In this example, Equation (2.1)describes the two‐group clinical trial of this chapter but, as we will see in other chapters, we can extend this model to describe more complex clinical trial designs although this basic type of equation encapsulates the essential structure of all our analyses.
In essence, one purpose of any experiment is to estimate the parameters of a statistical model analogous to that of Equation (2.1). Thus, we conduct a trial in order to collect data with this purpose in mind. We would like to believe that the estimates we obtain in some way reflect the true or population parameter values. In principle, if we repeated the study many times, then we would anticipate that these estimates would form a distribution that is centred on the true parameter value. If this is the case, our method of estimation is unbiased . For example, in a clinical trial comparing two treatments, the parameter β Treatcorresponds to the true difference (if any) in efficacy between them, and the object of the trial is to obtain an unbiased estimate of this. The method of selecting which of the eligible patients is to be included in the trial does not affect this, but the way in which those patients who are recruited to the trial are then allocated to which particular treatment does. As we discussed in Chapter 1, of fundamental importance to the design of any clinical trial is the random allocation of subjects to the alternative treatments. Randomisation also provides a sound basis for the ensuing hypothesis testing by the use of statistical tests of significance.
When planning a clinical trial of whatever size or complexity, it is very important to establish the ground rules. Although many of these are common‐sense based, it is very useful to have access to clear guidelines for all stages of the process. Such guidelines have been published covering a wide range of topics ranging from regulatory requirements to what a statistical referee should look for when reviewing a clinical trial manuscript for publication.
We will refer to some of these guidelines at the relevant stages later in the book. However, readers are warned that many of these are constantly being updated and it is always useful to check if the ones referred to are the most current.
1 O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, Yardley L and Hoddinott P (2019). Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open, 9, e029954.
Fuller details are provided by www.mrc.ac.uk/complexinterventionguidanceor the European Medicines Agency, Spark building, Orlyplein 24, 1043 DP Amsterdam, The Netherlands, http://www.emea.eu.
1 ICH E9 (R1) (2018). Statistical Principles for Clinical Trials. CPMP/ICH/363/96.
This contains, for example, a clear statement of what distinguishes an ITT from a per‐protocol analysis.
1 ICH E10 (2001). Choice of Control Group in Clinical Trials. CPMP/ICH/364/96.
Contains information concerning what are regarded as suitable control groups in many situations.
CHAPTER 3 The Trial Protocol
It is a fundamental requirement to develop a formal protocol for any clinical trial and we describe in general terms the subject matter of such a protocol. The chapter focuses on the content common to all trial protocols such as the background to the trial, the basic design, the type and number potential subjects to recruit, informed consent, details of the intervention options, and other practicalities including the forms required for recording the data. We illustrate each section by extracts from activated protocols used for a variety of trials in different areas.
We also emphasise the need to check local regulations concerned with the conduct of trials and reference is made to some published guidelines to help in the protocol development process.
Day (2007) defines a protocol as:
A written document describing all the important details of how a study will be conducted. It will generally include details of the products being used, a rationale for the study, what procedures will be carried out on subjects in the study, how many subjects will be studied, the design of the study and how the data will be analysed.
In our context, ‘study’ is replaced by ‘trial’ and commonly ‘products’ will be replaced by ‘treatments’ or ‘interventions’. In particular, a clinical trial protocol is a document that will include sections addressing those design features we have highlighted in Chapter 2, as they relate to the specific trial in question.
