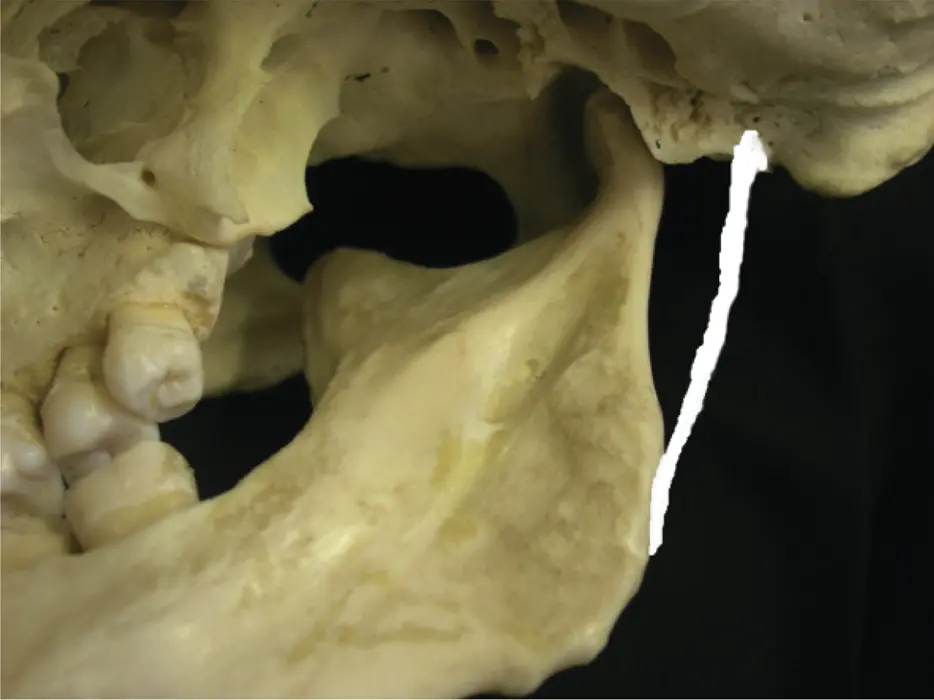
Figure 2.4The position of stylomandibular ligament.
(M. Ziad Al‐Ani, Robin J.M. Gray.)
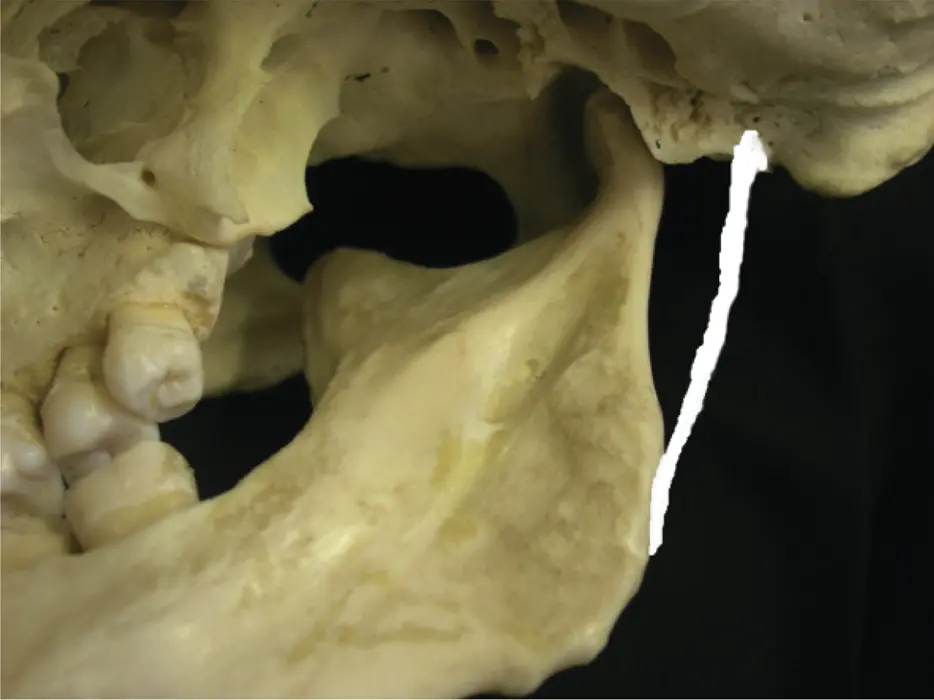
The sphenomandibular ligament
This ligament is also considered to be accessory. It comprises a flat band of fibrous tissue originating from the spine of the sphenoid bone and passes down to its insertion at the inferior margin of the mandibular foramen (lingula) ( Figure 2.5). Again, its function is not certain, but it is thought to limit lateral condylar movements.
