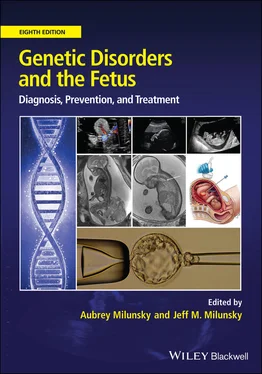
Genetic Disorders and the Fetus
Здесь есть возможность читать онлайн «Genetic Disorders and the Fetus» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Genetic Disorders and the Fetus
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Genetic Disorders and the Fetus: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Genetic Disorders and the Fetus»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Genetic Disorders and the Fetus — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Genetic Disorders and the Fetus», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Immune function
The placenta employs a number of mechanisms that protect the embryo/fetus from infection. Genes involved in immune regulation are among the most differentially expressed 30 , 31and differentially methylated 32in the placenta across different gestational ages. The human placenta is not only the source of hematopoiesis early in pregnancy, but remains a hematopoietic organ throughout gestation. 33 , 34The placenta also contains a large number of Hofbauer cells (placental macrophages), which may play roles in placental angiogenesis and prevent pathogens crossing from mother to fetus. 35Exosomes and microvesicles also appear to provide protection against viruses, which may be partially attributable to transmission of members of the chromosome 19 placenta‐specific paternally expressed microRNA cluster (C19MC). 36Understanding how the placenta protects from infection is an important question in the study of preterm birth (PTB). Chorioamnionitis (CA), or intra‐amniotic infection, an inflammation of the chorion and amnion usually caused by bacterial infection, is associated with the majority of extremely (<28 weeks) PTBs and about 16 percent of PTBs at 34 weeks. 37, 38Genetic variants that modify the maternal or fetal immune response have been linked to risk for PTB and/or PTL 39, 40possibly by disrupting cytokine balance (e.g. IL‐6 : IL‐10 ratio). 41
Placental insufficiency
Placental insufficiency is the situation whereby the placenta does not deliver an adequate supply of nutrients and oxygen to the growing fetus. It is associated with adverse pregnancy outcomes, including FGR, maternal PE, and PTB. Constitutional chromosomal abnormalities such as triploidy, trisomy 13, or trisomy 18 are commonly associated with placental insufficiency, but would normally be diagnosed through amniocentesis or fetal abnormalities detectable on ultrasound. The most common known genetic cause of FGR in an otherwise normally developed fetus with normal chromosomes at amniocentesis is confined placental mosaicism (CPM) (discussed further in “Developmental considerations in confined placental mosaicism”). Genomic imbalance (i.e. altered ratio of maternal and paternal haploid genomes) is also associated with a variety of adverse pregnancy outcomes. Epigenetic changes can be observed in placentas from complicated pregnancies, though these are more likely consequences than causes of placental pathology.
Fetal growth restriction
FGR, also referred to as intrauterine growth restriction (IUGR), is defined as poor fetal growth due to an underlying pathological cause. Although small for gestational age (SGA) (birthweight <10th percentile) is sometimes used as a surrogate for FGR, the majority of SGA fetuses are healthy. 42 , 43FGR represents 10–50 percent of SGA fetuses, with this proportion being dependent upon the population being studied and which growth curves are applied. 42 , 43Distinguishing FGR from a constitutionally small baby prenatally is important, as it is specifically the FGR baby that is at risk of adverse perinatal outcomes, including intrauterine death, premature birth, neonatal sepsis, and neurological impairment. 44 – 46Placental FGR is also a risk factor for adult‐onset diseases such as diabetes, hypertension, and cardiovascular disease. 47
To diagnose FGR prenatally, fetuses with abdominal circumference <10th percentile can be further assessed by uterine and umbilical artery Doppler to check for impeded blood flow to the placenta or fetus, amniotic fluid index, and other signs of fetal compromise (see Chapter 17). Altered protein levels in maternal serum have been associated with FGR caused by placental insufficiency, including lower levels of PlGF and increased levels of soluble fms‐like tyrosine kinase‐1 (sFLT‐1). 48 – 50Placentas associated with FGR tend to be small and are associated with a range of pathologies that may be a cause or consequence of impaired maternal or fetal vascular supply. 51These findings can include increased syncytial knots, intervillous fibrin deposition, villous infarcts, villous agglutination, distal villous hypoplasia, villous hypermaturation, marginal abruption, thrombosis, and chorangioma, among others. Compromised placental vascularization can also be seen as microvascular regression (particularly at the placenta periphery). 52However, such findings can occur in the absence of FGR, and further research is needed to clarify these relationships.
Genetic causes of fetal growth restriction
Many genetic conditions can be associated with FGR, but these are individually rare. The only relatively common known genetic cause of FGR is CPM, typically occurring as trisomy in some or most cells from the placenta, with a predominantly normal diploid fetus. CPM is present in approximately 10 percent of placentas associated with FGR pregnancies (after exclusion of constitutional chromosomal abnormalities). 53 – 56In the past, CPM was generally only diagnosed prenatally when chorionic villus sampling (CVS) was performed, with trisomy 16 being one of the most common trisomies involved when there is poor fetal growth. CPM can also be detected by noninvasive prenatal testing (NIPT), which is based on genetic analysis of DNA that is largely derived from the placental trophoblast and increasingly used routinely in prenatal assessment. 57 , 58
Although there is no identifiable placental pathology characteristic of placental (mosaic or nonmosaic) trisomy, certain features are more likely to be present. Placentas tend to be small, although fetal–placental weight ratio is often preserved. 59In early gestation, there may be trophoblastic irregularities reminiscent of hyperplasia, with a lacey appearance, and increased invaginations or inclusions of trophoblastic epithelium. 60In some cases of trisomy 16, ultrasound examination shows cystic changes, raising the clinical possibility of partial molar pregnancy but those changes are often not appreciated until after delivery of the placenta. 61Although not common, there are reports of other trisomies with a histological partial hydatidiform mole (PHM)‐like phenotype, including trisomies 7, 15, and 22. 62
The frequency with which CPM is identified as the explanation for FGR may be dependent on the criteria used to diagnose FGR and the prevalence of environmental risk factors for FGR (smoking, insufficient maternal nutrition, etc.) in the population. In addition, CPM would be considerably more likely when placental insufficiency occurs in the presence of older maternal age, a strong risk factor for trisomy. However, CPM and placental pathology can occur in the absence of IUGR, and further research is needed to clarify these relationships.
Amniocentesis for chromosome analysis in the second trimester may be recommended if fetal growth is discrepant for gestational age. Similarly, FGR detected in the third trimester would lead to serious consideration of an amniocentesis, since discovery, for example, of a trisomy, may well influence the mode and management of delivery. Chromosome analysis of the placenta at term may be warranted if there are concerns for the baby's development, especially if cord blood is not obtained. Placental mosaicism may be associated with fetal uniparental disomy or the trisomy may not be entirely confined to the placenta (i.e. low level fetal mosaicism can be present). For example, trisomy 7 in the placenta can be associated with fetal maternal uniparental disomy (UPD) 7, which can cause Silver–Russell syndrome (SRS), 63 , 64a condition characterized by severe FGR and dysmorphic facial features. If placental investigation is undertaken, it is important that specimens from multiple sites of the placenta are tested to diagnose the underlying mosaicism, as it is often present in only a subset of sampled sites. 53 , 65
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Genetic Disorders and the Fetus»
Представляем Вашему вниманию похожие книги на «Genetic Disorders and the Fetus» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Genetic Disorders and the Fetus» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.