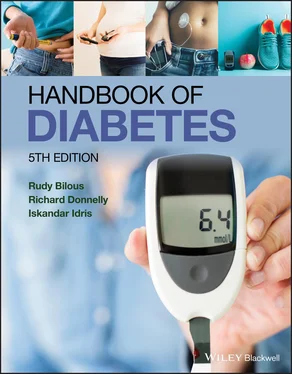
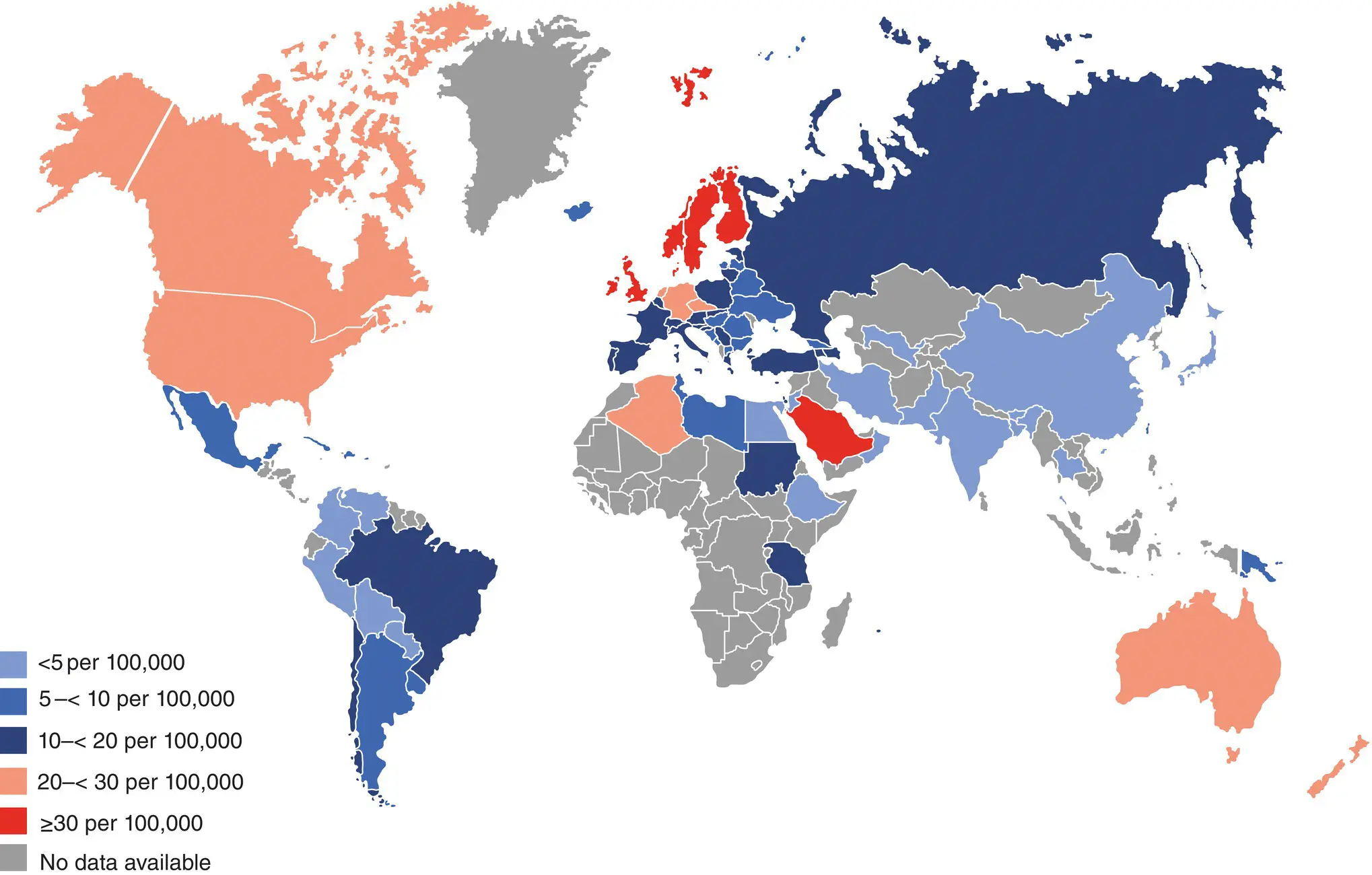
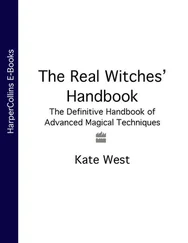
There is a striking variation in the incidence of type 1 diabetes between and within populations. Part of the problem has been the lack of full case ascertainment in carefully defined populations. Historically, the highest incidence rates have been in Northern Europe, but rates are rapidly increasing in other regions such as the Middle East ( Figure 6.1and Table 6.1). The variation in incidence by geographical position in Europe is striking ( Figure 6.2) and might reflect the impact of environmental factors. Incidence rates themselves have been increasing over the past three decades. In Europe the average rate of increase from 1989–2013 was 3.4% per annum reflecting a doubling in 20 years. However, the average hides considerable variation with rates of increase slowing in Scandinavia, Ireland, Italy, and Spain and some UK centres, and increasing in others (Poland, Romania, Lithuania, and