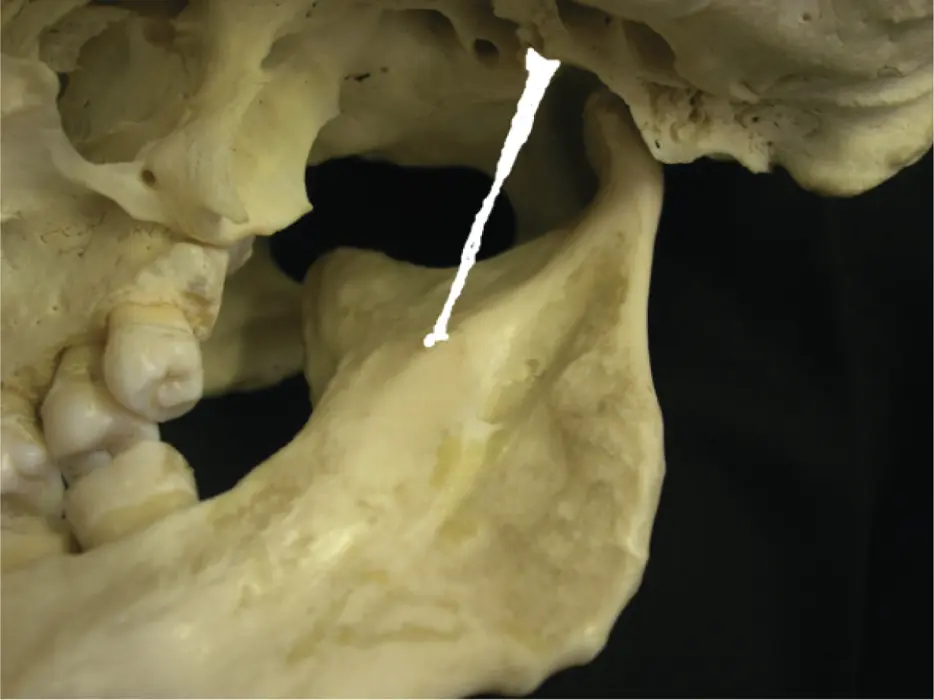
Figure 2.5The position of sphenomandibular ligament.
(M. Ziad Al‐Ani, Robin J.M. Gray.)