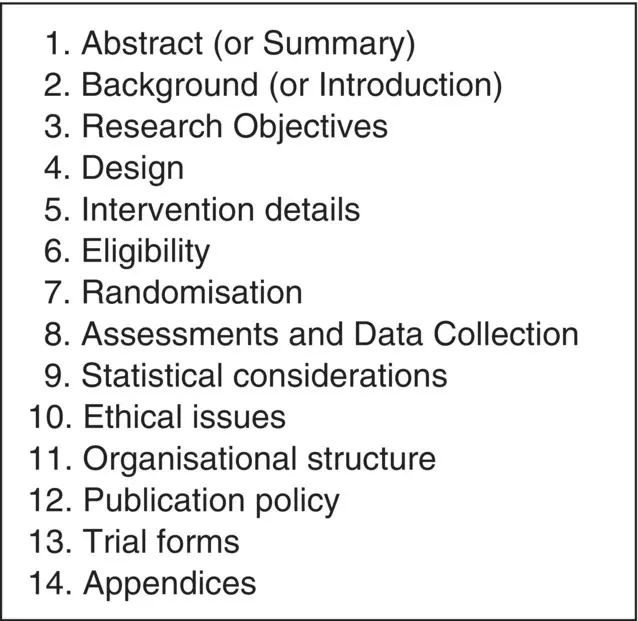
As we have pointed out, the questions posed in a clinical trial must be important and so it is vital that the research team identify all the scientific, clinical and practical elements, together with the resources and skills necessary in order to achieve clear answers. This is no small task even when embarking on a clinical trial of moderate size and complexity. A fundamental part of this process, and one that must be undertaken to obtain local and, if appropriate, regulatory approval, is the development of the associated trial protocol. This document must be clear yet concise and contain all the elements necessary for all the members of the investigating teams to carry out their respective tasks. Thus, for any clinical trial, although the main features of the trial from design to analysis will be discussed in detail at the planning stage, the trial itself cannot be conducted unless the finalised plan is thoroughly documented. In broad terms, the range of features to be addressed in the trial protocol is indicated in Figure 3.1although there may be additional requirements depending on the specifics of the actual trial to be undertaken, and the headings under which particular details fall will also vary with circumstance. For example, patient safety issues may be of paramount concern in one trial in which case this may warrant a dedicated section in the protocol. In others, this may not be the case so such issues may require only brief mention.
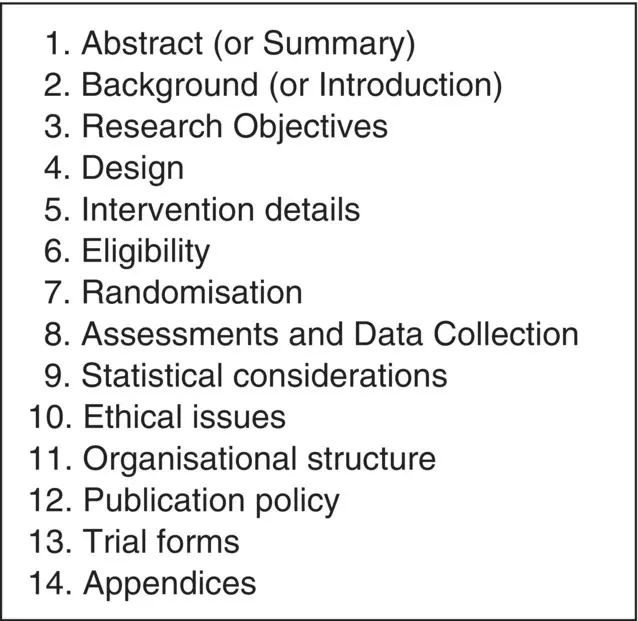
Figure 3.1Major components of a clinical trial protocol
It is very difficult for any one person to think of every detail of all the elements that are needed for a particular protocol and so it is important to involve as broad a team as one can (certainly to include members from a range of disciplines) in the development process.
Further, although this may be mandatory within many situations, a review of the document by two or more experienced but independent peers together with an independent statistician (and other experts as may be relevant) is also advisable. Such a group should also review the data forms, whether paper, electronic or in a web‐based format, to ensure they are clear and that they encapsulate the key features, do not overburden the clinical teams or trial subjects with unnecessary detail yet enable the trial endpoint(s) to be unambiguously recorded for each subject.
Finally, the protocol should be dated, suitably bound in book form, and any subsequent amendments carefully documented. In the following sections, we address the individual sections of a protocol as detailed in Figure 3.1and, wherever possible, give illustrative examples of how some of the sections have been phrased in activated protocols.
We cannot emphasise too strongly, that the protocol must be a high‐quality document, in both scientific and clinical terms, and needs to be written in clear language with careful highlighting of important issues. The protocol serves many purposes; for example, it gives an overview of the trial process from beginning to end, details the specific interventions, and how these are to be allocated. Importantly it guides the clinician through when and how assessments are to be made, and where necessary provides a step‐by‐step guide to administering the precise interventions stipulated.
Читать дальше