Macedonia). Lower rates of increase in the decade 2002–2012 have been reported in in the USA (1.8% pa), Canada (1.3% pa) and Australia (0.4% pa); but much higher rates in China (with historically a very low incidence) of 12% pa in Zhejiang province from 2007–2013. These rates of increase must be mediated by environmental factors as they are occurring too rapidly to reflect changes in genetic susceptibility. One explanation of the observed increase in incidence in global regions with a historically low rate has correlated the change to an increased life expectancy at birth and a mathematical model of how this would translate into natural selection. These scientists suggest that as more individuals live to reproductive age then the likelihood of transmitting diabetes (and other disease) susceptibility genes increases.
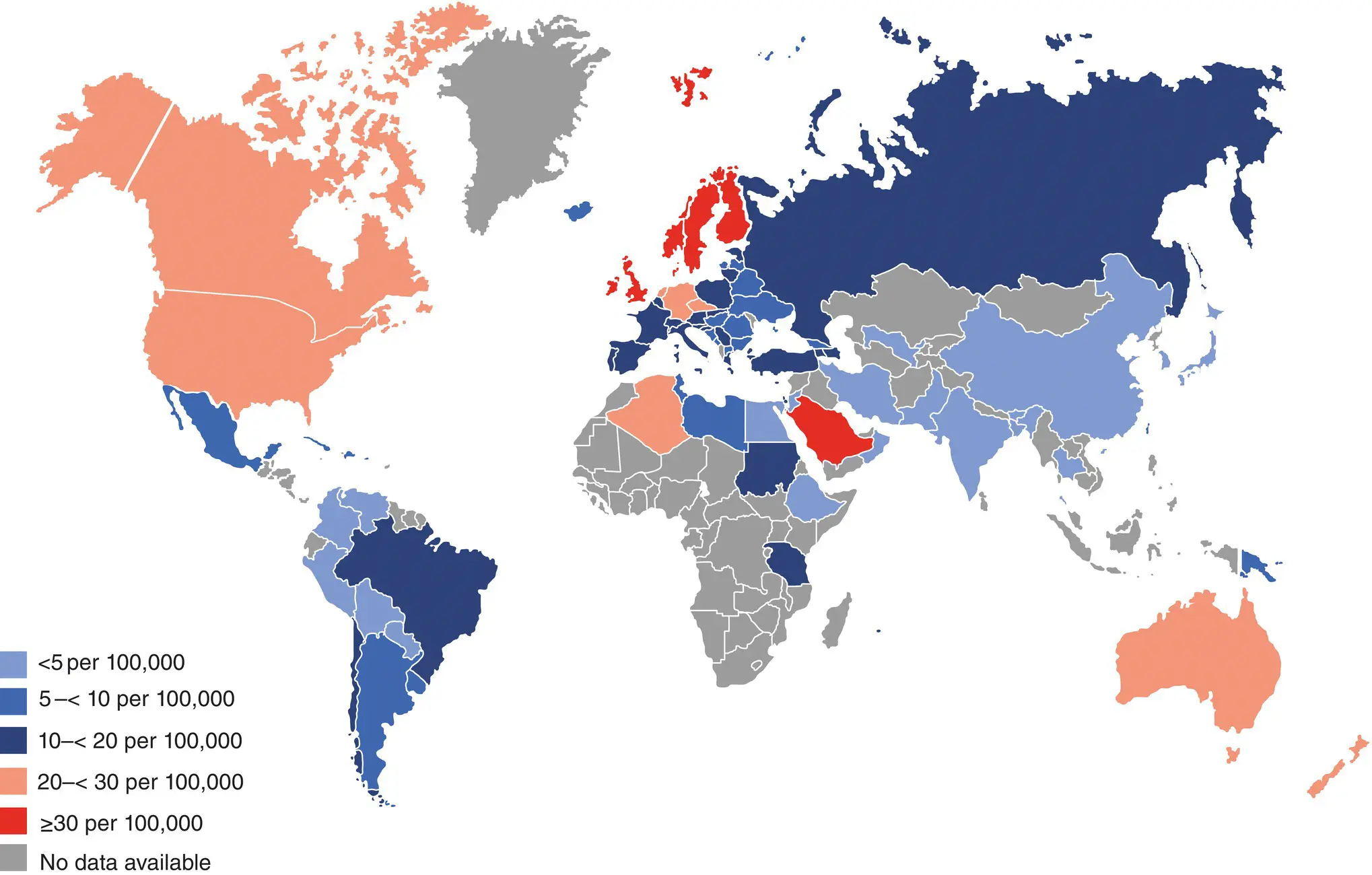
Figure 6.1 Age and sex standardised incidence rates per 100,000 population per year for type 1 diabetes in children and adolescents aged 0–14 years.