The intra‐articular disc (meniscus) 
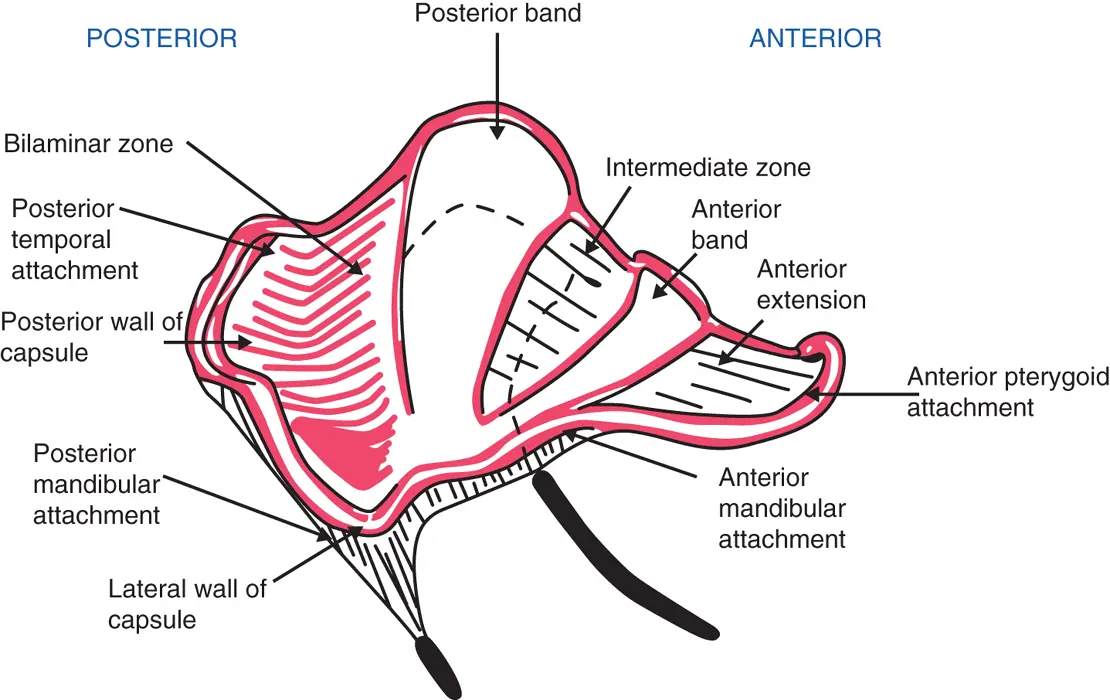
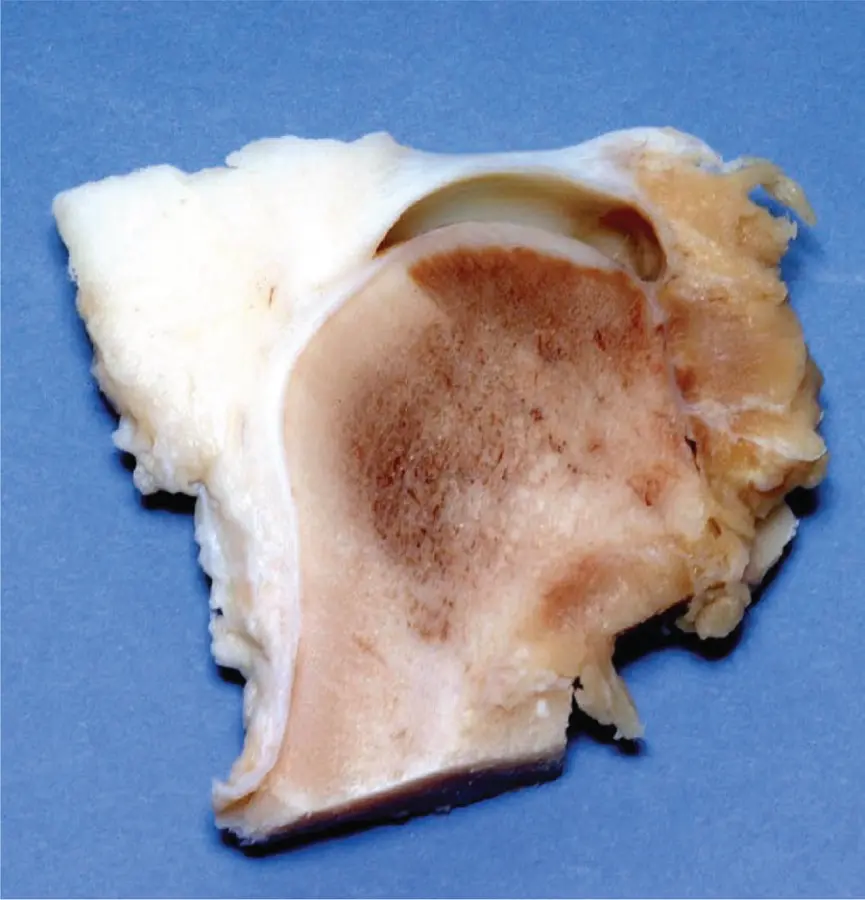
About 55 years ago, Rees described the intra‐articular disc as being like a ‘school‐boy’s cap'. It is an oval‐shaped tense sheet of fibrous tissue with a concave inferior surface sitting on the head of the condyle ( Figure 2.6). On its posterior aspect, it has a convex upper surface; it becomes saddle‐shaped on its anterior aspect. It overlays the condylar head and blends medially and laterally with the capsule. It is also attached to the medial and lateral poles of the condyle and anteriorly to the superior pterygoid muscle. This structural arrangement, as it is interposed between the head of the condyle and the glenoid fossa, divides the joint into the upper and lower joint spaces ( Figure 2.7).
