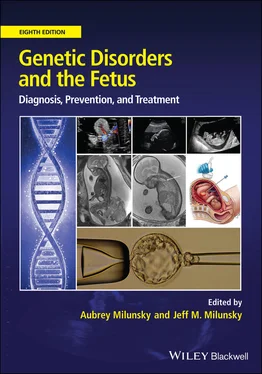
Genetic Disorders and the Fetus
Здесь есть возможность читать онлайн «Genetic Disorders and the Fetus» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Genetic Disorders and the Fetus
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Genetic Disorders and the Fetus: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Genetic Disorders and the Fetus»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Genetic Disorders and the Fetus — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Genetic Disorders and the Fetus», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Genetic linkage in large pedigrees segregating for PE has identified mutations in ACVR2A 120 , 121and STOX1 . 122 , 123These mutations appear though to be rare and found in only isolated pedigrees. BWS due to mutations in CDKN1C has also been linked with increased risk for PE. 124In addition, there is some evidence for contribution of genetic variants in several genes, including HLA genotypes and variants in FLT1 , to risk of PE. 125 , 126
Genetic findings associated with molar changes in the placenta
One of the most distinct placental phenotypes is that associated with a hydatidiform mole. Complete hydatidiform mole (CHM), PHM, and placental mesenchymal dysplasia (PMD) are related conditions that usually result from genomic imbalance involving an excess of paternal/maternal genomes ( Table 4.1). Pregnancy prognosis and management differ depending on diagnosis, as does recurrence risk. Importantly, PMD can be associated with a range of pregnancy outcomes, ranging from miscarriage/intrauterine death to healthy term birth.
Table 4.1 Genomic and chromosomal defects affecting placental function and fetal growth.
| Defect | Mechanism | Placenta/fetus |
|---|---|---|
| Digynic triploidy | Majority the result of errors in maternal second meiotic division (MII) | Very small placenta; no cystic change. Lacy trophoblastic with irregular villus contours. Asymmetric intrauterine growth restriction (IUGR) with associated adrenal hypoplasia. Fetal anomalies attributable to triploidy |
| Diandric triploidy | Fertilization of normal egg by two sperm (dispermy) | Large placenta with cystic villi. Cystic chorionic villi, focal trophoblastic hyperplasia – findings of partial hydatidiform mole. Fetal vasculature present, p57 staining positive (normal). May have symmetric IUGR. Fetal anomalies attributable to triploidy |
| Complete hydatidiform mole (CHM) | Fertilization of egg by two sperm with no contribution from the maternal pronucleus | Grossly evident cystic villi. Cystic chorionic villi, diffuse circumferential trophoblastic hyperplasia, ± cytologic atypia, stromal karyorrhexis. p57 staining negative (abnormal) |
| Androgenetic chimerism/mosaicism | Two cell populations: one normal, one androgenetic (paternal genome only) | Grossly, large placenta, large fetal vessels and associated Wharton's jelly extending into placental disc. Abnormal vessels extend into enlarged and myxomatous appearing stem villi. No trophoblastic hyperplasia. Beckwith–Wiedemann syndrome. Skin and hepatic hemangiomas. Hepatic mesenchymal hamartomas |
| Trisomy 13 | Generally maternal meiotic error | Small placental volume. Reduced fetal growth. Abnormal fetus. Increased risk of maternal preeclampsia |
| Trisomy 18 | Generally maternal meiotic error | Small placenta leading to reduced fetal growth. Fetal anomalies |
| Trisomy 21 | Generally maternal meiotic error | Normal size. Placenta shows deficiencies in the process of cytotrophoblast fusion leading to syncytiotrophoblast formation. Decreased risk of maternal preeclampsia |
| Confined placental mosaicism: trisomy 16 | Almost always maternal meiotic error | Cystic changes on ultrasound. Usually not grossly or histologically cystic. May show irregularities of trophoblast epithelium. Fetal growth restriction is common. Fetal anomalies may occur in a subset of cases |
Complete hydatidiform mole