Reproduced from the IDF Diabetes Atlas 9th edition 2019 with permission.
Table 6.1 Highest global rates of incidence per annum of type 1 diabetes in children aged 0–14 years per 100,000 population.
| Rank |
Country |
Incidence Rates /100,000 Population / Year |
| 1 |
Finland |
62.3 |
| 2 |
Sweden |
43.2 |
| 3 |
Kuwait |
41.7 |
| 4 |
Norway |
33.6 |
| 5 |
Saudi Arabia |
31.4 |
| 6 |
Canada |
29.9 |
| 7 |
United Kingdom |
29.4 |
| 8 |
Qatar |
28.4 |
| 9 |
Ireland |
27.5 |
| 10 |
Denmark |
27.0 |
Data from the IDF Diabetes Atlas 9th edition 2019 with permission.
There is some evidence of a cyclical variation in incidence from some, but not all, centres in the EURODIAB epidemiological study with a periodicity of 4–6 years, and may reflect exposure to infectious agents such as H1N1 influenza A.
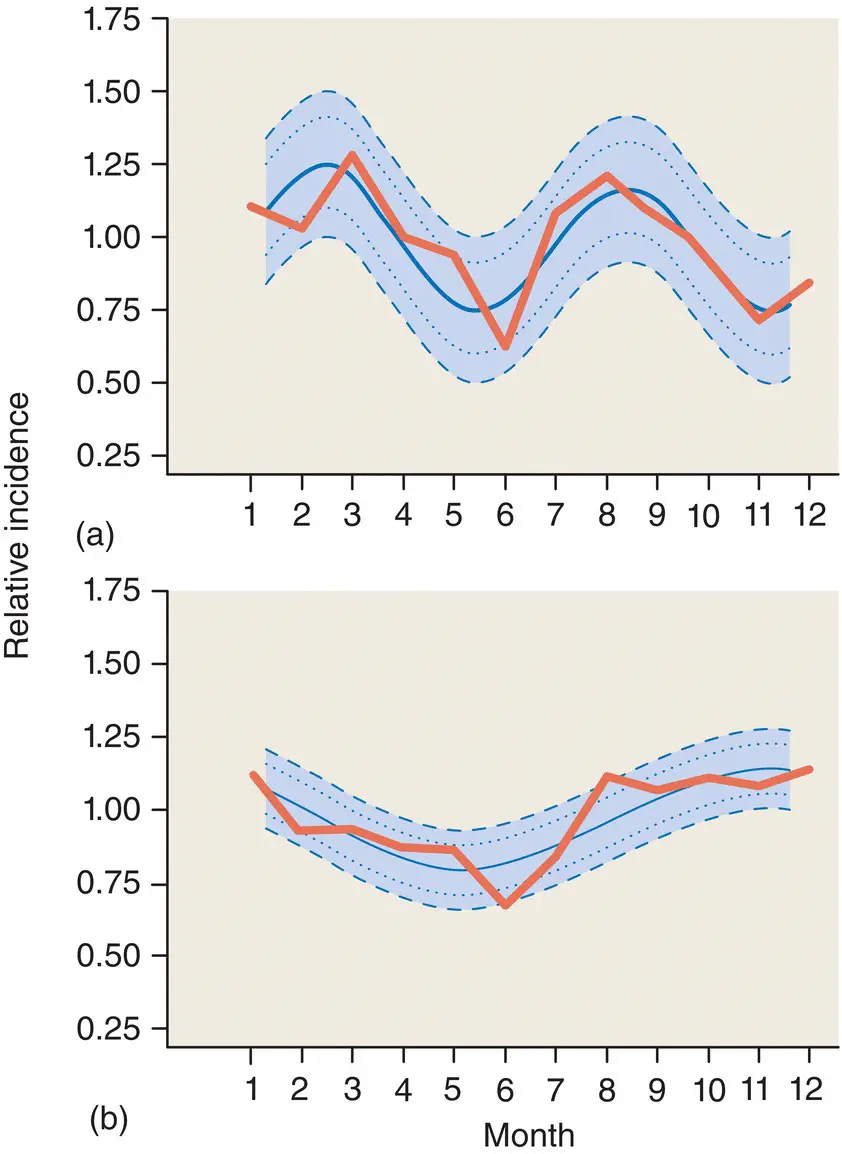
Evidence for environmental influences comes from studies that show a seasonal variation in the onset of type 1 diabetes in some populations, with the highest frequency in the colder autumn and winter months ( Figure 6.3). This is often thought to reflect seasonal exposure to viruses, but food or chemicals might also be involved. Moreover, people who have migrated from an area of low to an area of high incidence for type 1 diabetes seem to adopt the same level of risk as the population to which they move. For example, children of Asian families (from the Indian subcontinent and Tanzania) who moved to the UK traditionally have a low frequency of type 1 diabetes, but now have a rising incidence of the disease, which is approaching that of the background population.
Familial clustering of type 1 diabetes provides evidence for complex genetic factors in its aetiology. The lifetime risk for type 1 diabetes in monozygotic twins is >75%; for children with a mother with type 1 diabetes it is 1.3–4.0%; 6.0–9.0% if their father has type 1, and 15% if both have the condition (the background population risk is <0.4%). The reasons for the gender differences in inheritability and incidence are unknown. In (European) siblings of children with type 1 diabetes the lifetime risk is 6.0–7.0%, and this is much greater if they share the same human leucocyte antigen (HLA) DR3–DQ2 and DR4–DQ8 haplotype. However, only 10–15% of type 1 diabetes occurs in families with the disease (‘multiplex’) and most cases are said to be ‘sporadic’. The incidence has an equal gender distribution below age 10, thereafter there is a male preponderance although the reasons for these sex differences remain unknown.