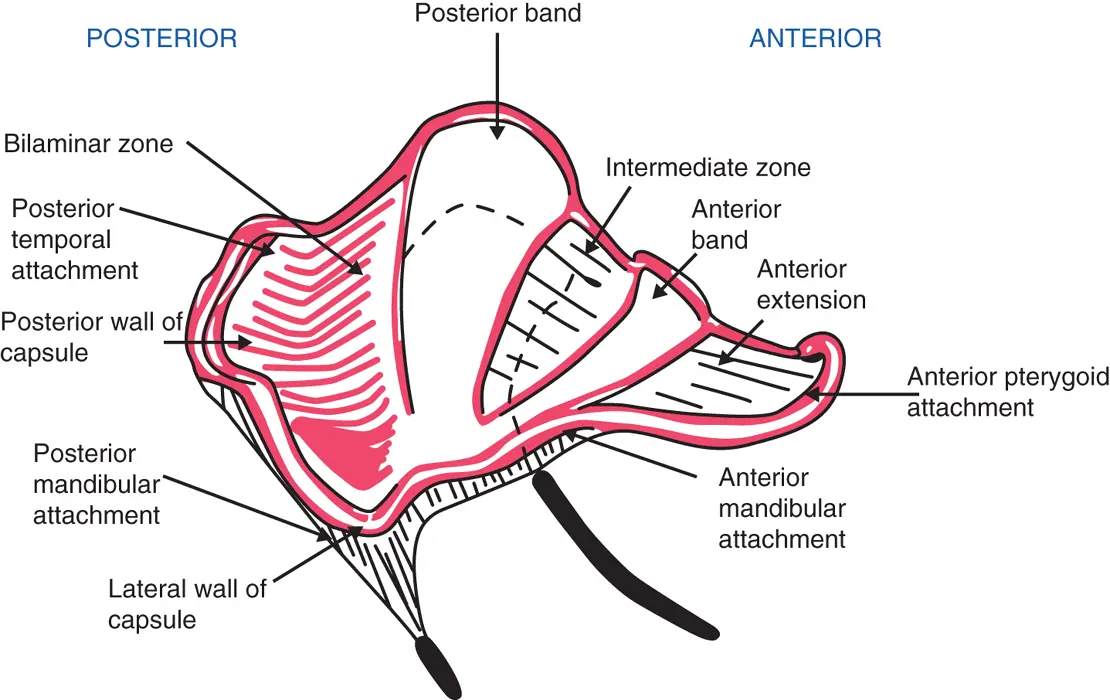
Figure 2.6Diagram of disc morphology.
(Rees LA. The structure and function of the mandibular joint. J Br Dent Assoc 1954; XCVI:126–33.)