CHMs are generally the result of androgenetic (paternal only) development and are observed in about 1/800 human pregnancies. 127Diagnosis is characterized by cystic, edematous chorionic villi (fluid accumulation within the placental villi), trophoblastic hyperplasia (overgrowth of the outer layer of the villi), and, generally, absent amnion, chorion, and fetal development ( Figure 4.1a, b). Pathological diagnosis is aided by absence of p57 KIP2staining, a protein expressed only from the maternal allele of the CDKN1C gene and, consequently, negative in CHMs. Most CHMs are diandric diploid with genomic contribution from either one or two sperm. 128The abnormal development of embryos lacking a maternal genome can be explained by loss of expression of developmentally important paternally imprinted (maternally expressed) genes. 129 , 130A small portion of CHMs are biparental in origin and these are more likely to be recurrent and familial. Maternal homozygous and compound mutations in NLRP7 have been detected in the majority of women experiencing recurrent biparental hydatidiform moles. 131 , 132Mutations in c6orf221 have also been reported. 133Biparental moles generally exhibit abnormal maternal imprints, although the extent of this and loci involved are variable. 134 – 136
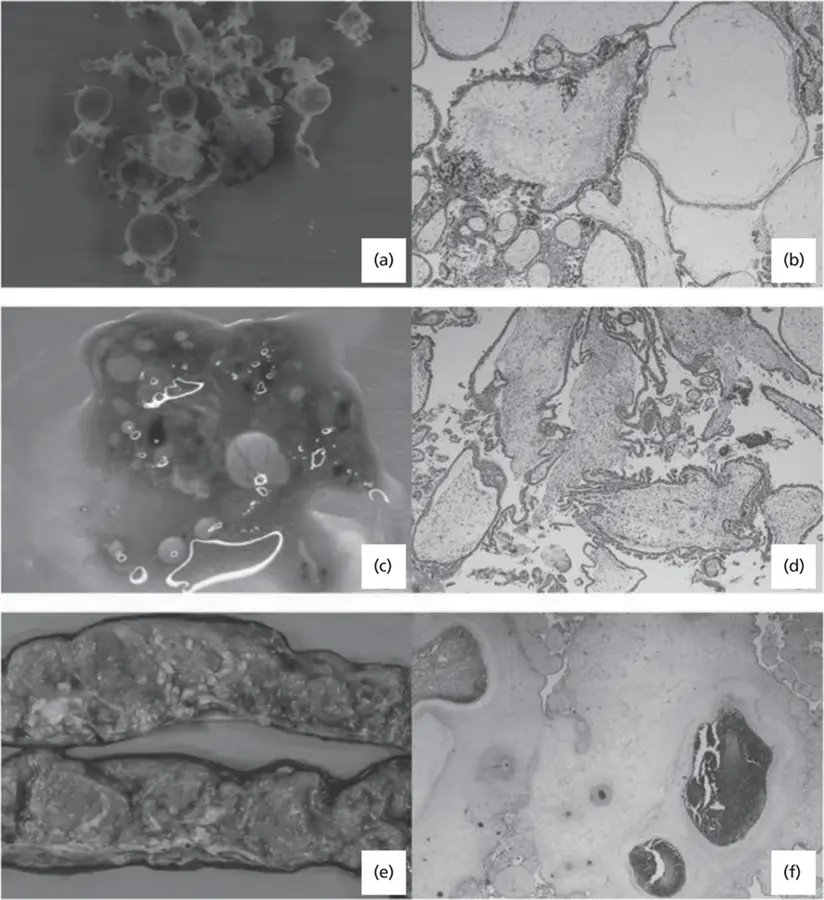
Figure 4.1 (a) Complete hydatidiform mole (CHM) gross – cystic villi; (b) CHM microscopic – cystic villi with cisterns, circumferential trophoblastic hyperplasia, stromal karyorrhexis; (c) partial hydatidiform mole (PHM) gross – cystic villi; (d) PHM microscopic – normal and cystic villi, focal trophoblastic hyperplasia, fetal vessels, and blood cells present; (e) placental mesenchymal dysplasia (PMD) gross – abnormal extension of vessels and Wharton's jelly into placenta parenchyma; (f) PMD micro – large, myxomatous stem villi with abnormal and dilated vessels.
Partial hydatidiform mole
PHM is the result of triploidy, but is present in only a subset of diandric triploid pregnancies. 137PHMs show some phenotypic overlap with CHMs on ultrasound assessment, but pathologically, exhibit a range of villi from normal to cystic villi with focal trophoblastic hyperplasia ( Figure 4.1c, d). 138Staining for p57 is preserved (normal). Although triploidy most commonly ends in miscarriage in the first trimester, PHM may be detected in a second‐trimester ultrasound where it presents as cystic placenta in association with an abnormally developed fetus, and may be associated with abnormal serum analytes (high hCG and α‐fetoprotein) 139 , 140and PE. 141Diagnosis may be confirmed with chromosome testing by CVS or amniocentesis.
Placental mesenchymal dysplasia
A rarer, but important, placental phenotype recognizable prenatally, is that of PMD ( Figure 4.1e, f). This can be misdiagnosed on ultrasound as a PHM and has been referred to as a “pseudo partial mole.” 142 – 146Placentas with PMD may appear on ultrasound as unusually large and thick with multiple echo‐poor regions representing edematous stem villi and possibly enlarged blood vessels. Remarkably, PMD can often coexist with a completely normal fetus; however, there is increased risk of FGR and fetal or neonatal death. PMD can be distinguished from a partial or complete mole on pathology examination as there is no trophoblast hyperplasia. PMD shows abnormal vessels in enlarged and myxomatous appearing stem villi. There may be some edematous chorionic villi but this is not usually a prominent feature. Whereas partial moles are triploid, PMD generally have a normal diploid karyotype, but molecularly can be shown to have a chimeric mix of androgenetic and biparental cells. 147 – 149In some cases, a CHM can grow closely adjacent to a twin placenta that is normal diploid and mimic the appearance of PMD on ultrasound.
Diagnosis of PMD has been associated with fetuses exhibiting features of BWS, including omphalocele, macroglossia, and visceromegaly. 143 , 145 , 146PMD associated with BWS generally results from mosaicism for maternal deletion, paternal duplication, or paternal UPD of chromosome 11p15.5, but appears to be a relatively rare finding among BWS cases as a whole. 150Additionally, androgenetic chimerism (often reported as mosaic “complete paternal uniparental disomy”) has been associated with BWS. 151 , 152In such cases, phenotype can be variable and there may be features of multiple imprinting disorders. 153
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Genetic Disorders and the Fetus»
Представляем Вашему вниманию похожие книги на «Genetic Disorders and the Fetus» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Genetic Disorders and the Fetus» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.