Figure 6.2 Incidence rates (1999–2003) of type 1 diabetes in 0–14‐year‐olds in 17 European countries grouped into regions with roughly homogeneous rates. Purple 22.9–52.6/100,000; pink 22.4–29.8/100,000; orange 13–18.3/100,000; green 11.1–17.2/100,000; and blue 11.3–13.6/100,000.
Reproduced from Patterson et al. Lancet 2009; 373: 2027–2033).
Evidence for autoimmunity in the pathogenesis of type 1 diabetes originally came from postmortem studies in patients who have died shortly after presentation, and pancreatic biopsies from living patients. They have revealed a chronic inflammatory mononuclear cell infiltrate (‘insulitis’) ( Figure 6.4) associated with the residual β cells in the islets of recently diagnosed type 1 diabetic patients. The infiltrate consists of T cell lymphocytes and macrophages. Later in the disease, there is complete loss of β cells, while the other islet cell types (α, δ and PP cells) all survive. The discovery of islet cell antibodies confirmed the autoimmune basis of the inflammation ( Figure 6.5).
Since these original observations, four circulating autoantibodies have been found in people with newly diagnosed type 1 diabetes. They are antibodies to the insulin molecule (IAAs), tyrosine phosphatase (insulinoma antigen‐2 protein IA–2), zinc transporter 8 (ZnT8) and glutamic acid decarboxylase 65 (GAD 65). However, less than 10% of individuals with a single autoantibody go on to develop type 1 diabetes, although the proportion increases dramatically in those with two or more autoantibodies ( Figure 6.6). The sequence of appearance of autoantibodies differs, the first to appear is IAA (sometimes GAD65) at a median age of 15 (range 6–24) months in prospective studies in high risk children. The second antibody is usually detected within the next 2–4 years, following which the likelihood of developing multiple autoantibodies appears to decline. In first degree relatives of probands with type 1 diabetes, 75% of seroconversions occur before 13 years of age.
