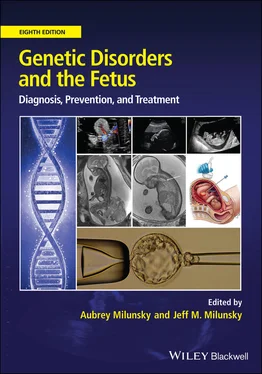
Genetic Disorders and the Fetus
Здесь есть возможность читать онлайн «Genetic Disorders and the Fetus» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Genetic Disorders and the Fetus
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Genetic Disorders and the Fetus: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Genetic Disorders and the Fetus»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Genetic Disorders and the Fetus — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Genetic Disorders and the Fetus», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
A frequent feature in the fetus from pregnancies affected by PMD, even in the absence of other fetal involvement, is the presence of hemangiomas. These may be benign skin hemangiomas, but in some cases hepatic hemangiomas are identified, as are hepatic mesenchymal hamartomas. These have been observed to be present in utero and may grow to an extent as to be life‐threatening to the fetus. 148 , 154 , 155Androgenetic chimerism can be found in some cases of liver hemangioma or hepatic mesenchymal hamartoma even in the absence of overt signs of PMD. 156Other cases of PMD have been reported to involve rearrangements of chromosome 19, which contains the C19MC imprinted, placenta‐specific microRNA cluster. 157Infantile hemangiomas may derive from placental mesenchymal cells that have invaded the fetus through the vascular system. 158 – 160
DNA methylation studies in the placenta and their clinical application
Epigenetic studies, such as analysis of genome‐wide DNA methylation, have aided our understanding of placental development and its unique nature. 161 , 162Relative to somatic cells, the placenta exhibits global hypo‐methylation, although this is not distributed randomly but mainly in distinct blocks along the chromosomes referred to as “partially methylated domains.” 161There is striking hypo‐methylation of some repetitive elements and the inactive X chromosome promoters in females, whereas average methylation at autosomal gene promoters does not differ. 163 , 164The distinct methylation of placental cells from somatic cells, such as blood, provides a means of distinguishing placental (fetal) from maternal cell‐free DNA in maternal blood for NIPT.
DNA methylation profiling can be used to characterize placental pathologies. For example, placentas associated with early‐onset PE exhibit widespread changes in DNA methylation. 98 , 165 – 169A subset of these changes overlap sites altered in syncytial trophoblast differentiation and hypoxia exposure; 165however, the relationship of the DNA methylation changes to the observed pathology is likely complex. Systematic changes in DNA methylation throughout gestation allow for methylation to be used as a gestational age “clock”. 170While this clock is largely robust to placental pathology, placentas associated with PE show evidence of acceleration of this clock, consistent with the phenotype of advanced villous maturation. DNA methylation profiling of placentas at delivery is useful to distinguish among different etiologies underlying PE 169and may be useful in the future development of new screening approaches.
Many imprinted DMRs are tightly maintained in placenta, and thus DNA methylation testing can be used for diagnosis of chromosomal imbalance in the placenta. For example, the parental origin of triploidy or the level of androgenetic cells in samples from placentas with PMD can be diagnosed from DNA methylation ratios at imprinting control regions. 171However, caution should be used in inferring imprinting defects in the fetus from evaluation of DNA methylation at imprinted DMRs in placenta. Some imprinted genes, such as CDKN1C and IGF2 , have placental specific promoters, 172 , 173and placental imprinted DMRs may differ from somatic ones for a given imprinted gene. Even for those that are maintained, some imprinting defects may arise post‐zygotically and the degree to which the placenta reflects imprinting status in the fetus has not been well established.
DNA methylation analysis is also typically used to evaluate X‐chromosome inactivation (XCI) skewing. It is important to note that XCI evaluation of the placenta cannot be used to infer skewed XCI in fetal tissues, as XCI occurs separately in these two lineages. 174In addition, the inactive X chromosome is incompletely methylated in the placenta and there are extensive site‐to‐site differences in XCI status due to the clonal manner in which villous trees grow, 174 , 175precluding use of a single site to infer XCI status of the placenta as a whole.
Epigenetic studies in the placenta and environment
The placenta exhibits a remarkable degree of developmental plasticity. 176By changing structure/cell composition, blood flow, or gene expression, the placenta may adapt to fetal demands for nutrients. 177Compensatory placental growth has been observed in response to reduced maternal nutrition in the first trimester of pregnancy. 178Placental size relative to the fetus is also affected by maternal smoking, 178 , 179psychosocial stress during pregnancy, 180 , 181and maternal iron levels early in pregnancy. 182Epigenomic analysis offers great promise in providing a record of the combined effects of a variety of in utero environmental exposures, as the epigenome (DNA methylation and histone modifications) can reflect both altered cell composition and changes to gene expression. 182Nonetheless, interpreting epigenomic studies of placenta faces many challenges. As placental size, shape, and function are associated with postnatal health of the baby into adulthood, there is great interest in overcoming these challenges to enhance our ability to assess the placenta to assist in the assessment of newborn health at birth.
The placenta as a predictor of child health
Increasing attention is being paid to the role of the placenta in predicting postnatal health outcomes (see Chapter 5), in particular related to neurodevelopment. 183For example, placental inflammatory lesions have been reported to be associated with autism spectrum disorder. 184 , 185Sex differences in brain volume, cortical thickness, and brain connectivity may arise in fetal development; 186links between genetic risk factors for schizophrenia and abnormal placental function have been suggested. 185 , 187It has also been suggested that genes and other factors linked to congenital heart disease may be connected to placental development, either because both share common regulatory pathways or because the dynamics of blood flow from the placenta plays an important role in heart development. 188Although the mechanisms linking prenatal events to childhood health are largely unknown, it seems plausible that examining molecular profiles and pathogenic markers in the placenta at delivery may be useful in predicting future risks for childhood and adult disease.
Further considerations
The placenta can be an important hallmark of fetal wellbeing in pregnancy. However, the placenta shows a remarkable degree of normal variability in size, shape, and gene expression. In particular, there may be areas of the placenta showing pathological features, while other areas appear normal. This makes evaluation of the placenta challenging, as the presence of abnormalities may not necessarily affect outcome if there is sufficient healthy placental tissue. A limitation to the use of placental evaluation is also simply a lack of attention paid to the placenta in research and clinical settings, which has impeded progress in utilizing this important resource. As appreciation for the placenta as an important component of fetal development grows, we are optimistic that we will learn to better extract the wealth of information it contains about the genetic makeup and environmental forces that have played a role in the development of the baby.
References
1 1. Bernischke K, Burton GJ, Baerge RN. Pathology of the human placenta, 6th edn. Berlin: Springer‐Verlag, 2012.
2 2. Barker D, Thornburg K. Placental programming of chronic diseases, cancer and lifespan: a review. Placenta 2013; 34:841.
3 3. Burton G, Fowden A. The placenta and developmental programming: balancing fetal nutrient demands with maternal resource allocation. Placenta 2012; 33:S23.
4 4. Haeussner E, Schmitz C, Von Koch F, et al. Birth weight correlates with size but not shape of the normal human placenta. Placenta 2013; 34:574.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Genetic Disorders and the Fetus»
Представляем Вашему вниманию похожие книги на «Genetic Disorders and the Fetus» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Genetic Disorders and the Fetus» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.