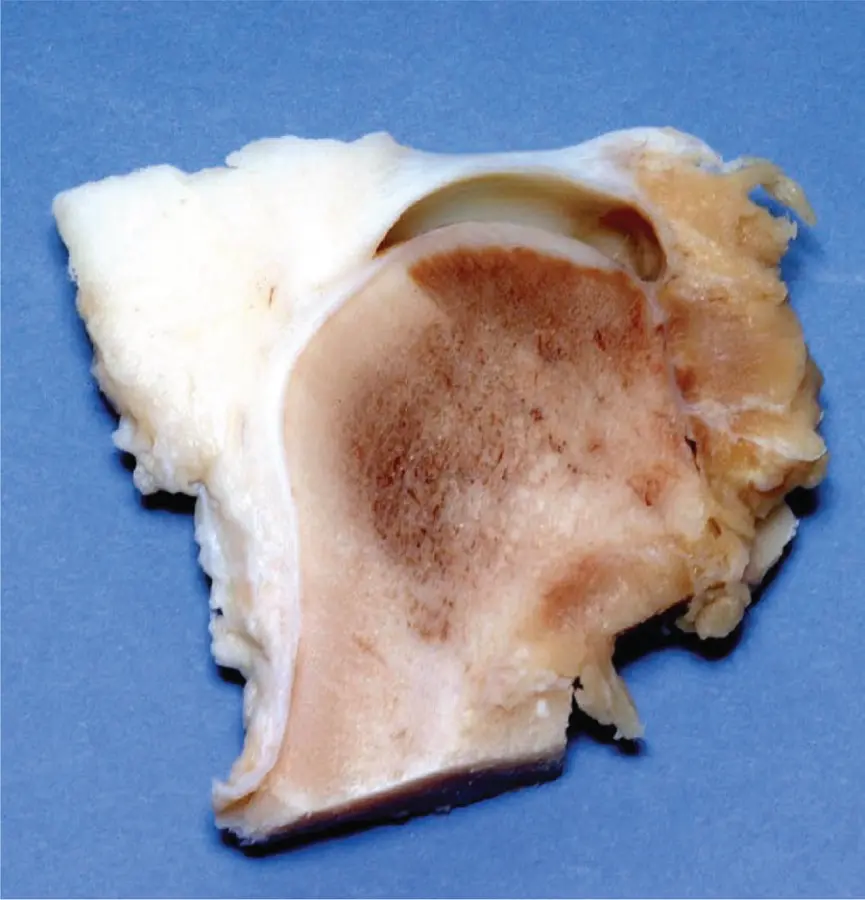
Figure 2.7Sagittal section of porcine temporomandibular joint. As in human beings, the articular surface of the mandibular condyle is convex and joins the lower articular surface of the meniscus, which is concave, to form a condylomeniscal joint.
(M. Ziad Al‐Ani, Robin J.M. Gray.)
There are four zones of the disc:
1 The anterior band which is of moderate thickness but narrow in an anteroposterior direction.
2 The intermediate band, which is the thinnest zone of the disc.
3 The posterior band, which is both the thickest and the widest transverse zone of the disc.
4 The bilaminar zone, which consists of two parts: the superior band, which is attached to the posterior wall of the glenoid fossa and squamotympanic fissure and is elastic, and the inferior band, which is attached to the neck of the condyle and is fibrous.
The disc is attached anteriorly to the margin of the articular eminence superiorly and to the articular margin of the condyle inferiorly. Posteriorly, the disc is attached to the glenoid fossa and squamotympanic fissure (elastic attachment) and to the distal aspect of the neck of the condyle (fibrous attachment). This is termed the ‘posterior bilaminar zone’. Medially and laterally the meniscus blends with the capsule. The disc is also attached to adjacent muscles, namely the lateral pterygoid (anteriorly) and masseter and temporalis muscles (laterally). The fibres of the lateral pterygoid muscle merge with the disc anteriorly to form its true insertion. The connections with the masseter and temporalis muscles are less strong, consisting of fibrous bands of thickened tissue at right angles to the direction of the muscle fibres.
Читать дальше






![John Bruce - The Lettsomian Lectures on Diseases and Disorders of the Heart and Arteries in Middle and Advanced Life [1900-1901]](/books/749387/john-bruce-the-lettsomian-lectures-on-diseases-and-disorders-of-the-heart-and-arteries-in-middle-and-advanced-life-1900-1901-thumb.webp)