The lifetime risk of type 1 diabetes approaches 100% in genetically at‐risk children with two or more autoantibodies. The rate of progression to symptomatic disease in these children depends upon the number of autoantibodies (more = faster), the age of seroconversion (earlier = faster), and the type of antibody (IAA and IA–2 = earlier onset; IA–2 and ZnT8 = faster). In first degree relatives, 78% of those developing symptomatic type 1 diabetes have IA–2 and ZnT8 autoantibodies.
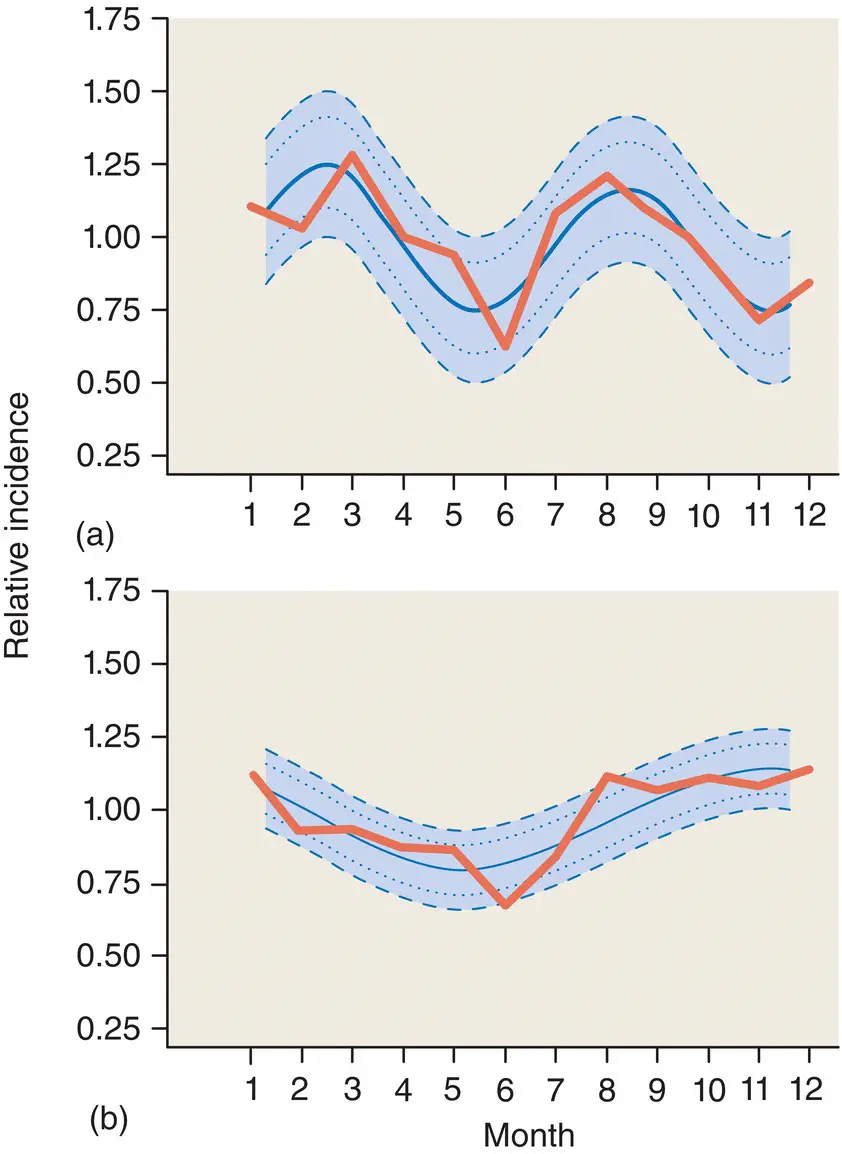
Figure 6.3 Seasonal variation of type 1 diabetes among Finnish children (a) 0–9 years of age, (b) 10–14 years of age during 1983–92. (The observed monthly variation in incidence is the solid line with dots.) The inner interval is the 95% confidence interval (CI) for the observed seasonal variation and the outer interval is the 95% CI for the estimated seasonal variation.
Читать дальше